Pericarditis
Jens Richter is editor-in-chief at Since July 2020, the doctor and journalist has also been responsible as COO for business operations and the strategic development of
More posts by Jens Richter All content is checked by medical journalists.
When the pericardium is inflamed, the firm, connective tissue covering that surrounds and holds the heart in the chest becomes inflamed. Doctors speak of pericarditis (or pericarditis). It can be acute and severe or chronically insidious. An acute course is potentially life-threatening without medical treatment. Find out more about the causes, symptoms and treatment of pericarditis here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. I09I32I31I30
Pericarditis: description
Pericarditis or pericarditis is the inflammation of the connective tissue that completely surrounds the heart. It can be caused by pathogens such as viruses or bacteria, but also by non-infectious reactions of the immune system.
Pericarditis can occur acutely and is then often accompanied by severe symptoms. These can be life threatening. Because a common complication of acute pericarditis is the accumulation of fluid in the pericardium (pericardial effusion). It constricts the heart muscle and thus impairs its function (pericardial tamponade). But there is also chronic pericardial inflammation that progresses slowly.
Structure and function of the pericardium
The pericardium (pericardium) consists of a firm, hardly stretchable connective tissue. He holds the heart in place. The pericardium also protects the sensitive heart muscle and its blood vessels. A small amount of liquid of 20 to 50 milliliters lies between the pericardium and the heart muscle and reduces friction with each heartbeat.
Acute pericarditis
Infections, but also other diseases such as rheumatic diseases, can trigger acute pericarditis. In addition, pericarditis can be the result of a heart attack. The dead myocardium causes an inflammatory reaction. It can occur a few days after a heart attack when the inflammation spreads to the neighboring pericardium (early pericarditis, pericarditis epistenocardia). More rarely, the pericardium does not become inflamed until weeks after the myocardial infarction (Dressler syndrome, late pericarditis).
If white-yellowish fibrin deposits form during the inflammation (similar to a scrape when it closes), one speaks of fibrinous-acute pericardial inflammation.
If bacteria are the cause of the pericardial inflammation, there is a possibility that pus will form. This consists of dead immune cells and bacteria. A purulent acute pericardial inflammation is a sign of a fresh bacterial infection.
In some cases, the pericardial inflammation is bloody, for example as a result of a heart operation, after a heart attack or in the case of tuberculosis. Tumors or daughter tumors (metastases) growing in the pericardium can also cause bloody inflammation.
Chronic pericardial inflammation
Chronic pericardial inflammation often occurs when acute pericarditis (despite treatment) does not heal completely and keeps flaring up. If pericarditis persists for three months, doctors speak of chronic pericarditis. It can also develop without an acute history. For example, tuberculosis, rheumatological diseases, some medications or medical radiation (for example in the case of a lung tumor) can cause chronic pericardial inflammation.
Panzerheart
Due to the inflammatory reactions, the pericardium may store "calcium" and scar. That makes him more and more immobile. This also reduces the space for the working heart muscle, for example it can no longer fill properly. With the so-called armored heart, the actually thin protective bag around the heart can grow to a thickness of one centimeter and severely constrict the heart (pericarditis constrictiva).
Perimyocarditis
Since the pericardium is close to the heart muscle, both structures are sometimes inflamed at the same time. Doctors then speak of perimyocarditis. It is usually difficult to tell the difference between pericarditis and myocarditis. However, this is not absolutely necessary, as the treatment often does not change. This is done in the hospital, however, as the risk of complications is increased.
Pericarditis: symptoms
Typical symptoms of acute pericardial inflammation are pain behind the breastbone (retrosternal pain) or in the entire chest. The pain can also radiate to the neck, back or left arm and is aggravated when you inhale, cough, swallow or change your position. Often times, people with acute pericarditis also have a fever.
In some cases the heartbeat is certain to accelerate (tachycardia). Cardiac arrhythmias and the feeling of stumbling the heart also occur with pericarditis. Depending on the severity of the disease, there may be shortness of breath and chest tightness. Similar complaints can also occur with pneumonia with pleurisy, a collapsed lung (pneumothorax) or especially with an acute heart attack.
You should always have the cause of acute chest pain clarified immediately!
