Pacemaker
All content is checked by medical journalists.A pacemaker is an electrical clock generator. It is used to treat severe arrhythmias and to prevent sudden cardiac death. Read everything about pacemaker surgery and life with a pacemaker.

What is a pacemaker?
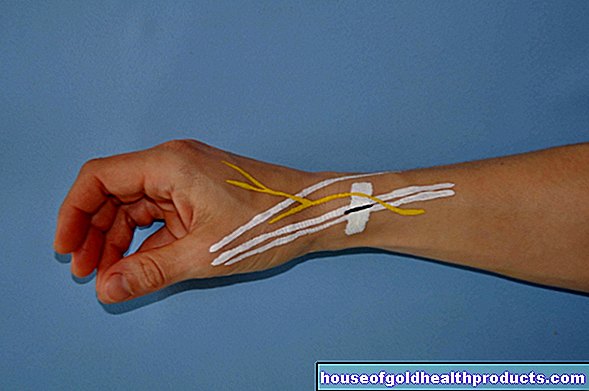
The pacemaker is a small device that helps a sick heart to beat in time again. It is placed below the collarbone, just under the skin or the pectoral muscle. Pacemakers are equipped with long wires, the electrodes, that extend through a large vein into the heart. There they measure the activity of the heart muscle.
The device itself (pacemaker with battery and pulse generator) recognizes the heart's action. Constant impulses are suppressed when the heart beats itself. The device can also stimulate the heart itself if necessary. To do this, the pacemaker sends an electrical impulse to the heart muscle via the electrodes, which then contracts.
With the help of a powerful pacemaker battery, which is mostly made of lithium, the devices last between five and 15 years, depending on the activity, before they have to be replaced.
When do you need a pacemaker?
According to the German Pacemaker Register, doctors in Germany implanted around 77,283 new pacemakers in 2017. The reason for this was mostly cardiac arrhythmia in which the heart beats too slowly (bradycardia). These include above all the so-called AV block, sick sinus syndrome, bundle branch block or bradyarrhythmic atrial fibrillation. In these diseases, the formation or conduction of electrical impulses in the heart muscle is slowed down or even fails completely, which is why the heart muscle contracts too seldom or does not work at all (cardiac arrest).
A heart attack, in which the conduction cells of the heart have been damaged, is a rarer indication for a pacemaker. A pacemaker is sometimes necessary even after bypass surgery or cardiac ablation. Sometimes doctors only need to use a pacemaker temporarily, for example in the event of a digitalis overdose.
What types of pacemakers are there?
Which pacemaker is implanted depends on the type of underlying disease. For example, if the sinus node, the heart's clock, does not work properly, single-chamber pacemakers are implanted. With these types, the probe reaches into the right ventricle of the heart and always emits an impulse when one's own excitement is absent. The pulse of the probe then triggers a heartbeat, which spreads in reverse in the direction of the atria.
Strictly speaking, a probe in the atrium would be sufficient. Since the patients often develop a conduction disorder in the AV node and would then need a probe in the ventricle, doctors usually place the probe in the ventricle and not in the atrium.
If the heart's cable system (the line from the sinus node to the heart muscles) is affected by a malfunction, pacemakers with two electrodes are used - one in the right atrium and one in the right ventricle.
If there is also cardiac insufficiency, pacemakers with three electrodes are used (so-called biventricular or CRT pacemakers). Here, too, the probes are located in the right atrium and the right ventricle, but an additional probe extends to the left side of the heart towards the main chamber. This allows the left and right ventricles to beat synchronously.
If over time it turns out that the type of cardiac arrhythmia has changed, the function of the implanted pacemaker can also be adjusted.
How do you perform a pacemaker operation?
The so-called pacemaker implantation does not normally take place under anesthesia. So the patient is awake during the operation. Before doctors use the pacemaker, the skin and underlying tissue are numbed. As a result, the patient usually does not feel any pain during the operation.
