Allergic asthma
Tanja Unterberger studied journalism and communication science in Vienna. In 2015 she started her work as a medical editor at in Austria. In addition to writing specialist texts, magazine articles and news, the journalist also has experience in podcasting and video production.
More about the experts All content is checked by medical journalists.Allergic asthma (also allergic bronchial asthma) is a chronic lung disease that is triggered by contact with various allergens. Allergic asthma is the most common form of bronchial asthma and leads to severe coughing, shortness of breath and sudden shortness of breath in those affected. Read more about the treatment, triggers and symptoms of the disease here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. J45J46
![]()
Brief overview
- Treatment: Avoid contact with allergenic substances; Well treatable with medication (e.g. asthma spray, allergy immunotherapy).
- Prognosis: Currently, allergic asthma cannot be cured, but those affected can positively influence the course of the disease themselves.
- Symptoms: Typical symptoms are coughing, shortness of breath and sudden shortness of breath.
- Causes: Is particularly often triggered by pollen, house dust mite excrement, allergens from the fur of pets or mold spores.
- Risk factors: Certain factors (e.g. genes, secondhand smoke, excessive hygiene) promote the development of the disease.
- Frequency: Allergic asthma is usually more common within the family. 25 to 40 percent of all patients with untreated pollen allergy develop allergic asthma.
- Diagnostics: The doctor makes the diagnosis through a physical examination and a lung function test, among other things.
What can you do about allergic asthma?
People with allergic asthma are often less productive. This has a negative effect on everyday life and professional life. The aim of the treatment is therefore to relieve those affected from their complaints and to make them physically fit again. In the treatment of allergic asthma, in addition to medication (e.g. asthma spray), a changed lifestyle is in the foreground: By learning to deal with the triggers of the allergy, they improve their quality of life themselves.
Treatment without medication
Medication-free measures are just as important in the treatment of allergic asthma as medication therapy. The following is therefore recommended for those affected:
Avoid triggering cause
For people with allergic asthma, the first thing to do is to find out what factors and situations are causing or worsening the symptoms. Doctors advise those affected to avoid these triggers as much as possible. Of course, this is easier said than done in everyday life. However, there are a few ways to protect yourself against the triggering allergens to a certain extent:
House dust mites: If you are allergic to house dust mites, you can use a mite-proof mattress cover. Wash the bed linen regularly at a temperature of at least 60 degrees Celsius. Do not use "dust catchers" such as carpets, thick curtains or furs in the home or soft toys in your child's bed. Try to avoid increased humidity (over 50 percent) and temperatures over 22 degrees Celsius in rooms. Regular ventilation helps.
Molds: Molds occur wherever it is damp, for example on and around potted plants. Avoid doing this if you suspect that you are allergic to mold. Here, too, it is advisable to ventilate regularly and to keep the humidity low; this is especially true for the bathroom. It is best to avoid using a humidifier.
Pollen: With the help of a pollen calendar you can find out when and where which pollen is on the move - avoid these regions or times as much as possible. If there is a particularly high amount of pollen, shower and wash your hair every day before bed. Avoid storing clothes that have pollen on them in the bedroom. Also, do not hang laundry outside to dry. Some models of so-called electric pollen filters have also proven to be effective, which use a fan to guide the room air through a set of very fine-pored filters and thus can significantly reduce the number of pollen.
Medications: Certain medications, such as beta-blockers, used to treat heart disease can increase the risk of an asthma attack. Some pain relievers (e.g. with the active ingredients acetylsalicylic acid or ibuprofen) can also worsen the symptoms in asthmatics. Therefore, speak to your doctor if you are taking any new medication. If necessary, he will prescribe a different active ingredient for you if you need the medication. For example, asthmatics usually tolerate the pain reliever paracetamol very well.
Adjust lifestyle
People with allergic asthma can do a lot themselves to contribute to the success of the therapy and thus improve their quality of life.
This includes, among other things:
- Go to the pulmonologist regularly to have the course of the disease checked.
- Make sure that you receive an individual, written therapy plan that also includes an emergency plan (e.g. what to do in the event of an acute asthma attack?).
- Pay attention to the correct and regular use of the medication and the therapy plan.
- Take part in an asthma training course in which you learn, for example, how to use the medication correctly, how to use the therapy plan or how to behave in an emergency.
