Diabetic retinopathy
and Martina Feichter, medical editor and biologistDr. med. Julia Schwarz is a freelance writer in the medical department.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Diabetic retinopathy is a secondary disease of diabetes (diabetes mellitus). In those affected, the high blood sugar has damaged the retina, so that the eyesight deteriorates. Some patients even go blind.Diabetics should have their eyes checked regularly so that retinal damage can be detected early. Read more about diabetic retinopathy!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. E11E10E13O24H36E12E14
Diabetic retinopathy: description
Diabetic retinopathy (diabetic retinal disease) means damage to the retina in the eye due to high blood sugar levels. It can occur in both type 1 and type 2 diabetes.
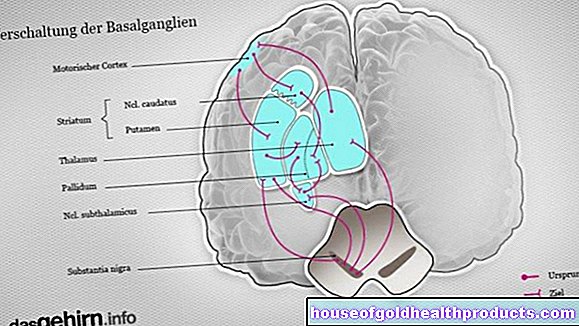
The retina consists of specialized nerve cells (photoreceptors) that convert the light rays falling into the eye into nerve impulses. High blood sugar levels damage the small blood vessels in the retina so that the photoreceptors receive too little oxygen. In advanced stages, new but unstable blood vessels form in the retina. Those affected see increasingly poorer vision and in severe cases can even go blind. Diabetic retinopathy is the most common cause of middle-aged blindness in developed countries.
Doctors differentiate between two different stages of disease in diabetes-related neuralgia: The initial stage is non-proliferative diabetic retinopathy. Years later, this can turn into proliferative diabetic retinopathy, with the risk of blindness. In addition to these two stages, there is a special form of the disease in which the retina is damaged, especially in the area of the macula (yellow spot, point of sharpest vision): diabetic maculopathy.
Non-proliferative diabetic retinopathy
“Non-proliferative” means that no new retinal vessels are formed at this stage of the disease. But even now the tissue in the eye is insufficiently supplied with blood, so that the retinal cells receive too little oxygen.
This reduced blood flow triggers typical structural changes in the retina, which the ophthalmologist can see when examining the fundus. At this stage, the patient himself often does not notice his illness. Only some patients report loss of visual field (from bleeding in the retina) and gradual deterioration in vision.
Proliferative diabetic retinopathy
In the advanced stages of diabetic retinopathy, the body tries to compensate for the marked lack of oxygen in the retina by forming new blood vessels in the vitreous humor. However, these are very unstable and tend to tear or burst. The result is frequent bleeding and fluid accumulation in the retina. Such new vessels also form in the iris (rubeosis iridis) and around the point where the optic nerve joins the retina (optic nerve papilla).
Proliferative diabetic retinopathy poses a serious threat to patients' eyesight. Most of the time, eyesight is already severely impaired. At this stage, however, there is a risk of complete blindness.
Diabetic maculopathy
Diabetic maculopathy is a special form of diabetic retinopathy. The place of sharpest vision (macula) in the area of the retina is particularly affected by the permanently increased blood sugar level. Fluid builds up in the tissue. Patients therefore have great difficulties in everyday life, for example when driving or reading.
Diabetic retinopathy: symptoms
As a result of the damage to the nerve cells in the retina, eyesight becomes increasingly poor. That dragged on for a few years. The damage often progresses slowly, especially in the first few years of the disease, but can accelerate later. It is usually noticed late by those affected.
In addition, diabetic retinopathy can also cause acute symptoms: if a retinal vessel ruptures and bleeding occurs in the retina, dark spots can suddenly appear in the field of vision. If the bleeding is excessive, the blood can also enter the vitreous humor of the eye and cause what is known as vitreous hemorrhage. Those affected see black dots flowing by ("soot rain").
In addition, diabetic retinopathy can cause retinal detachment (ablatio retinae) at an advanced stage. This is noticeable, for example, through flashes of light and sudden loss of visual field.
Diabetic retinopathy: causes and risk factors
Diabetic retinopathy is caused by permanently high blood sugar levels. The worse the blood sugar level, the more likely it is that diabetic retinopathy will develop.
In those affected, the many sugar molecules in the blood damage the inner walls of the smallest blood vessels (capillaries). This damage is also called microangiopathy. It affects all the tiny vessels in the body, but especially the retinal vessels and the kidney vessels.
If the nerve cells of the retina are no longer adequately supplied with blood and oxygen due to the vascular damage, they die. In addition, the damaged capillaries can leak. The resulting blood leakage also damages the nerve cells of the retina.
In addition to increased blood sugar, other risk factors also contribute to damage to the small vessels in the eye. This includes:
- high blood pressure (arterial hypertension)
- smoking
- increased cholesterol (and other fat levels in the blood)
- hormonal changes, for example during puberty or pregnancy
Diabetic retinopathy: examinations and diagnosis
The diagnosis of "diabetic retinopathy" is usually made by the ophthalmologist. Usually, he or she first conducts a detailed discussion with you as the patient in order to collect your medical history (anamnesis). Describe your symptoms to the ophthalmologist in detail. The doctor often asks questions such as:
- How long have you been suffering from diabetes?
- Have you seen a lot of blurred vision recently?
- Do you sometimes see black dots that seem to fly by?
- Do you suffer from high blood pressure?
- Do you smoke?
- Are you known to have high blood lipids or high cholesterol levels?
