Balanitis
Clemens Gödel is a freelancer for the medical team.
More about the experts All content is checked by medical journalists.Balanitis is inflammation of the glans penis, the tip of the penis. In the great majority of cases it also affects the foreskin and is then referred to as balanoposthitis. Those affected usually notice a distinct, painful reddening or change in the glans. Balanitis can have infectious and non-infectious causes and can usually be treated well. Find out here about symptoms, diagnosis and therapy of balanitis!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. N48
Balanitis: description
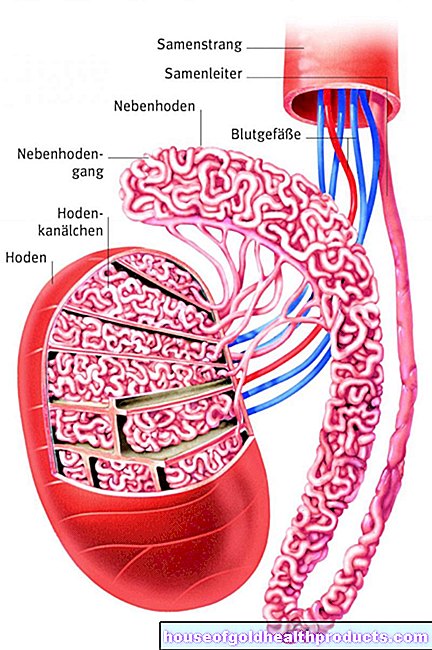
Balanitis is inflammation of the glans of the penis. Glans penis is the name given to the thickening at the end of the penis. It is a very sensitive part of the male body as it is endowed with many sensitive nerves. In uncircumcised men, the glans is covered by the foreskin. When an erection occurs, the foreskin usually retracts behind the glans. The inner sheet of the foreskin rests directly on the glans, so that inflammation at the glans very often spreads to the foreskin. This is known as balanoposthitis. Recurring and long-lasting episodes of glans inflammation are possible.
Balanitis occurs most frequently in uncircumcised men and is almost equally common in all age groups. Depending on the age, however, the frequency of the various causes of glans inflammation varies. Overall, it is estimated that between three and eleven percent of men develop balanitis each year. However, most studies only looked at children and sexually active men.
Balanitis: symptoms
The main symptom of balanitis is a more or less painfully red and inflamed glans. Usually only the upper layers of the skin are inflamed and not the deep cavernous bodies of the glans. Those affected often report rashes and unclear changes to the glans. An itchy glans is also a common symptom.
As a rule, affected men also suffer from discharge from the penis. This discharge can be of different colors and smelly. The consistency is often purulent. Pulling back the foreskin is usually difficult and painful. This can also be due to the fact that the glans swell (edema). This can make urination problematic and painful. In severe cases, the control of the urine stream can also be disturbed. Sometimes balanitis is even associated with impotence, even if only temporarily.
In most cases the glans inflammation is limited to the penis. Systemic signs of inflammation such as fever, malaise or vomiting are atypical in balanitis. With some pre-existing conditions, however, balanitis can also cause severe systemic reactions. This applies in particular to existing diseases that impair the immune system. Deep damage to the skin of the glans, including bleeding, occurs only in advanced, severe disease.
Indications of the cause of balanitis
In addition, there are a number of signs of balanitis that already indicate a possible trigger. Some are listed here as examples:
- When infected with the herpes virus, a large number of grouped vesicles form. The infection is usually accompanied by a fever and swelling of the inguinal lymph nodes.
- Human papillomavirus (HPV) infection causes condylomas - cauliflower-like growths that are often found at the base of the glans penis.
- The syphilis infection results in a painful ulcer with a hard edge.
- Raised redness or whitish discoloration with itching are indications of a fungal infection.
- The balanitis in the context of Reiter's syndrome shows itself by redness, which is delimited by a white border, as well as by skin damage on the glans.
- The zoon plasmacellular balanitis is a chronic inflammation of the glans of unknown cause. It is characterized by smooth, lacquer-like and red-brown areas.
Balanitis: causes and risk factors
There are a variety of causes that can be responsible for balanitis. Often there is also a combination of several causes. Mechanical irritation can lead to infection. In a third of all patients, no clear cause of the glans inflammation can be determined.
The causes of balanitis can be roughly divided into non-infectious and infectious causes. In addition, the glans inflammation can occur in the context of other diseases.
Non-infectious causes of balanitis
A common cause of inflammation of the glans is insufficient or excessive cleaning ("cleanliness balanitis"). If there is insufficient hygiene, the remaining smegma accumulates - a yellowish-white mass of sebum secretion, skin cells and bacteria). This can lead to balanitis.
Even high mechanical and chemical stress - for example from disinfectants and excessive washing - can provoke balanitis.
In some cases, balanitis is also the result of irritation or an allergic reaction to medication, fragrances or (latex) condoms.
Infectious causes of balanitis
The two most common causes of balanitis are believed to be fungal and bacterial infections.