- If you run out of medication, get a new prescription in good time.
- Make sure that the environment is smoke-free. This not only applies to asthma patients themselves, but especially to parents whose children are affected by asthma! Secondhand smoke is a powerful and dangerous trigger for asthma attacks and can negatively affect the course of the disease in children with asthma.
Diet for allergic asthma
Asthmatics who consciously eat a lot of fruit, vegetables and whole grain products often have fewer symptoms and a higher quality of life. Much meat, sugar, and salt, on the other hand, can worsen the symptoms. Incidentally, those who eat a balanced and healthy diet also lower the risk of developing asthma in the first place.
Home Remedies & Homeopathy
Some home remedies can aid treatment. They can help alleviate the symptoms of allergic asthma, but they are never a substitute for a doctor's visit. These include:
- Turmeric as a tea, spice or drop is said to have a mild anti-inflammatory effect.
- Ginger as a tea or extract is said to protect against inflammation and strengthen the immune system.
- Magnesium (e.g. in the form of effervescent tablets or capsules) relaxes the muscles of the bronchi.
- Medicinal herbs such as Icelandic moss, fennel and ribwort in the form of lozenges or extracts make breathing easier and have an expectorant effect.
Essential oils such as peppermint, menthol or eucalyptus oil are not suitable for asthmatics. They can irritate the mucous membranes and cause shortness of breath.
Remedies from homeopathy such as Lobelia Inflata, Kalium iodatum or Natrum sulfuricum can also be tried in addition to the therapy. The use of acupuncture (laser acupuncture) to improve symptoms of asthma and allergies can also help some sufferers. However, there is only weak evidence of its effectiveness in a few applications.
Allergic asthma belongs in the hands of a doctor! The effects of home remedies and homeopathic remedies have not been clearly proven by studies. Those affected should therefore only use them to support the treatment of asthma.
Medication
When treating allergic asthma with medication, a distinction is made between long-term and reliever medication.
Long-term drugs
Long-term medications are the foundation of any asthma treatment. They counteract the triggering cause of the asthma. The most important active ingredients in this group are corticosteroids (cortisone), which are similar to the endogenous hormone cortisol. They prevent the bronchi from reacting too vigorously to certain stimuli and inhibit inflammation. This improves lung function, prevents acute breathing difficulties and alleviates or prevents typical symptoms.
In asthma therapy, the doctor almost always prescribes cortisone in the form of sprays or inhalation powders, as it gets directly to the place where it has to work. If cortisone is inhaled, the dose in the lungs is high enough, but in the entire body it is considerably lower than with cortisone tablets. Side effects are therefore less common. However, inhaled cortisone takes one to two weeks to develop its full effect, and the effect is only maintained through constant use.
For this reason, those affected are advised to continue therapy with cortisone sprays even if they are currently not experiencing any symptoms. This does not apply to treatment with cortisone tablets. These can increase the risk of serious side effects and secondary diseases (e.g. diabetes, osteoporosis), especially if taken continuously.
If cortisone alone is not enough to control the symptoms, the doctor will combine it with other active ingredients. These include certain active ingredients from the group of long-acting beta-2 sympathomimetics or leukotriene antagonists. Beta-2 sympathomimetics stimulate part of the nervous system called the sympathetic nervous system. This causes the affected person's bronchi to dilate. Leukotriene antagonists slow down the inflammation in the bronchi.
Medication if needed
The doctor uses reliever medication in the event of acute worsening of the allergic asthma and in an emergency. The drugs most frequently used for this are short-acting beta-2 sympathomimetics (e.g. in the form of sprays), which those affected also inhale. They widen the bronchi within minutes and so relieve asthma symptoms quickly.
In severe allergic asthma that does not respond to the usual therapy, the doctor may give the active ingredient omalizumab. This is a laboratory-made antibody that interrupts the allergic reaction in the body. In order to specifically interrupt the allergic reaction, the doctor injects the drug directly under the skin.
Those affected receive the drug when the total IgE level (IgE is an antibody that is largely responsible for allergic reactions in the body) in the blood remains high despite treatment (therapy with cortisone spray and beta-2 sympathomimetics) continue to have symptoms.