The surgeon then makes an incision, usually below the right collarbone. A large blood vessel runs here that leads directly to the heart. The doctor opens it and pushes the long, flexible tubes through the vein to the heart. To ensure the correct position, the chest is x-rayed several times during the pacemaker operation. In this way, the position of the probes can be checked and corrected if necessary.
The doctor then checks whether the electrodes correctly measure the heart's own electrical activity and whether the impulses sent by the pacemaker are arriving correctly. If everything works properly, the skin over the pacemaker is sealed.
What are the risks of the pacemaker?
Even if a pacemaker operation is a relatively safe procedure, complications cannot always be avoided. In almost every thirtieth pacemaker implantation, the probes are incorrectly positioned. The consequences can be functional limitations of the device, vascular injuries or cardiac arrhythmias. However, this complication is usually recognized and treated in the hospital.
If the patient suddenly has hiccups after a pacemaker operation, this indicates an unwanted electrical excitation of the diaphragm. A tingling sensation in the arm can also indicate that a probe is incorrectly positioned. Normally, you then have to perform a pacemaker operation again, in which the wires are positioned differently.
A bruise (hematoma) often forms in the area of the wound below the collarbone. As a rule, it does not have to be treated as it is gradually broken down by the body itself. Major bleeding may also occur as part of the procedure.
If the wound swells and reddens after a pacemaker operation, there may be a bacterial infection behind it.Then regular wound control and treatment by the doctor is important, especially if the patient develops a fever or feels weak and exhausted. Bacterial infections are treated with antibiotics.
Other possible complications are pacemaker-induced reentry tachycardia. The device incorrectly detects excitations that it has triggered itself. It then mistakenly sets other stimuli that lead to a racing heart.
Pacemaker syndrome can occur with a special type of pacemaker (VVI pacemaker). It manifests itself as low blood pressure, shortness of breath, dizziness and fainting spells.
What do you have to consider after a pacemaker implantation?
As a rule, patients perceive life with a pacemaker as completely normal. Most of the time, they are also much more efficient and resilient than before, as their heart now works much better. Nevertheless, you have to pay attention to a few things in everyday life:
After the pacemaker operation, you should avoid the wound for a few days during personal hygiene and make sure that the skin is not stretched, for example by lifting your arm too vigorously.
Immediately after the operation, the doctor will issue you a pacemaker card that you must always have with you. How often you have to have a pacemaker check-up depends on the underlying disease and the device used, which is why you make an individual appointment with a heart specialist.
Magnetic resonance imaging can
Living with a pacemaker
Shortly after the pacemaker operation, you should initially refrain from strenuous physical activity. On the one hand, the body still has to recover after the procedure, and on the other hand, it takes a few weeks for the device and the wires to grow firmly in place. In principle, however, you can do anything that is good for you.
As a pacemaker wearer, you must be careful when handling electrical devices. The electromagnetic fields emanating from these can interfere with the work of the pacemaker. Especially devices that contain strong magnets can cause problems. For example, people with older pacemakers are not allowed to have a magnetic resonance imaging (MRI) scan, as the strong magnet can interfere with the device and the metal in the pacemaker can heat up. In the meantime, however, there are pacemakers for which such an examination is unproblematic. Induction cookers that work with magnets can also cause problems in the kitchen. Please read the relevant information in the instructions for use.
Pay attention to electrical devices or systems as well as magnets at home, in your free time and at work! You can disturb the pacemaker function!
Cell phones, drills, cordless screwdrivers, toasters, hair dryers and other electrical devices can also cause interference. They express themselves, for example, in a feeling of dizziness or a noticeably irregular pulse rate. These disappear as soon as you switch off the device. As a rule, however, a safety distance of 15 to 30 centimeters is sufficient between the pacemaker and the device to be operated. If you are unsure which devices could interfere with your pacemaker, you should ask your heart specialist.
Tags: parasites drugs digital health