Artificial fertilization
Nicole Wendler holds a PhD in biology in the field of oncology and immunology. As a medical editor, author and proofreader, she works for various publishers, for whom she presents complex and extensive medical issues in a simple, concise and logical manner.
More about the experts All content is checked by medical journalists.For many childless couples, artificial insemination is a great opportunity to get pregnant despite a fertility disorder. Doctors support the sperm and egg cells on their way to each other. Which assisted reproductive technology (ART) is most suitable depends on the individual situation of the couple. Get an overview of the methods, chances of success and risks of artificial insemination here.

What is artificial insemination?
The term artificial insemination covers a number of fertility treatments. Reproductive medicine generally helps with assisted reproduction so that the egg cell and sperm can find each other more easily and fuse together successfully.
Artificial insemination: methods
There are three methods of artificial insemination:
- Semen transfer (insemination, intrauterine insemination, IUI)
- In Vitro Fertilization (IVF)
- Intracytoplasmic Sperm Injection (ICSI)
Except for the transfer of semen, artificial insemination takes place outside the female body. Thus, the sperm and egg cells must first be removed from the body and processed accordingly.
Further information
You can find out more about the process as well as the advantages and disadvantages of the individual methods in the articles Insemination, IUI, IVF and ICSI.
Cycle monitoring
In many cases, cycle monitoring takes place before artificial insemination. This means that doctors closely examine the processes in the female body for a menstrual cycle. For this, the woman usually has to appear for three to four ultrasound appointments and blood samples. On the one hand, cycle monitoring serves to track down the cause of unwanted childlessness. On the other hand, the findings help the doctor to find the right treatment for a couple (e.g. by means of hormone treatment).
How does artificial insemination work?
The process of artificial insemination depends on the organic causes of the infertility. Only after a precise diagnosis can the doctor decide which procedure is most suitable.
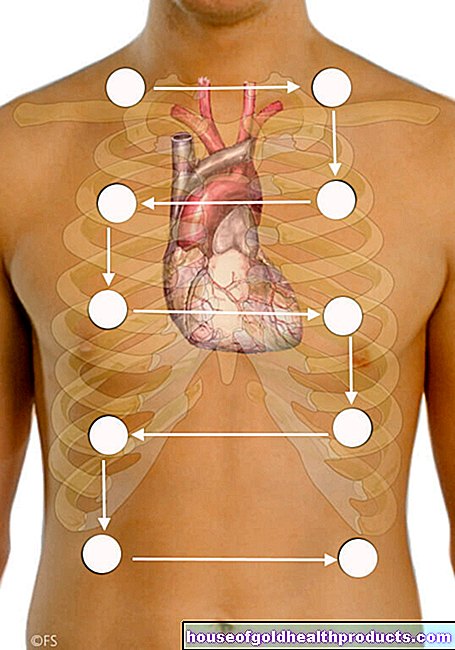
Even if every reproduction technique works a little differently in detail, the following steps can be distinguished in all of them:
Collection of sperm cells
To help with fertilization, doctors need sperm cells. The extraction or extraction can take place in different ways. Which of these is chosen in each individual case is decided by the individual case. In principle, the following are possible:
- masturbation
- surgical removal from the testicle (TESE, testicular sperm extraction)
- surgical removal from the epididymis (MESA, microsurgical epididymal sperm aspiration)
You can find out how sperm cells are extracted from the testes or epididymis in the article TESE and MESA.
Hormonal stimulation treatment
In order for egg cells to be mature for artificial insemination, the woman sometimes has to undergo hormone therapy. There are various methods (stimulation protocols) that can be considered here. After examining the ovaries and determining hormone levels, the doctor will select an appropriate protocol. During the treatment, he uses ultrasound and hormone analysis to check the growth and maturity of the follicles.
Important stimulation protocols are the short and the long protocol:
Short protocol
The short protocol takes about four weeks. From the second or third day of the cycle, the patient injects the stimulating hormone (FSH or hMG = human menopausal gonadotropin) under the skin on a daily basis. She can also ask her partner to give her the finished injection syringe. From about the sixth day of the stimulation cycle, the hormone GnRH (gonadotropin-releasing hormone) is also administered. It prevents spontaneous ovulation ("downregulation").
If the doctor determines during the check-up about ten days after the start of treatment that the follicles have matured well, he gives the woman the hormone hCG (human chorionic gonadotropin). It triggers ovulation. After 36 hours - shortly before ovulation - the follicles are removed by puncture.
Long protocol
The long protocol extends over six weeks. In the previous cycle between the 21st and 23rd day, the woman is injected with a GnRH agonist as a depot preparation. It inhibits the release of the body's own fertility hormones, which prevents spontaneous ovulation in the subsequent cycle ("downregulation"). After ten to 15 days, when the new cycle begins, the actual hormonal stimulation begins: As with the short protocol, it consists of daily injections of FSH or hMG. If enough follicles have matured after about nine to twelve days, the doctor triggers ovulation with an hCG injection. 36 hours later - shortly before ovulation - he removes the follicles.
Depending on the protocol, hormonal stimulation can also take place with tablets or with a combination of syringes and tablets.
Egg retrieval (more precisely: follicular puncture)
The following options for removing the egg cells or follicles are available:
- Removal of mature egg cells (follicle puncture after hormone treatment)
- Removal of immature egg cells (IVM, in-vitro maturation)
More information
You can find out how immature egg cells can be used in artificial insemination in the article In Vitro Maturation.
