Endocarditis prophylaxis
and Florian Tiefenböck, doctorFlorian Tiefenböck studied human medicine at the LMU Munich. In March 2014, he joined as a student and has supported the editorial team with medical articles ever since. After receiving his medical license and practical work in internal medicine at the University Hospital Augsburg, he has been a permanent member of the team since December 2019 and, among other things, ensures the medical quality of the tools.
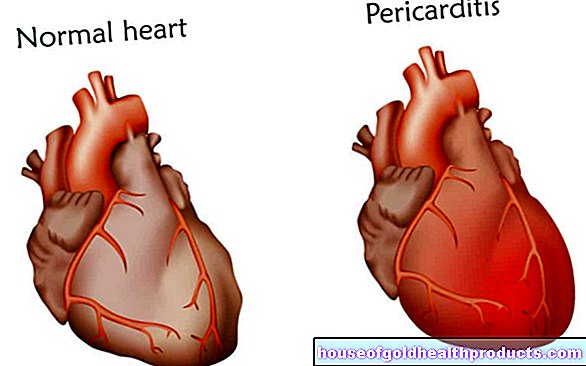
More posts by Florian Tiefenböck All content is checked by medical journalists.Endocarditis prophylaxis is understood to mean various measures that are intended to prevent endocarditis - an inflammation of the inner lining of the heart. Most often, the term endocarditis prophylaxis refers to antibiotic therapy prior to certain medical interventions that are associated with an increased risk of subsequent infectious endocarditis. Read more about endocarditis prophylaxis here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. I33I09I01I38I39

Endocarditis prophylaxis - for whom?
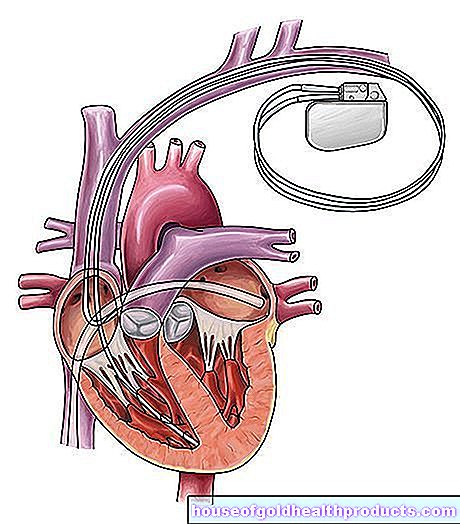
In most cases, infectious endocarditis occurs when the inner lining of the heart is affected by a previous disease. This could be, for example, in the case of a congenital heart or heart valve defect, but also if, for example, the aortic valve has changed in old age due to arteriosclerosis (hardening of the arteries). Every defect in the endocardium (inner lining of the heart), of which the heart valves also consist, offers a target for pathogens to attack. Even after certain heart operations, there is therefore a risk of cardiac inflammation.
Endocarditis can therefore best be prevented if the underlying diseases are treated or operated on at an early stage. At the same time, you have to avoid that large amounts of bacteria get into the bloodstream and thus into the heart - or at least render them harmless as quickly as possible. This is where endocarditis prophylaxis comes in.
According to the current status, the following patients belong to the high-risk group for cardiac inflammation or a severe course and therefore receive endocarditis prophylaxis:
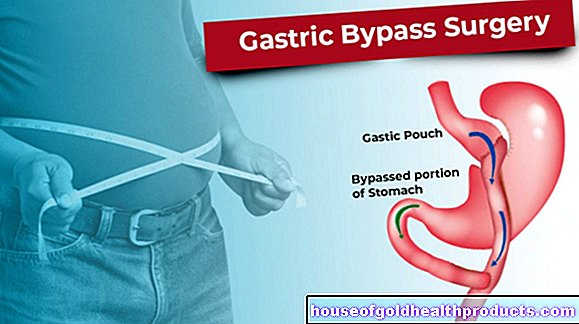
- Patients with artificial heart valves (mechanical or made from animal material)
- Patients with reconstructed heart valves with artificial material (in the first six months after the operation)
- Patients who have had endocarditis
- Patients with certain congenital heart defects ("cyanotic" heart defects)
- All heart defects treated with prostheses (in the first six months after the operation, for life if parts of pathological changes persist, e.g. a residual shunt or valve weakness)
- Patients who have had a heart transplant and develop problems with their heart valves (according to European guidelines, prophylaxis has not been required in this case since 2009, some doctors still use it for safety in everyday clinical practice)
Endocarditis prophylaxis - this is how it is carried out
Whether the doctor initiates endocarditis prophylaxis before an operation or procedure depends on the patient, the location of the procedure, and the particular procedure. Endocarditis prophylaxis is important if, during an operation, for example, bacteria are washed directly into the bloodstream due to injuries to the mucous membrane (bacteremia). However, the currently valid guidelines only recommend endocarditis prophylaxis in very few cases.
On the one hand, this is due to the fact that their benefits have not yet been clearly proven. On the other hand, the frequent use of antibiotics promotes resistant bacteria. The experts of the European Heart Society ESC only advise high-risk patients - as mentioned above - to endocarditis prophylaxis.
This is now almost only advocated for certain dental treatments, for example for interventions on the tooth holding apparatus, when a tooth is extracted or during implantation procedures. Endocarditis prophylaxis is also useful for high-risk patients when cleaning teeth and removing tartar, if major damage to the gums could occur.
Endocarditis prophylaxis is only used if the operating theater or examination area is infected. This includes various examinations or interventions in which the mucous membrane can be injured, for example in the gastrointestinal tract, the urinary and sexual apparatus or on the skin or soft tissues (e.g. muscles). Another area is interventions on the airways, such as tonsil surgery or lungoscopy.
A general recommendation for endocarditis prophylaxis is only available for certain treatments in the oral cavity and only for high-risk patients!
The patient takes an antibiotic in tablet form, such as amoxicillin, 30 to 60 minutes before the procedure. In the case of existing infections, the antibiotic for endocarditis prophylaxis is adapted to the respective pathogen, for example ampicillin or vancomycin in the case of an enterococcal infection in the intestine. In some cases, a drug is needed that cannot be taken as a tablet; in which case the doctor will give it as an infusion.
Endocarditis prophylaxis at home: oral hygiene factor
Temporary bacteremia (bacteria in the blood), which leads to endocarditis, can occur even without medical intervention. When chewing or brushing your teeth, for example, small injuries in the oral mucosa can cause bacteria to enter the bloodstream.
Careful oral hygiene is important to keep your gums healthy and resilient. You can also reduce the number of harmful bacteria in the oral flora in this way. It is advisable for everyone to brush their teeth regularly and to use dental floss and, if necessary, mouthwashes. Specialists especially recommend high-risk patients to have a dental check-up twice a year.However, if you suffer from a disease of the heart valves, for example, you not only maintain your oral health, but also take active endocarditis prophylaxis for your heart.
Tags: interview nourishment fitness







.jpg)



.jpg)