Heart failure
and Martina Feichter, medical editor and biologistSophie Matzik is a freelance writer for the medical team.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
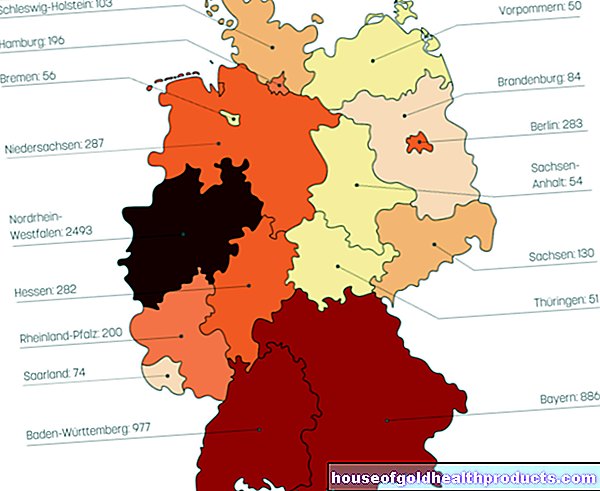
With heart failure (heart failure, heart failure, myocardial insufficiency), the heart is no longer able to supply the body with sufficient blood and thus oxygen. The disease is one of the most common causes of death in Germany. Read everything you need to know about: What is Heart Failure? What are the causes? What are the symptoms? How is heart failure diagnosed and treated?
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. I50
Heart Failure: Quick Reference
- Causes: in the first place, narrowing of the coronary arteries (coronary heart disease), high blood pressure, heart muscle diseases (cardiomyopathies), inflammation of the heart muscle (myocarditis), heart valve defects, cardiac arrhythmias, chronic lung diseases, heart valve defects, heart attack, increased, liver cirrhosis, drug side effects
- Symptoms: Depending on the stage, shortness of breath (dyspnea) during exercise or at rest, reduced performance, fatigue, pale or blue discoloration of the lips and nail beds, edema, especially on ankles and lower legs, throat vessels, rapid weight gain, nocturnal urge to urinate, palpitations, cardiac arrhythmias, lower Blood pressure
- Diagnostics: physical Examination, blood pressure measurement, listening to the heart and lungs, blood sampling with determination of the biochemical heart failure markers BNP (Brain Natriuretic Peptide), NT-proBNP, and MR-proANP (which are released by a stretching stimulus on the heart muscle), cardiac ultrasound, X-ray of the chest, EKG / long-term EKG, cardiac catheter
- Treatment: Drugs to lower blood pressure (antihypertensive drugs), to flush out (diuretics), to slow down the heartbeat (e.g. beta blockers), to reduce the effect of certain hormones (aldosterone antagonists) and to strengthen the heart's strength (e.g. digitalis). Depending on the cause, surgery (e.g. heart valves, bypass, pacemaker), sometimes heart transplant
Heart failure: causes and risk factors
With heart failure (heart failure), the heart is no longer as efficient as a healthy heart. It can no longer adequately supply the body's tissues with blood (and thus oxygen). That can be life-threatening. Heart failure can have several causes:
The most common cause of heart failure is calcification of the coronary arteries (coronary heart disease, CHD). The calcium plaques constrict the vessels that supply the heart muscle and the blood can no longer flow properly. As a result, the heart muscle is undersupplied and is no longer as efficient.
The second main cause is high blood pressure (hypertension). With high blood pressure, the heart has to pump harder continuously, for example against narrowed blood vessels. Over time, the heart muscle thickens in order to be able to build up more pressure (hypertrophy). In the long term, however, it cannot withstand this load - and the pumping capacity declines.
Other causes of heart failure are cardiac arrhythmias and heart muscle inflammation. Defects in the heart septum and heart valve defects (congenital or acquired) can also lead to cardiac insufficiency. The same applies to an accumulation of fluid in the pericardium (pericardial effusion or pericardial effusion, especially in the case of pericarditis).