Bacterial causes of balanitis include infections with staphylococci, enterococci, streptococci and also with Mycobacterium tubercolosis, the causative agent of tuberculosis. The bacterium Gardnerella vaginalis can also lead to balanitis. This germ is a common cause of bacterial vaginosis in women (vaginal inflammation). Men can become infected with the bacterium in sick women and develop balanitis.
Balanitis caused by fungi is also known as candidomycetic balanitis. Like bacterial infections, fungal infections can either only show up locally or systemically (i.e. also in the rest of the body).
Candida albicans, a yeast fungus, is the most common pathogen causing balanitis candidomycetika. Although the yeast Candida albicans can be detected on the glans in around 15 percent of men, only a small proportion of them develop balanitis. Uncircumcised men are more likely to get fungal balanitis than circumcised men. In most cases, the fungus is transmitted through sexual contact.
Another fungal infection, namely Malassezia furfur, is pityriasis versicolor (bran fungus). This form of skin fungus is very rare in Europe, but common in tropical areas. It particularly affects the back, shoulders, neck and chest, and sometimes other parts of the body such as the penis. This fungal infection is characterized by sharply demarcated, brownish and flaky lesions.
Other fungal infections spread to the penis even less often. Above all, fungi that get stuck in the groin can continuously spread to the penis.
The inflammation of the glans penis also occurs in the context of sexually transmitted diseases. Particularly noteworthy here are infections with herpes viruses and human papillomaviruses (HPV) - especially types 6 and 11. HPV in particular leads to protracted balanitis that are not easy to defeat.
Other possible triggers are trichomonads, gonococci, Treponema pallidum (pathogen of syphilis) and Haemophilus ducreyi.
Balanitis in the context of other diseases
Various skin diseases can relieve balanitis, but can also trigger it. These include pemphigus vulgaris, seborrheic dermatitis and psoriasis.
Lichen sclerosus et atrophicancs should also be mentioned here. The chronic skin disease of unknown cause causes typical white plaques on the foreskin and glans. This form of glans inflammation is known as balanitis xerotica obliterans. As the disease progresses, scars form and the foreskin becomes thin. The scars narrow the foreskin. The disease can spread to the urethra.
As part of Reiter's disease, a non-infectious inflammation, around a quarter of those affected develop balanitis. This disease is characterized by the three symptoms of joint inflammation, urethritis and conjunctivitis. It usually occurs one to four weeks after a urinary tract or gastrointestinal infection.
Zoon plasmacellular balanitis occurs in older men between the ages of 50 and 80. The cause of this form of glansitis is unclear. There is small bleeding and deposits of hemosiderin, an iron storage protein. In addition, immune cells infiltrate the tissue of the glans.
Inflammation of connective tissue cords can rarely lead to tissue death and thus trigger dangerous gangrenous balanitis. It requires emergency treatment.
Balanitis as part of cancer treatment
The so-called BCG instillation in the treatment of bladder carcinoma can rarely lead to granulomatous balanitis. BCG is the abbreviation for a type of bacteria. To prevent bladder cancer from relapsing, the urinary bladder can be flushed with weakened BCG bacteria. The bacteria trigger local inflammation that activates the immune system.This should inhibit the further development of cancer cells.
Risk factors for balanitis
The main risk factor for balanitis is poor intimate hygiene. It is important to wash the penis, and in particular the glans, daily with warm water and remove smegma. Failure to clean - but also too aggressive cleaning - can promote the development of balanitis.
A narrowed foreskin that is difficult to retract (phimosis) also promotes balanitis. This is because pathogens can attach themselves to the glans and spread more easily. Because of this, circumcision appears to reduce the risk of balanitis significantly.
Statistically speaking, people with certain diseases have balanitis more often than otherwise healthy people. This is especially true with diabetes mellitus. Presumably, the sugar in the urine of diabetics promotes the development of balanitis. Diabetic patients often have a fungal infection as the cause of balanitis.
Serious obesity and the chronic inflammatory bowel diseases Crohn's disease and ulcerative colitis are also seen as risk factors for glans inflammation.
Balanitis: examinations and diagnosis
Men should see a urologist if they suspect glans are infected. At the beginning of the balanitis diagnosis there is a detailed discussion with the patient to collect the medical history (anamnesis). The doctor asks, for example:
- How intensively do you practice intimate hygiene?
- Have you noticed any changes to the glans or penis?
- Are you suffering from pain or itching?
- Are you having problems urinating or having sexual intercourse?
- Are you known to have any skin or other diseases?
As part of the physical exam, the lymph nodes, especially those in the groin, and the glans should be examined. Even when looking at the glans penis, the doctor usually notices redness and swelling. In addition, discoloration of different colors is often observed. The foreskin should also be examined carefully. Often they too are affected by the inflammation. The doctor will also watch out for any narrowing of the foreskin.
As already described under the symptoms, many causes of balanitis can be determined by typical, visible changes in the glans, such as grouped blisters in a herpes infection.