Allergen-specific immunotherapy (AIT or desensitization)
If the trigger of the allergic asthma is a pollen or house dust mite allergy, allergen-specific immunotherapy (AIT or desensitization) is recommended. It directly fights the cause of allergic asthma. The principle is as follows: If you give the body a small dose of the allergen at regular intervals and increase it slowly, the immune system gets used to it and the symptoms decrease.
There are two options for allergen-specific immunotherapy: Either the doctor gives injections under the skin, or the patient takes drops or tablets. Whether and, if so, which of the two treatments is possible, is decided by the doctor on a case-by-case basis.
Allergen-specific immunotherapy cannot replace existing asthma therapy, it can only complement it.
Asthma control according to the step-by-step scheme
Asthma treatment with medication is always based on the severity of the disease. The symptoms of asthma can vary in severity. The doctor therefore checks the course of the disease regularly in consultation with the patient and adjusts the therapy if necessary. The basic principle is: as much as necessary and as little as possible.
A step-by-step scheme serves as a guideline, with the help of which doctor and patient adapt the treatment to the current severity. Each therapy level corresponds to a certain combination of medication, there are five levels in total.
Depending on the degree of asthma control, the doctor adjusts the treatment to the respective therapy level. The "degree of asthma control" results from different parameters (e.g. frequency of symptoms, lung function of the person affected, etc.)
In addition, the doctor often uses questionnaires with which he can better assess the disease (example question: How often have you suffered from shortness of breath in the last 4 weeks?). This instrument helps the doctor to better assess the person's asthma control.
The degree of asthma control is divided into:
- controlled asthma
- partially controlled asthma
- uncontrolled asthma
The aim is to bring the symptoms under control so that seizures occur as rarely as possible and those affected live with almost no restrictions.The control of asthma prevents acute worsening of the disease (so-called exacerbations) and improves the quality of life of those affected many times over. Regular control and adjustment of treatment plays a key role, especially with children, so that they can develop in a physically and mentally healthy manner.
Treatment of allergic asthma in children
Adults and children are generally treated according to the same principles, the dosage and administration of the medication, however, is determined by the attending physician according to the age and physical development of the child. The level scheme for treating children with asthma also differs somewhat from that for adults.
Bronchial asthma due to an allergy?
In allergic asthma, allergens such as pollen or animal hair trigger bronchial asthma. The immune system inadvertently classifies these actually harmless substances as dangerous and reacts with an excessive defense reaction. In addition to other substances, the body releases excessive amounts of histamine and thus triggers the typical allergy symptoms, such as:
- allergic rhinitis (rhinitis)
- allergic conjunctivitis (conjunctivitis)
- allergic bronchial asthma with spasms of the bronchial muscles and inflammation of the mucous membranes
Asthma or COPD?
Like COPD (chronic obstructive pulmonary disease), allergic asthma is a chronic lung disease. Since sufferers often have similar symptoms, it is easy to confuse the diseases. In order to choose the right therapy, it is therefore important that a doctor examines the symptoms in detail. For example, breathlessness occurs in attacks in people with asthma, while COPD patients primarily have breathing problems during physical exertion. Asthmatics are also more likely to have a dry cough. People with COPD have a pronounced cough with thick sputum that occurs mainly in the morning.
COPD patients often have little response to treatment with asthma sprays.
Who gets allergic asthma?
Allergic asthma usually occurs more frequently within the family and in many cases begins in childhood or adolescence. But it can also only develop in the course of life. An estimated 10 percent of children and 5 percent of adults are affected by bronchial asthma.
If an existing allergy is not treated or not treated sufficiently, the disease worsens: Around 25 to 40 percent of all patients with untreated pollen allergy develop allergic asthma in the course of their lives. In such cases one speaks of a "floor change". This means that the allergic reaction travels from above, from the mucous membranes, down into the bronchi. Sometimes this happens unnoticed.
Allergic asthma in children
50 to 70 percent of all asthma illnesses in children and young children are triggered by an allergy. In some cases, allergy-related asthma disappears during puberty but can reappear in adulthood. The more severe asthma is in childhood, the more likely it is for people to suffer from it as adults.
In addition to the typical symptoms such as cough, shortness of breath and tightness in the chest, children with asthma often also have a fever. Since asthma can affect the child's development, parents are advised to consult a doctor at the first sign.
If the disease is recognized early and treated consistently, asthma in children can be cured.