Heart failure can also be caused by heart muscle diseases (cardiomyopathies). These in turn can arise, for example, from inflammation or excessive alcohol, drug or medication abuse. A special case is the so-called stress cardiomyopathy. After a serious traumatic event, a life-threatening heart failure suddenly occurs (mostly in women after the menopause). In this disease, also known as Tako Tsubo cardiomyopathy, the heart function usually returns to normal. So there is no permanent heart failure. Life expectancy and quality of life are therefore not impaired after stress cardiomyopathy has been overcome.
Metabolic diseases can also play a role in the development of heart failure. Examples are diabetes mellitus and disorders of the thyroid function (such as hyperthyroidism = overactive thyroid).
Lung diseases such as emphysema or COPD (chronic obstructive pulmonary disease) are other possible causes of heart failure. In particular, the rarer right heart failure (functional weakness of the right half of the heart) can be due to a lung disease. Because in the diseased lungs, the vessels are usually also damaged. The blood can no longer flow through them properly (pulmonary hypertension). It backs up in the right heart and puts a strain on it.
In some people, heart failure develops as a result of anemia or other organ diseases, such as the liver or kidneys. In rare cases, an AV fistula (AV shunt) leads to heart failure. This is an abnormal short circuit between an artery and a vein.
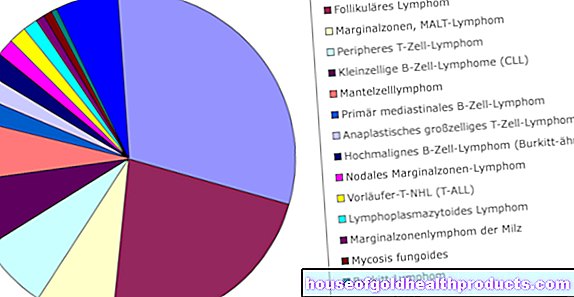
Sometimes drugs also cause heart failure. This risk exists, for example, with certain agents for cardiac arrhythmias, certain cancer drugs (antineoplastic agents), appetite suppressants and migraine drugs (such as ergotamine). But also tumors of the heart or cancerous settlements (metastases) can cause heart failure.
Systolic and diastolic heart failure
Heart failure is generally made up of two parameters: systolic and diastolic heart failure.
The term systolic heart failure (also known as congestive heart failure) describes the heart's reduced ability to pump: the pumping function and the ejection capacity of the left heart chamber (ventricle) are reduced. This means that the organs are no longer adequately supplied with blood. In addition, the blood backs up. This causes edema, for example in the arms and legs or in the lungs.
In addition to systolic heart failure, diastolic heart failure usually also occurs. This means that the heart chambers are no longer adequately filled with blood. Most of the time, the left ventricle is abnormally changed, making it less flexible and unable to take in sufficient blood. As a result, less blood is pumped into the body's circulation. This leads to an insufficient supply of oxygen to the body. Diastolic heart failure occurs mainly in old age. Women are affected more often than men.
Heart failure: classification
Heart failure can be classified according to various criteria:
- Depending on the affected heart area, a distinction is made between left heart failure, right heart failure and global heart failure (both halves of the heart affected).
- Depending on the course of the disease, a distinction is made between acute heart failure and chronic heart failure.
- A rough division according to the condition of the disease is into compensated heart failure and decompensated heart failure.
- A more precise differentiation is offered by the NYHA classification of heart failure, a classification of the stages according to the degree of complaint, published by the New York Heart Association.
The European Heart Society (ESC) also classifies heart failure according to the ejection capacity of the heart. If the left heart continues to pump enough blood, doctors speak of a preserved ejection quantity (ejection fraction = EF, normal value 60-70%). In contrast, there is the reduced amount of ejection. This results in the following classification:
- Heart failure with reduced left ventricular EF (HFrEF, EF <40%)
- Heart failure with moderate EF (HFmrEF, EF = 40-49%)
- Heart failure with preserved EF (HFpEF, EF is at least 50%)
Heart failure: left, right, global
In right heart failure, the right atrium and the right ventricle of the heart muscle are particularly affected by cardiac insufficiency. The right side of the heart is the side that the deoxygenated blood from the body is first directed to. From there it pumps the blood further into the lungs in order to “fill up” with new oxygen. The enriched blood then flows into the left half of the heart and from there into the body's circulation.