If infectious balanitis is suspected, a swab should be taken from the glans penis and the urethral entrance to determine the pathogen. This smear can be examined under the microscope - possibly with the help of special stains. Fungi can be identified particularly well with a potassium hydroxide stain. In addition to a smear, it can be considered to start a culture in order to cultivate existing pathogens and thus to be able to better identify them.
In very rare cases, the blood of balanitis patients can also be tested for the pathogen or antibodies against the pathogen. This can be useful for certain types of mushrooms. However, the blood test is usually reserved for unclear and severe cases.
A small sample of tissue (biopsy) is considered for unclear and complicated balanitis. In the case of infectious balanitis, however, the findings of a biopsy are usually unspecific. In uncertain cases, a biopsy can mainly be used to investigate a suspected tumor or skin disease. Namely, there are a number of diseases that are similar to balanitis or are a complicated form of balanitis. These include a certain precancerous stage (erythroplasia Queyrat), penile carcinoma, the autoimmune vascular disease Behcet's disease and infection- or drug-induced rash (Steven-Johnson syndrome).
If there are problems urinating, the doctor will examine the urethral outlet for signs of inflammation. He asks the patient whether the foreskin "inflates" when urinating. If there is any indication that the urinary tract is involved, the doctor will also do an ultrasound examination of the bladder. Thereby an obstruction of the urine flow can be excluded or confirmed.
It is also possible that balanitis was triggered by multiple causes at the same time. This always also means that further investigations should be carried out even after a supposedly established cause. A wart caused by the human papillomavirus can also be covered by another infection.
Warning signs of a complicated course of balanitis are:
- Signs of blood poisoning (sepsis)
- a poorly controlled diabetes
- Inability to pull back the foreskin
- Blockages when urinating
Balanitis: treatment
The therapy of glans inflammation depends on various factors: the cause of the inflammation, the glans findings and the general condition of the patient. The basis of every balanitis therapy is good and appropriate intimate hygiene. This includes daily washing of the genital area with warm water and also good drying. Chamomile hip baths can be used to support the therapy. In almost all infections, the partner should also be treated, even if they have not yet shown any symptoms.
Local balanitis treatment is usually sufficient
In the case of an infectious glans inflammation, local (external) balanitis therapy is usually sufficient. An ointment with the antibiotic metronidazole is usually prescribed against bacteria. It has a very broad spectrum of activity. Cotrimazole, which is effective against a large number of fungi, is mostly used against fungi. This is usually enough to defeat the infection. If no success can be seen after four weeks of anti-fungal therapy, the diagnosis should be reconsidered.
In the case of balanitis of a non-infectious nature, local cortisone therapy with an ointment is usually tried first. Cortisone dampens the inflammation and thus usually significantly improves the symptoms. It should be noted, however, that the symptoms of cancer (precursors) can also improve under cortisone, but reappear after discontinuing the ointment.
If cortisone doesn't help, an ointment containing pimecrolimus, a stronger drug to calm the immune system, can also be used.
Systemic balanitis therapy with tablets
In certain situations, however, the medication must be taken as a tablet. This applies, for example, to diabetes mellitus (diabetes), severe alcoholism, chemotherapy, AIDS and prolonged use of cortisone. In addition, an increased risk of the infection recurring must be expected in these cases.
surgery
Circumcision can be considered in the case of repeated balanitis and a narrowed foreskin. The foreskin of the penis is surgically removed. Circumcised men tend to be less susceptible to infection. Surgical intervention is often performed to prevent narrowing of the urethra, particularly in the case of lichen sclerosus.
Balanitis therapy in children
There are special therapy recommendations for children that must be observed. The parents or the child themselves should consistently carry out intimate hygiene every day with the foreskin pulled back and, if necessary, apply an ointment containing cortisone twice a day.
If the foreskin is narrowed, it should only be pushed back in consultation with the attending physician, if at all. This can be very painful and uncomfortable. For this reason, the use of local anesthesia with an ointment or the administration of painkillers (possibly also locally) can be considered.
Balanitis: disease course and prognosis
In the vast majority of cases, the balanitis treatment is permanently successful. If the therapy does not work, the choice of medication can be adjusted to better combat the glans inflammation.
Untreated balanitis can rise along the urinary tract. Possible consequences are a urinary tract infection, bladder or prostate inflammation. Urinary tract infections are rare in men and must be treated more consistently than in women.
If the balanitis does not improve despite proper therapy, this can be an indication of a malignant process. In this case, a biopsy should be done. In most cases it is then a Queyrat erythroplasia.
Cancer precursors are rarely caused by chronic inflammation of the glans.
Infectious balanitis in particular should be observed in particular in patients with a weakened immune system. On the one hand, it is easily possible for the infection to spread and affect other parts of the body. On the other hand, balanitis can also be the first sign of an infection in the body. In addition, infections with a weakened immune system can take a much more severe course than in healthy people and lead to severe skin damage with bleeding. Persistent fungal balanitis can lead to a painful inflammation of blood-draining vessels.
In rare cases, a narrowing of the foreskin (phimosis) can result from balanitis.
Tags: toadstool poison plants eyes alternative medicine