Many symptoms only arise when fluid collects in the pericardium.Dry, fibrinous pericarditis therefore often only manifests itself as pain. The symptoms of wet (exudative) pericarditis, for example due to a bacterial infection, depend on the amount of effusion. The more fluid that collects in the pericardium, the more the cardiac function is restricted. If the heart muscle no longer works properly, those affected suffer from symptoms of cardiac insufficiency (heart failure). An armored heart also ultimately leads to poor heart function.
If the pericardium is chronic from the start, symptoms usually develop insidiously. It therefore often goes unnoticed for a long time. In addition to general symptoms of inflammation such as fatigue and reduced performance, symptoms of cardiac insufficiency can also occur as the pericardium becomes scarred and thickened:
- Faster heartbeat and flatter pulse
- Difficulty breathing during physical exertion (later also at rest)
- cough
- Blocked (visibly protruding) neck veins
- Edema
- "Paradoxical pulse" (pulsus paradoxus = decrease in systolic blood pressure by more than 10 mmHg when inhaling)
Complication of pericardial tamponade
Pericardial tamponade is a life-threatening complication of pericarditis. It occurs when a lot of blood, pus, and / or inflammatory fluid builds up quickly in the pericardium. Since the pericardium cannot expand, the effusion constricts the heart muscle and the heart chambers can no longer expand properly. This means that less blood is pumped to the lungs (from the right ventricle) or into the body's circulation (from the left ventricle). The blood pressure drops, the heart races. In addition, the blood backs up in the veins, which can be seen in protruding neck veins. It is difficult for them to breathe. People suddenly appear pale and sweaty. The cycle can collapse. A pericardial tamponade is acutely life-threatening and must be treated immediately.
Pericarditis: causes and risk factors
Acute pericarditis can be triggered by various factors. Viruses or bacteria are often the trigger, sometimes (especially if the immune system is weakened) fungi or parasites. They get to the heart from the respiratory tract or other organs via the blood or lymph vessels.
But other diseases or treatment methods can also cause pericarditis. This includes:
- Kidney failure with increased levels of uric acid in the blood
- Autoimmune diseases and rheumatic diseases
- Metabolic disorders (hypothyroidism or hypercholesterolemia)
- Consequences of a heart attack
- Heart surgery (postcardiotomy syndrome)
- Tumor diseases
- Radiation therapy
Pericarditis: examinations and diagnosis
If an inflammation of the pericardium is suspected, the general practitioner will in most cases refer the patient to a heart specialist (cardiologist). This first asks the medical history:
- How long have the complaints existed?
- Have the symptoms increased or have new complaints been added?
- Do you feel less physically resilient?
- Do you have a fever - and if so, how long has it been?
- Have you had an infection in the past few weeks - especially in the respiratory tract?
- Does the chest pain change when you breathe or when you lie down?
- Have you ever had ailments or diseases of the heart in the past?
- Do you have any known rheumatism or any other disease of the immune system?
- What medications are you taking?
The so-called physical examination includes taking a temperature, palpating the pulse, measuring blood pressure and tapping and listening to the chest. In the case of pericarditis, the doctor can often hear a characteristic rubbing with each heartbeat when the effusion is still small. If the effusion is already extensive, the examiner hardly hears the heartbeat any more.