Increased pressure in the lungs due to illness leads to a backlog in the blood flow: the right ventricle then has to pump the blood into the lungs with more force. As a result, the heart is overloaded and damaged over time (pulmonary heart / cor pulmonale). The excessive strain causes the muscle layer in the wall of the right ventricle to thicken.
If the right half of the heart can no longer generate the extra power, the blood builds up in the supplying vessels (veins). The increased pressure in the veins causes water to accumulate (edema) in the body, especially in the legs and abdomen.
Right heart failure usually develops as a result of chronic left heart failure.
In left heart failure, the pumping capacity of the left half of the heart is no longer sufficient. As a result, the blood backs up in the pulmonary vessels (congested lung). This is particularly dangerous as it can cause water to accumulate in the lungs (pulmonary edema).Cough and shortness of breath are typical symptoms.
When global heart failure is present, the pumping capacity of both parts of the heart is reduced. So there are symptoms of right and left heart failure.
Heart anatomy
Acute heart failure and chronic heart failure
In acute heart failure, the first symptoms appear very quickly within a few hours to a few days. The causes are mostly other diseases. Chronic heart failure develops slowly over the course of several months to years.
Compensated and decompensated heart failure
The terms compensated heart failure and decompensated heart failure describe the cases in which symptoms occur. Compensated heart failure usually only triggers symptoms when exerted. On the other hand, the heart can still provide the required performance when it is at rest, so that there are no symptoms.
On the other hand, decompensated heart failure causes symptoms such as water retention (edema) or shortness of breath (dyspnea) even at rest or under low stress.
Doctors mainly use the terms when they are already aware of cardiac insufficiency. If the symptoms are under control (for example with the right medication), the heart failure is compensated. However, if this condition gets out of hand (e.g. due to acute illnesses or a lack of tablet intake), the heart failure is considered decompensated.
Heart failure: NYHA classification
The NYHA (New York Heart Association) has created a generally applicable classification of heart failure based on the observable symptoms:
- NYHA I: No physical symptoms at rest or during everyday stress.
- NYHA II: Slight restrictions in physical resilience (e.g. 2 flights of stairs), but no symptoms at rest.
- NYHA III: High restrictions even with everyday physical stress. Complaints such as exhaustion, cardiac arrhythmias, shortness of breath and "chest tightness" (angina pectoris) occur quickly even with low stress.
- NYHA IV: Symptoms show up with any physical exertion and at rest. Those affected are mostly immobile (bedridden) and depend on permanent help in their daily life.
Heart failure: symptoms
Heart failure: symptoms of left heart failure
The left part of the heart is where the blood passes after it has been oxygenated in the lungs. When this half of the heart no longer functions properly, the blood backs up into the lungs. This leads to coughing and difficulty breathing (dyspnoea). In most cases, shortness of breath only occurs during exercise (exercise dyspnea) and only later at rest (dyspnea at rest). In many of those affected, it is particularly noticeable at night when lying down, as the blood (and therefore water) then flows back more easily to the weak heart.
Heart failure symptoms with "asthma cardiale"
If the left heart failure continues, fluid will leak from the pulmonary capillaries into the alveoli. In addition to shortness of breath, this also leads to increased urge to cough. At the same time, the bronchi can cramp. This symptom complex is also called "asthma cardiale" ("heart-related asthma").
If more fluid flows into the lung tissue, what is known as pulmonary edema develops. Its characteristics are severe shortness of breath and "blistering" breathing noises. Due to the insufficient supply of oxygen, the skin and mucous membranes turn bluish (cyanosis). Some patients then cough up foamy, sometimes flesh-colored secretions. If fluid collects around the lungs in the pleural space, doctors speak of a pleural effusion. It is also one of the possible symptoms of heart failure.