Can you cure allergic asthma?
Despite intensive research, asthma cannot yet be cured. The symptoms usually persist for a long time and only subside temporarily, if at all. In most cases, however, the disease can be treated well with medication. A well-treated asthmatic has the same life expectancy as a healthy person. With proper treatment, the disease will develop favorably in the long run as well.
What are the symptoms of allergic asthma?
Regardless of the cause, the bronchial tubes of the person affected change in asthma (air ducts that guide the air): The airways narrow and cause the typical asthma symptoms.
This includes:
- Cough (mostly dry)
- wheezing (wheezing)
- Chest tightness
- shortness of breath
- Shortness of breath
- Chest pain
Typically, the symptoms are not permanent, but rather seizure - often in the early morning. In principle, coughing fits can also occur at night. This is because the bronchi also have a day-night rhythm and they are less dilated during the night. People also often find it harder to breathe out, and their breathing is accompanied by wheezing. Sometimes they have a cough, sometimes in the form of coughing fits. In severe cases, an acute asthma attack occurs, in which the affected person can hardly breathe or no longer breathe.
If you have an asthma attack, keep calm, inhale your emergency asthma spray, and take a position that makes it easier for you to breathe. If your symptoms do not improve quickly, call the emergency doctor!
What causes allergic asthma?
In people with asthma, the airways are chronically inflamed. At the same time, the bronchial tubes of those affected are over-sensitive (bronchial hyperreactivity) to stimuli such as smoke or cold air in winter. These two factors lead to a narrowing of the bronchi (airway obstruction), which in turn triggers the typical symptoms of asthma.
Bronchial asthma can be allergic and non-allergic; mixed forms occur in many adults.
What triggers are there?
The triggers for allergic asthma include:
- Tree pollen: hazel, alder, birch, ash
- Grass, plantain, nettle, mugwort, ragweed pollen
- House dust mite allergens (feces and tanks)
- Animal hair (e.g. cat, dog, horse, guinea pig, rat, ...)
- Mold spores (e.g. Alternaria, Cladosporium, Penicillium, ...)
- Occupational allergens (e.g. flours, isocyanates in color varnish, papain in the manufacture of textiles)
Asthma that is triggered by pollen is called seasonal asthma, as the symptoms mainly occur during the pollen season. Year-round complaints occur with all other triggers, especially house dust mite and animal hair allergies.
What are the risk factors for allergic asthma?
Why some people develop allergies and - associated with this - allergic asthma has not yet been clearly clarified. Doctors suspect certain risk factors that favor the occurrence of an allergy or allergic asthma:
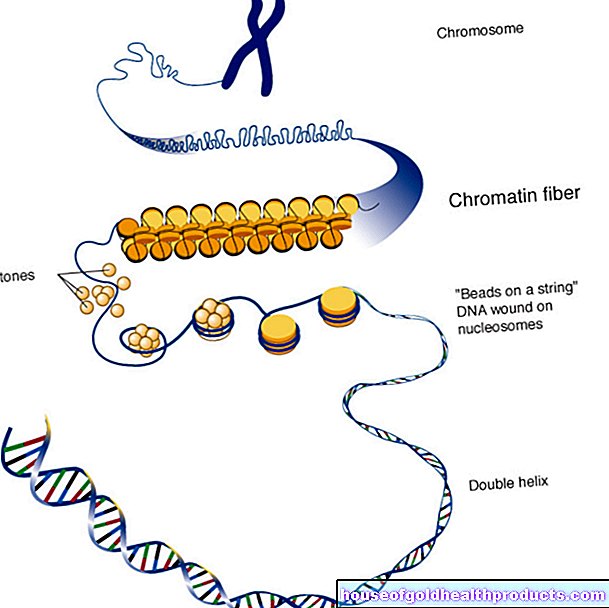
Genes
Hereditary predisposition plays a major role in allergic asthma. Children whose parents have allergic asthma have a higher risk of asthma than children whose parents are not affected.
External influences
Environmental factors also influence the development of allergic asthma. Children whose mothers smoke during pregnancy, for example, have an increased risk of developing allergies (e.g. hay fever, allergic asthma) later. The same applies to children who are regularly exposed to secondhand smoke. They are also more likely to develop allergies and allergic asthma than children who grow up smoke-free.
