Hemodialysis
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
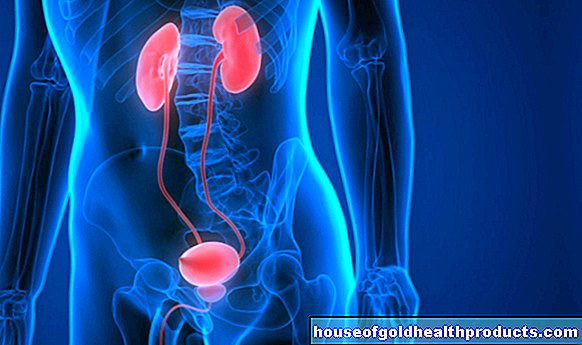
Hemodialysis is a blood washing procedure that is used in patients with kidney failure. It is used more often than peritoneal dialysis (abdominal dialysis). A device with a membrane filters and cleanses the blood outside the body. One also speaks of "artificial kidney". Hemodialysis usually takes place in a dialysis center. The supervisors are specially trained nursing staff and a team of doctors. Read more about hemodialysis.

What is hemodialysis?
With hemodialysis, the blood is sent outside the body through an artificial membrane to remove harmful substances. This membrane works like a filter, so it is only permeable to some of the substances.
Hemodialysis uses the physical principle of osmosis. If substances are present in a higher concentration on one side of the membrane than on the other side, then these migrate through the membrane until the substance concentration is equalized (osmosis). The blood has a different concentration of urinary substances and blood salts than the liquid in the dialyzer (dialysate). Therefore, these substances migrate from the blood into the dialysate.
Conversely, during hemodialysis, the patient's blood can be enriched with appropriate substances through a specific composition of the dialysate. So harmful substances are removed from the blood and desired substances are added again.
Dialysis shunt
During hemodialysis, a large amount of blood is regularly withdrawn from the body, cleaned and fed back into the body. However, regular punctures damage the blood vessels, the wall of which is usually thin and easily vulnerable in chronic kidney weakness. Therefore, dialysis patients receive a stable artificial vessel, more precisely: an artificially created short circuit between an artery and a vein. This so-called dialysis shunt (also Cimino shunt) is often placed on the patient's forearm under local anesthesia (regional anesthesia).
An artery and a vein are exposed and brought close to one another through a small incision on the wrist. They are then tied off briefly before the surgeon makes a small longitudinal incision in the vessel walls. The artery and vein are sewn together using these longitudinal incisions. Sometimes the artery and vein are connected to each other with a short plastic tube.
Because the blood flows in arteries at a higher pressure than in veins, the blood flows via the dialysis shunt into the vein with unusually high pressure. In adaptation to this, the vein expands over time and acquires a thicker wall. It can then be punctured repeatedly for dialysis. Dialysis is performed through a catheter until the wall of the vein is sufficiently thick. It is usually placed on the patient's neck.
A dialysis shunt usually has little effect on the patient. If a blood clot blocks the shunt, it can be removed with a minor surgical procedure. Any bottlenecks can also be removed surgically or expanded using a balloon catheter.
When is hemodialysis done?
Hemodialysis is used:
- for a few days in the event of acute kidney failure or poisoning.
- as a permanent therapy for chronic kidney failure (chronic kidney failure) in an advanced stage.
What do you do with hemodialysis?
During hemodialysis, blood is taken from the dialysis shunt and fed into the dialysis machine via a hose system. Here urinary substances and excess body water are removed from the blood and the blood salts (electrolytes) are balanced. The blood then returns to the body via the shunt. The whole process takes several hours.
The dialysis patients usually have to come to the treatment center three times a week for four to eight hours each time. Hemodialysis is therefore time-consuming - with all the restrictions that it entails for work and normal everyday life.
Hemodialysis as home dialysis
Hemodialysis is usually done in a dialysis center. However, after intensive training lasting several weeks, patients can also carry out the artificial blood wash at home. The patients receive continuous medical care. This includes having a kidney specialist available around the clock.
Hemodialysis as home dialysis requires a lot of personal responsibility from the patient, but offers him greater flexibility in terms of time than hemodialysis in a dialysis center. In addition, treatment complications (such as problems with the dialysis shunt) are much less common with home dialysis.
What are the risks of hemodialysis?
Since hemodialysis does not take place continuously, water and toxins regularly build up in the blood. Many substances that the body absorbs with food and drink are therefore not excreted. They have to be removed by dialysis. A hemodialysis patient must therefore adhere to a diet (see “Dialysis and nutrition”).
Medicines: Due to the weak kidneys, phosphate can accumulate in the body. The result can be an overactive parathyroid, followed by bone damage and arteriosclerosis. Dialysis patients must take phosphate-binding tablets with every meal. If the calcium level in the blood allows it, vitamin D is also given, as this is important for the absorption of calcium into the bones.
During hemodialysis there is a loss of water-soluble vitamins (especially B vitamins), which must be compensated for with medication.
What do I have to consider during hemodialysis?
Hemodialysis puts a strain on the body and restricts the patient in terms of timing and nutrition. But it is vital when the kidneys fail. Dialysis can often bridge the long waiting time for a new kidney (kidney transplant).
Many patients "hang" on dialysis for years. The duration and frequency of dialysis affects life expectancy and the occurrence of possible complications. The more hours per week and the more often the patients are dialyzed, the longer they live and the lower the late-stage damage. These include, for example, vascular calcification, heart disease or bone and joint damage.
However, such complications can be significantly reduced or delayed through optimal hemodialysis treatment. Therefore, high blood pressure, lipid metabolism disorders and anemia (renal anemia), which can arise as a result of chronic kidney failure, must be carefully treated.
Factors such as the age of the patient at the start of hemodialysis, their compliance and any additional illnesses also have an influence on life expectancy and possible late-stage damage.
Tags: diet sleep alcohol