Heart failure patients usually sit down instinctively with an upright and elevated upper body because of the breathing problems. That will ease the symptoms. In addition, the auxiliary breathing muscles can be used more effectively in this position.
Heart failure: symptoms of right heart failure
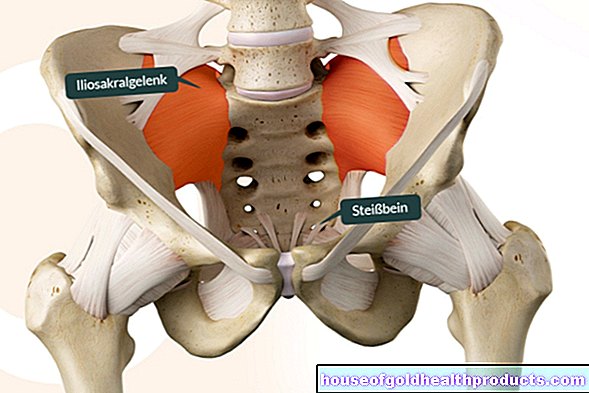
The deoxygenated blood from the body flows to the right part of the heart. It is pumped from the right ventricle to the lungs, where it is re-oxygenated. If the right half of the heart is affected by the weak heart, the butt backs up into the body veins. Typical heart failure symptoms in this case are water retention in the body (edema). They usually show up first in the legs (leg edema) - especially on the ankles or on the back of the foot, then also over the shins. In bedridden patients, the edema usually first develops over the sacrum.
In the advanced stages of right heart failure, water is also stored in the organs. Other typical symptoms of cardiac insufficiency are therefore impairment of organ functions. A congestion in the stomach (congestion gastritis) manifests itself for example through loss of appetite and nausea, a congestion of the liver through pain in the right upper abdomen. Fluid can also collect in the abdominal cavity (ascites, ascites).
The water retention often causes rapid weight gain, often more than two pounds per week.
This swelling can dry out the skin because the pressure in the tissue becomes too great. Possible consequences are inflammation (eczema), which can develop into open, poorly healing wounds.
Global heart failure: symptoms
If both halves of the heart are affected by the organ weakness, one speaks of global heart failure. The symptoms of both forms of disease (right and left heart weakness) then appear together.
More heart failure symptoms
Heart failure causes water retention (edema) throughout the body. These are released (mobilized) especially at night when the person concerned is lying down. The body wants to excrete the released, excess fluid through the kidneys. This is why those affected have to go to the toilet very often at night. This frequent nocturnal urination is known as nocturia.
Breathing is disturbed, especially in the advanced stages of heart failure. A common form is the so-called Cheyne-Stokes breathing. This can be recognized by the fact that the breathing depth and thus also the breathing noise periodically increase and decrease. It occurs when the central nervous system is no longer properly supplied with blood due to advanced cardiac insufficiency.
The heart beats very quickly during exercise (palpitations = tachycardia). In addition, cardiac arrhythmias can occur, especially in the case of pronounced cardiac insufficiency. The arrhythmias can become life-threatening and must then be treated immediately.
Another classic late-stage heart failure sign is low blood pressure.
General and very common symptoms of heart failure are also decreased performance, tiredness and exhaustion.
Heart failure: examinations and diagnosis
The heart failure diagnosis is based on the recording of the medical history (anamnesis) as well as on physical and technical examinations.
During the anamnesis interview, the doctor asks the patient, among other things, about his or her symptoms and whether there has already been any heart disease in the family (genetic predisposition).
There are various options for the physical examination, which vary in terms of time and effort. In addition, the physical examination serves to rule out other diseases that also cause heart failure symptoms such as shortness of breath and chest pain (differential diagnosis).