A blood sample is used to search for typical markers for an inflammation or an infection. These include:
- Accelerated sedimentation rate
- Increased CRP value
- Increase in white blood cells (leukocytosis in bacteria or fungi, lymphocytosis in viruses)
- Detection of bacteria in the blood culture
- Elevated cardiac enzyme levels (CK-MB, Troponin T)
- Increased so-called rheumatoid factors
Various technical investigations then confirm the suspected diagnosis of pericarditis:
- ECG: abnormal ST segment elevation, flatter or negative T-wave or, in the case of a pericardial effusion, overall reduced rashes (low voltage)
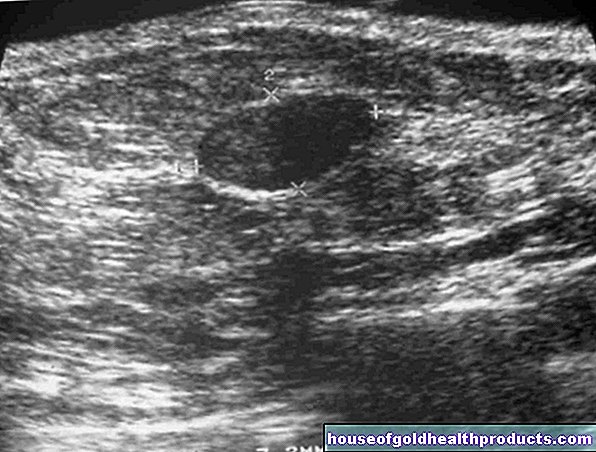
- Echocardiography ("heart ultrasound") to detect an effusion
- X-ray examination of the chest ("X-ray thorax", only shows large effusions through enlarged heart shadow)
- Magnetic resonance imaging (MRI) or computed tomography (CT) to show the pericardial wall and any existing effusion
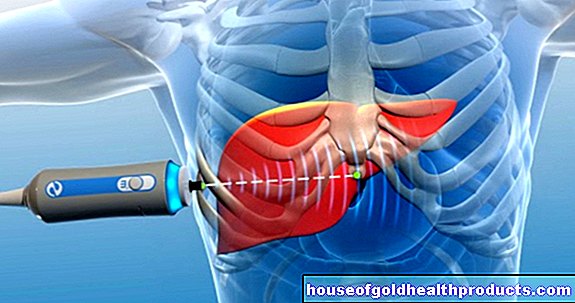
- Pericardial puncture (if there is an existing effusion) to relieve the heart, assess the condition and attempt to detect pathogens
Pericarditis treatment
The first measure to be taken in case of pericarditis is to take some rest to relieve the heart. Doctors usually treat viral pericarditis on an outpatient basis. They then prescribe anti-inflammatory drugs, for example NSAIDs such as ibuprofen, ASA or colchicine. Means directly against the viruses are not used (or only in individual cases).
In some cases, however, certain circumstances increase the risk that pericarditis will be complicated. If such a risk factor is present, doctors refer the person concerned to a hospital. For example, a high fever over 38 degrees or a large pericardial effusion are among these risk factors.
If a specific cause of pericarditis is known, it determines the further treatment (causal therapy):
at bacterial infections doctors prescribe antibiotics. They are often given as an infusion to make them work better.
at Fungal infections fungicides, so-called antimycotics, are used. These are also often given as short infusions.
at Autoimmune diseases the excessive immune reactions are suppressed with drugs. Suitable active ingredients are, for example, glucocorticoids, cyclophosphamide or methotrexate (“MTX”).
Is a Kidney failure the cause of the pericardial inflammation, the blood has to be cleaned by means of a so-called dialysis.
The success of the treatment is checked by regular ultrasound examinations of the heart. In the case of chronic pericardial inflammation with thickening and scarring of the pericardium (armored heart), the pericardium must be removed by an operation on the open chest (pericardectomy).
Treatment of pericardial tamponade
With a pericardial tamponade, so much fluid collects in the pericardium that the heart's function is impaired. It is life threatening and needs immediate treatment. For this purpose, the pericardium is punctured from the outside through the chest with a needle under ultrasound control (sonography) and the effusion fluid is drawn off. The patient must then be closely monitored by ultrasound in order to detect any trailing effusion fluid or blood at an early stage.
Even slowly but steadily increasing pericardial effusions relieve doctors with a puncture if those affected are suffering from it. In this way, they want to prevent further, ultimately life-threatening restrictions in cardiac function at an early stage. If the fluid hardly increases and the patient does not experience any symptoms, no pericardial puncture is performed.
Pericarditis: disease course and prognosis
Pericarditis is a serious disease. It can extend to the heart muscle (perimyocarditis) or the entire heart (pancarditis). The effusion that sometimes occurs (serous fluid, pus or blood) can dangerously constrict the heart muscle. If pericarditis is recognized early and its causes and consequences treated, it can heal without consequences. If left untreated, pericarditis is a life-threatening disease due to its serious complications (armored heart and pericardial tamponade).
Tags: vaccinations sex partnership baby toddler