Embryo transfer
After artificial insemination outside the body (ICSI, IVF), the transfer of the fertilized egg cells into the uterus is the most important step on the way to pregnancy. If this happens within three days of fertilization, it is called an embryo transfer.
With a liberal interpretation of the Embryo Protection Act, it is possible to cultivate several fertilized egg cells. However, a maximum of two embryos may be transferred after a culture period of up to six days. Surplus embryos that are capable of development can be frozen (cryopreserved) and embryonic stages that are not capable of development can be discarded. However, there is no clear legal certainty for this widely practiced middle ground.
The best time for the transfer to take place varies from person to person.
Blastocyst transfer
If there are more egg cells available, it can make sense to wait a little longer. Thanks to the development of new nutrient solutions, the egg cells can continue to grow outside the female body for up to six days.
The cells divide after fertilization and the egg cells develop into blastomeres within the first three days, which then reach the blastocyst stage around the fifth day. Only 30 to 50 percent of all fertilized cells make it here. If the transfer takes place five to six days after fertilization, it is called a blastocyst transfer.
The chances that these cell structures implant themselves in the uterus are usually better than with an embryo transfer. Because the longer time outside the body, a deficient or faulty development can be recognized early, so that possibly unsuitable cell structures are not even used - i.e. inserted into the uterus. In a direct comparison of the pregnancy rates of embryo and blastocyst transfer, however, hardly any differences can be found.
Who is artificial insemination suitable for?
Artificial insemination helps couples with a fertility problem (men and / or women) and lesbian couples to have a child. Artificial insemination also offers cancer patients before chemotherapy or radiation therapy the chance of later wanting to have children.
Artificial insemination: requirement
In Europe, artificial insemination is best regulated for married heterosexual couples. In addition to a permanent partnership, a couple must meet other requirements, for example:
- clear medical indication
- Mandatory advice on artificial insemination (assisted reproductive technology, ART)
- HIV test
- Rubella and chickenpox vaccination
- Recommended: tests for toxoplasmosis, chlamydia, hepatitis
Artificial Insemination: Lesbian Couples
Some fertility centers and sperm banks in Germany and Austria enable homosexual women to have artificial insemination in the form of insemination. The prerequisite is that they are married and sign a treatment contract that stipulates maintenance payments and an adoption by the second mother. The couples are usually advised to use donor sperm from someone else's donor in order to exclude any legal claims later. In principle, however, fertilization is also possible with a sample from a private donor. In Switzerland, homosexual couples are denied the possibility of artificial insemination.
Artificial Insemination: Single Women
For anonymous sperm donation, a permanent partnership, ideally with a marriage certificate, is mandatory in Germany, Austria and Switzerland. Women without a partner have little chance of artificial insemination - single women who want to have children in this country will find it difficult to find a doctor or a sperm bank for artificial insemination. The reason are legal gray areas. For single women from Germany, Austria and Switzerland, countries like Denmark, where anonymous sperm donation is allowed, are therefore attractive. Or they try a so-called self or home insemination.
Artificial Insemination: Chances of Success
In vitro fertilization does not work with all couples. Sometimes it is a rocky road with failed attempts, setbacks, psychological and physical stress. Some couples hold their dream child in their arms at some point, while with others, artificial insemination reaches its limits.
The chances decrease with the age of the woman
In vitro fertilization works best in women up to 35. After that, the pregnancy rate drops rapidly and goes to zero in women over 45. The reason for this is the quality of the egg cells, which decreases with age. The older the woman, the higher the risk of miscarriages and deformities. If the trend towards starting a family at a later date continues and egg donation remains prohibited, freezing one's own egg and sperm cells at a young age (social freezing) could become more important.
additional Information
You can find out more about freezing egg cells at a young age and why the method has not yet established itself in some countries in the article Social Freezing.
Artificial Insemination: Opportunities by Method
Whether artificial insemination is successful depends on various factors - in addition to individual parameters such as the type of fertility disorder, age and psychological stress, this also includes the method used. The birth rate per treatment cycle can only be roughly estimated for each technique and varies between 10 and at best 20 percent depending on the method.
Guidelines: Artificial insemination in Germany, Austria and Switzerland
If pregnancy does not occur after several attempts at fertilization, it is depressing and difficult for the couple to accept. But medicine, too, sometimes has its limits - physically, methodically and legally. Not everything that is technically possible is also allowed in Germany, Austria and Switzerland.
Legal regulations (e.g. Embryo Protection Act in Germany) stipulate which methods and interventions the doctor may carry out in these countries. This is to avoid commercial and unethical use. According to the law, an embryo is a fertilized, viable egg cell. Pregnancy with a surrogate mother, spouse deceased with sperm and gender selection for sperm (except for severe genetic hereditary diseases) are not permitted for artificial insemination in Germany, Austria and Switzerland. In Austria, pregnancy with foreign egg cells (egg donation) is permitted under certain conditions (e.g. age limit for motherhood), but not in Germany and Switzerland.
Advantages and disadvantages of artificial insemination
There are various risks and complications associated with artificial insemination. The following problems can arise:
- Overstimulation syndrome
- bacterial infection
- Injury to the bladder, intestines and blood vessels from puncture
- Multiple pregnancies: Couples must be clear - twins are rare with artificial insemination, as two embryos are usually used. In addition, twins often have premature and caesarean births.
- slightly increased rate of miscarriages (mostly due to the higher age of the women)
- mental stress
In spite of all the risks and complications, artificial insemination naturally offers a great advantage - the chance to fulfill the desire to have children despite a fertility disorder, cancer or homosexual partnership.
Tags: womenshealth organ systems unfulfilled wish to have children