Cardiac ultrasound (echocardiography)
Listening to the heart's activity with the stethoscope provides the doctor with initial indications of a heart valve defect or a weak heart muscle. When listening to the lungs, a rattling noise is a sign of heart failure. It indicates water retention in the lungs. Rattling noises also occur, for example, with pneumonia. The doctor may also hear a third heart sound (this is otherwise only normal in children and adolescents).
If there is edema in the legs, visible dents can be pressed into the skin. If the doctor measures the pulse, it may change its intensity with each beat (pulsus alternans). The examiner also recognizes protruding jugular veins - signs of a backlog of blood.
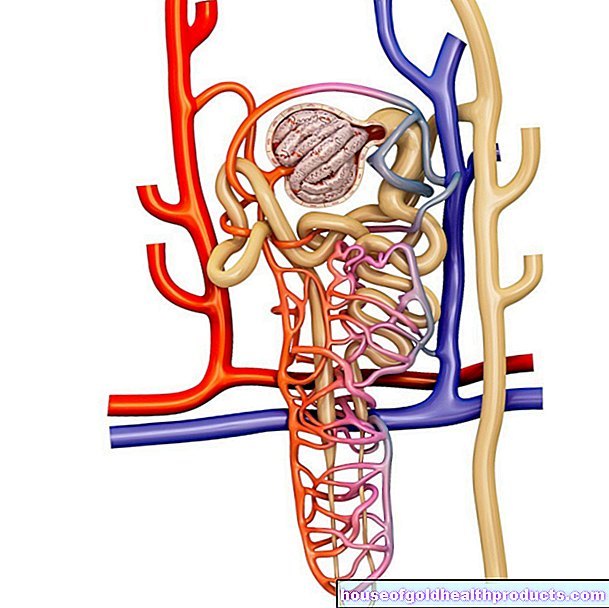
The function of the heart can be assessed with a heart ultrasound (echocardiography). The doctor can see whether there are any defects in the valves, in the structure of the heart walls or in the interior of the heart. A thickened wall structure and the ejection capacity of the heart are also made visible in this way.
The blood flow that flows through the heart can be visualized with the help of color Doppler sonography. This is a special form of ultrasound examination. With an ultrasound device, the doctor can also see accumulations of fluid, for example in the abdomen (ascites) or chest (pleural effusions). At the same time, he checks the vena cava and organs for signs of congestion.
Cardiac arrhythmias are best detected with a long-term EKG. The person concerned is given a small portable device to take home with them. It is connected to the electrodes that the doctor places over the patient's chest and continuously records the heart's activity. A long-term ECG usually runs for 24 hours. The examination is painless and does not harm the patient.
With a heart catheter examination, the doctor can check whether narrowed coronary arteries are causing the heart failure. The examination usually takes place under local anesthesia. If narrowed areas are discovered, they can be stretched immediately. Under certain circumstances, stents (vascular supports) are used to keep the coronary artery permanently open. Furthermore, stress tests (e.g. on a bicycle ergometer) help to assess the extent. In some cases, the heart is so weak that these tests are no longer possible.
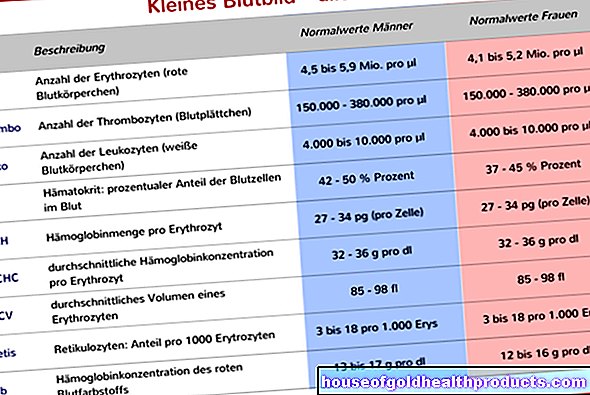
Blood pressure measurements are also carried out if heart failure is suspected. In addition, the doctor will order various urine and blood tests in the laboratory. Among other things, the urine status and a blood count are made. The electrolytes (especially sodium and potassium) are also determined. Various organ parameters such as creatinine, fasting blood sugar, liver enzymes including coagulation values and the protein Brain Natriuretic Peptide (BNP, also NT-proBNP) are also measured. Heart failure leads to an increase in the BNP level, as it is released when the heart is overstretched and stressed. This value is closely related to the severity of heart failure (NYHA classification).