Fundoscopy is the most important examination for diagnosing diabetic retinopathy. The doctor looks at the fundus, which is completely painless for the patient.
In diabetic retinopathy, the damaged blood vessels can be visible in the fundus, depending on the stage of the disease. In addition, vascular sacs (aneurysms), retinal hemorrhages, retinal infarcts (“cotton wool foci”) and deposits of fats in the retina (“hard exudates”) can be seen.
Further investigations
Sometimes further examinations are necessary to clarify diabetic retinopathy more precisely. This includes, for example, a color examination of the retinal vessels (fluorescence angiography): A fluorescent substance is injected as a contrast agent to visualize the vessels. Optical coherence tomography (OCT) can also be used to examine the location of sharpest vision (macula) in more detail.
Diabetic retinopathy: treatment
Diabetic retinopathy occurs when the blood sugar level is too high. The best therapy is therefore the best possible blood sugar control. Any other risk factors that may exist should also be addressed. In addition, special ophthalmological treatments can potentially slow the progression of the disease.
Blood sugar control
In the therapy of type 2 diabetes, a long-term blood sugar level (HbA1c) between 6.5 and 7.5 percent is generally aimed for. In type 1 diabetes, the value should be below 7.5 percent. In individual cases, however, the attending physician can specify a different therapy goal:
For example, if a patient's high blood sugar values have already damaged medium and large vessels (such as leg vessels or coronary arteries), the HbA1c value should be between 7.0 and 7.5 percent. If there is already diabetes-related kidney damage (diabetic nephropathy), values below 7.0 percent are often aimed for.
Treatment of risk factors
Any risk factors for vascular damage that may be present must also be treated in order to prevent the increasing damage to the retina. One of the most important therapeutic measures is to use drugs to lower high blood pressure. Increased blood lipid levels (cholesterol, triglycerides) should be reduced through dietary measures. In addition, patients should avoid alcohol and nicotine, because these luxury foods are also bad for the blood vessels.
Ophthalmological treatment options
Advanced diabetic retinopathy can be treated with laser therapy and medication injected into the eye (vitreous humor). If there is bleeding into the vitreous body, the vitreous body can be removed and replaced with a clear liquid.
Laser therapy
In several sessions over the course of a few weeks, a laser is used to create targeted scars on the retina under local anesthesia (laser coagulation). Only areas of the retina that have already been pathologically changed are scarred, but the nerve cells are spared as much as possible. By eliminating the pathologically altered areas of the retina, the total oxygen requirement of the retina is reduced. This means that more oxygen is available to the healthy parts of the retina.
Laser therapy can prevent impending blindness. But it has side effects. The previously existing visual acuity is retained in only about half of the patients. After the treatment, visual disturbances in the dark (night blindness) and a restriction of the field of vision may occur. As a result of the procedure, water can also accumulate in the retina (retinal edema).
Injection of drugs into the vitreous humor
This intravitreal injection can be considered if the diabetes has led to swelling at the point of sharpest vision (macular edema) with involvement of the fovea. In most cases, so-called VEGF inhibitors are then injected. These active ingredients can inhibit the pathological growth of blood vessels in the eye.
If this therapy doesn't work, a cortisone may be injected into the vitreous humor. It has a vascular sealing effect and thus helps against swelling. However, cortisone injections increase the risk of cataracts and glaucoma.
Some of the active ingredients used are not officially approved for intravitreal injection in macular edema. They are therefore used “off-label”. They may only be used if the patient is first informed in detail about the effects and side effects of the drug and gives his written consent.
Vitreous removal (vitrectomy)
In some cases, diabetic retinopathy is associated with bleeding into the vitreous humor or retinal detachment. Bleeding into the vitreous body affects eyesight. In addition, the vitreous humor can be abnormally changed, especially in the presence of diabetic retinopathy, and thus cause retinal detachment. In these situations it makes sense to remove the vitreous body, which is almost completely made up of water (vitrectomy). This is done under local anesthesia. Then the resulting cavity is filled with a liquid or a gas.
A risk of the procedure: After the vitrectomy, the risk of cataracts can be increased.
Diabetic retinopathy: disease course and prognosis
Diabetic retinopathy is a chronic disease that can lead to complete blindness within a few years from being free of symptoms. Due to the lack of oxygen, more and more nerve cells in the retina die irreversibly. As a result, the eyesight deteriorates increasingly. There is also a risk of numerous complications such as increased intraocular pressure (glaucoma) and retinal detachment. Complete blindness as a result of diabetic retinopathy is observed in less than one percent of diabetic patients.
So far the disease cannot be cured. However, with the right treatment, their progression can often be slowed down. The decisive factor for the prognosis is, above all, how well the person concerned manages to control blood sugar and to eliminate other risk factors for diabetic retinopathy (high blood pressure, smoking, etc.).
When should diabetics go to the ophthalmologist!
In order for diabetic retinopathy to be recognized in good time, diabetics should visit an ophthalmologist at regular intervals:
- If there are no retinal changes and there is no particular risk, an eye examination is recommended every two years.
- If there are no retinal changes, but other risk factors (such as high blood pressure, high blood lipid levels, etc.) are present in addition to high blood sugar, the ophthalmological examination should be carried out once a year. This also applies if it is unclear whether a patient has such other risk factors.
- If there are already diabetes-related changes in the retina, patients should see an ophthalmologist at least once a year. This will decide at what intervals a check-up is necessary in each individual case.
If new symptoms appear in the eye area, such as a new deterioration in vision, blurred vision or "soot rain" in front of the eyes, a diabetic should see an ophthalmologist immediately. In this way, diabetic retinopathy or its deterioration can be recognized in good time.
Tags: organ systems alcohol drugs prevention