Excessive hygiene
Scientists discuss excessive hygiene in childhood as another possible risk factor for the development of allergies. They assume that the immune system gradually learns to deal appropriately with pathogens and harmless substances (such as animal hair) when exposed to them. With excessive hygiene, these stimuli are largely absent. As a result, the immune system remains underdeveloped.
Viral infections in childhood
In addition, viral infections (e.g. bronchiolitis, respiratory infections with chlamydia and rhinoviruses) in early childhood increase the risk of the disease.
How does the doctor make a diagnosis?
The most important diagnostic tools for allergic asthma are a detailed discussion (anamnesis), a physical examination and measuring the lung function (peak flow measurement; spirometry).
Talk to the doctor
If you suspect allergic asthma, your family doctor is your first point of contact. If necessary and for further examinations, he will refer you to a specialist in lung diseases (e.g. pulmonologist / pulmonologist; also allergist). Thanks to detailed examinations, the doctor can usually make the correct diagnosis quickly. To this end, he has a detailed discussion with the patient at the beginning, which often provides important information about the type of illness. The doctor asks the following questions, among others:
- When, how often and in which situations / in which environment do you have a cough / shortness of breath?
- Are there any allergic diseases within the family (e.g. neurodermatitis, pollen allergy, ...)?
- Are there animals in the household or in the immediate vicinity?
- Do the complaints occur seasonally or all year round?
- What do you do for a living?
Physical exam and pulmonary function test
This is followed by a physical examination and a pulmonary function test (spirometry). The patient blows into the mouthpiece of a device that measures the force and speed of the breath. In this way, the lung function, which is usually reduced by asthma, can be determined.
Here, three measured values are particularly important:
- Vital capacity (VC): the highest possible capacity of the lungs
- Second Capacity (FEV1): the amount of air that is exhaled in one second
- FEV1 / VC: the ratio of seconds capacity to vital capacity
If the FEV1 / VC ratio is less than 70 percent, the bronchi are narrowed. In asthma, the values for FEV1 and VC are usually below the norm, in severe asthma even very clearly. If only the small airways - less than 2 mm in diameter - are narrowed, one speaks of a "small airways disease".
Reversibility test
The doctor finally confirms the suspected diagnosis of “allergic asthma” by means of a so-called reversibility test. The patient inhales a drug that dilates the bronchi. After ten minutes, another lung function test is carried out: If the FEV1 is more than 12 percent or 200 ml higher than before the drug was taken, the diagnosis “reversible airway obstruction” is confirmed.
The narrowing of the airways has been significantly improved by treatment with a bronchodilator agent. People with asthma typically respond positively to bronchodilator substances, but this is not the case with COPD.
Allergy test
The doctor uses an allergy test to determine the exact trigger - the allergen. For the so-called "prick test", the doctor applies the most common allergens (e.g. cat, house dust mite excrement, grass or birch pollen) in liquid form to the skin of the person affected, then slightly scratches the skin ("prick"). If the patient has an allergy to a certain substance, skin wheals will appear on the affected skin area after about 20 minutes (allergic reaction).
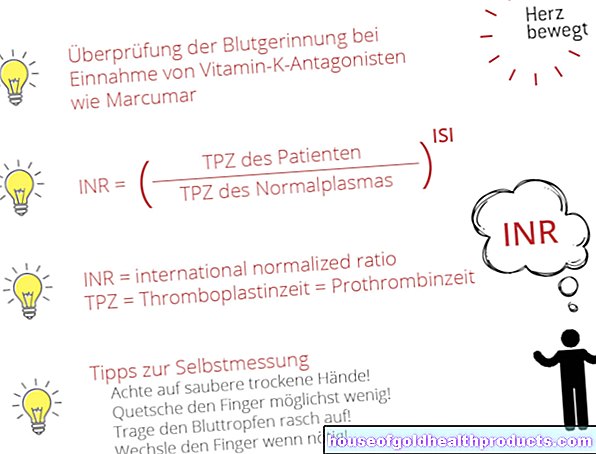
Blood test
A blood test gives the doctor further information on whether there is an allergy. Three values are determined:
- Total IgE: Elevated values indicate an allergy.
- Specific IgE: indicates which specific allergen the IgE antibodies are directed against
- Eosinophils / ECP: certain white blood cells that are usually more common in allergic diseases