With the help of these examinations, for example, disorders of the liver, kidneys or thyroid can be determined. Elevated blood lipid levels and diabetes mellitus can also be diagnosed in this way.
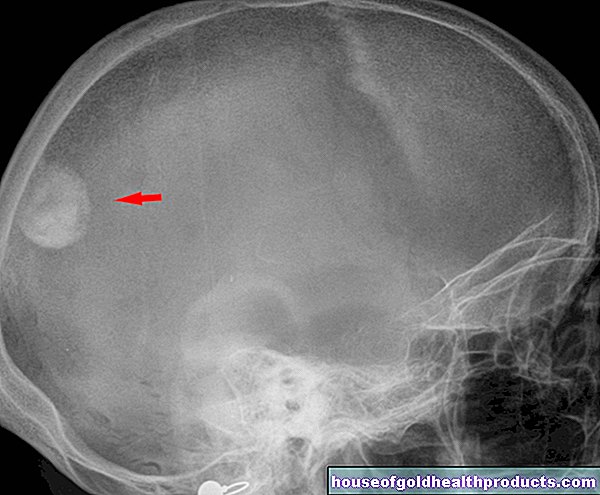
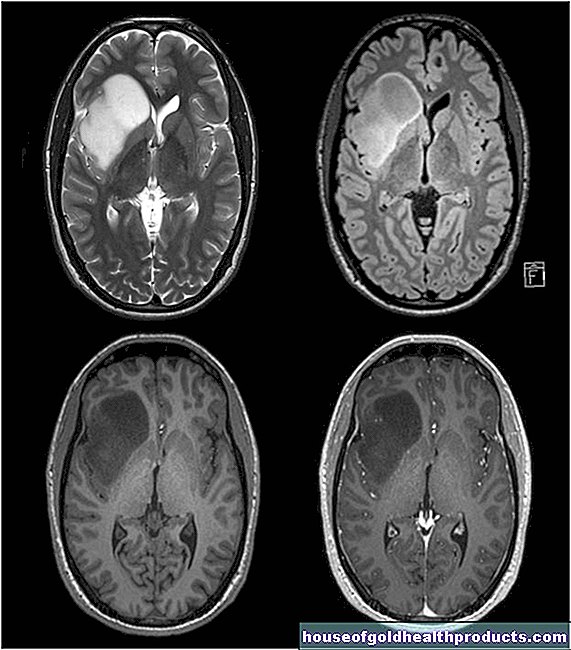
In addition, chest x-rays and magnetic resonance imaging (MRI) can help diagnose heart failure.
Heart failure: treatment
Heart failure therapy consists of several components and depends primarily on the severity of the heart failure. In addition to drug therapy, personal lifestyle is also fundamental. If the illness is severe, a pacemaker or a heart transplant may be necessary.
In general, heart failure is a progressive disease that often leads to death. The therapy guidelines of international specialist societies therefore recommend palliative care for all patients. This includes, on the one hand, symptom relief (for example with medication or surgery). On the other hand, this also includes intensive communication between doctor and patient: Everything important about diagnosis, therapy, course and prognosis of the disease should be discussed together. You should also take care of power of attorney and living wills. This makes it easier for the patient and his relatives to deal with the disease.
Heart failure: medication
With heart failure drug therapy, the aim is to prevent complications of the disease and improve the patient's quality of life. Different drugs are used depending on the cause of the heart failure. Some drugs have been shown to improve the prognosis, others primarily alleviate existing symptoms.
Active ingredients from the group of ACE inhibitors (first choice) and beta blockers are very often used in heart failure therapy. According to the latest studies, they have a life-prolonging effect. In order for these and other drugs to work properly, they must be taken permanently and regularly as prescribed by the doctor.
Overall, there are various active ingredients available for heart failure therapy. The most important are:
- ACE inhibitors: They block a protein that is responsible for narrowing blood vessels in the body. This keeps the blood vessels dilated and the blood pressure drops. This relieves the heart and the remodeling of the heart muscle as a result of the permanent overload is slowed down. The doctor usually prescribes ACE inhibitors first (NYHA I).
- AT-1 antagonists (sartans): They block the effects of a blood pressure-increasing hormone. However, they are only used if the patient cannot tolerate ACE inhibitors.
- Beta blockers (beta receptor blockers): They lower blood pressure and pulse, prevent life-threatening cardiac arrhythmias and thus improve the prognosis of heart failure. They are usually used from NYHA stage II, but also earlier, for example if a heart attack has occurred.
- Mineralocorticoid receptor antagonists (MRA): These are also indicated in NYHA stages II-IV, especially when the heart is no longer pumping sufficiently (EF <35%). They increase the excretion of water from the body, which ultimately relieves the heart. This treatment is supposed to help reverse the damaging heart muscle remodeling as "antifibrotic therapy".
- Sacubitril / Valsartan: This combination of active ingredients is only prescribed in certain cases of chronic heart failure. Sacubitril is a so-called neprilysin inhibitor and thus inhibits the breakdown of hormones in the body that dilate the blood vessels. Valsartan counteracts the effects of the blood pressure increasing hormone angiotensin.
- Ivabradine: This drug lowers the heart rate. Doctors prescribe it if the heartbeat is too fast (> 70 / min), even with beta blockers, or if these are not tolerated.
- Digitalis: Preparations with digitalis improve the pumping power of the heart. It does not prolong life, but increases the quality of life and the resilience of those affected. Digitalis (Digitoxin, Digoxin) is used to control the frequency of atrial fibrillation, a common cardiac arrhythmia.
- Diuretics: Diuretics are water tablets. They excrete stored fluid, so that the heart and blood vessels are less stressed. So they are always used when the patient suffers from edema.
- According to the new European guidelines on heart failure, standard therapy includes diuretics, ACE inhibitors and beta blockers, and MRA in NYHA stages II-IV.
Every drug can also have side effects. For example, a common side effect of ACE inhibitors is a dry cough. However, this is usually harmless. AT1 antagonists and diuretics can upset the blood salt balance, while beta blockers can greatly slow the heartbeat. If heart failure patients experience side effects from medication, they should tell their doctor. He or she can adjust the dosage or possibly even prescribe a different preparation.
Hawthorn for heart failure
Herbal medicine recommends hawthorn preparations for heart failure. They are said to improve the force of contraction and the supply of oxygen to the heart muscle. They also counteract cardiac arrhythmias (antiarrhythmic effect). From a scientific point of view, no relevant and reliable effectiveness of hawthorn for heart failure has been proven. If patients still want to try such medicinal plant preparations, then in consultation with the doctor or pharmacist and in addition to conventional medical heart failure treatment.
Iron substitution as an infusion is indicated if the ferritin value is below 100 micrograms per liter or the transferrin saturation is below 20 percent. This measure can make breathing easier. Because iron is a basic component of our oxygen transporters in the blood, the red blood cells (erythrocytes). Iron deficiency sooner or later leads to anemia, which promotes heart failure.
Hawthorn for heart failure
Pacemaker against heart failure
For people with advanced heart failure, a so-called biventricular pacemaker (CRT = cardiac resynchronization therapy) can be combined with drug therapy. Both together can compensate for the weak heart. With CRT, pacemaker wires are inserted into the heart chambers so that they beat in the same rhythm again.
Patients who have survived cardiac arrest or who suffer from dangerous cardiac arrhythmias benefit from an implantable defibrillator (implantable cardioverter / defibrillator, ICD).The device is used like a pacemaker. It will deliver an electric shock if it detects a dangerous rhythm disturbance.
Sometimes doctors also use a combination device from both systems, the so-called CRT-ICD system (also CRT-D system).
Surgical measures
If heart failure worsens despite an existing therapy, it may be necessary to replace the old heart with a new one (heart transplant). Patients can receive a donor heart or an artificial heart. This can lead to various complications such as rejection reactions.
Narrowed coronary arteries (coronary heart disease, CHD) are one of the most common causes of heart failure. The impaired blood flow can be improved surgically by widening the vessels as part of a cardiac catheter examination (balloon dilatation, possibly with the installation of a stent = vascular support). You can also use a bypass.
If defective heart valves are the reason for the heart failure, an operation may also be necessary. Sometimes a "repair" (reconstruction) of the heart valve is possible. In other cases, the defective heart valve is replaced (biological or mechanical valve prosthesis).
Heart Failure: What You Can Do Yourself
If your doctor has diagnosed you with heart failure, it is imperative that you follow a healthy lifestyle. This minimizes risk factors and increases the quality of life. You should therefore heed the following:
- Diet: Eat a diet with sufficient fruit and vegetables. Avoid animal fats if possible and eat low-salt. Salt ensures that water is stored in the body. The heart then has to work harder.
- Fluid intake: The amount of daily fluid intake should be discussed with your doctor. In general, if you have a weak heart, you should never drink three or more liters a day. In most cases, a fluid intake of around 1.5 liters per day is ideal.
- Exercise: An effective heart failure therapy always includes exercise and moderate physical activity. In everyday life, for example, you can walk to work and take the stairs instead of the elevator. Walks, light strength and coordination exercises, swimming, cycling and walking are also recommended. You can also join a sports group for heart patients (rehab sports). Discuss with your doctor which physical activities and sports make sense in your case and to what extent you are allowed to exercise.
- Body weight: Being overweight has a very negative effect on heart failure. If your body mass index (BMI) is over 40, you should definitely reduce your weight. Weight loss should be controlled and slow, and in any case under the supervision of a doctor. Heart failure patients of normal weight should also check their weight regularly, preferably on a daily basis. A very rapid and large gain in weight can be an indication of water retention in the body. Rule of thumb: If you gain weight by more than one kilo per night, more than two kilos in three nights or more than 2.5 kilos in a week, you must definitely see a doctor.
- Alcohol: Minimize your alcohol consumption, as alcohol can damage the heart muscle cells. Women are advised not to consume more than twelve grams of pure alcohol (a standard drink) per day. Men should not consume more than 24 grams of pure alcohol (equivalent to two standard drinks) per day. Patients whose heart failure is caused by excessive alcohol consumption (alcohol-toxic cardiomyopathy) should completely avoid alcohol.
- Smoking: It is best to give up smoking completely!
- Vaccination: Get vaccinated against flu every year and pneumococcus every six years.
- Journal: Keep a journal of any complaints you notice. So you can’t forget anything at your next visit to the doctor.
Exercise for heart failure
Patients with heart failure have long been advised to take physical rest and avoid physical exertion. However, many scientific studies have found a positive effect of moderate endurance training in heart failure. Physical activity is not only safe, it is an important part of treatment.
Exercise in heart failure improves the physical performance and quality of life of those affected. However, it is still unclear whether the activity also has an effect on the life expectancy of the patients.
Warning: In the case of acute illnesses such as an acute coronary syndrome, shortness of breath at rest, water retention in the tissue or an inflammation of the myocardium within the preceding two days, the patient should not participate in any sport.
Start training with heart failure
Before the patient can start exercising, the doctor performs a spiroergometry. This enables him to determine the patient's maximum performance. The patient then receives a tailor-made training plan.
Which sport for heart failure?
There is no one-size-fits-all training plan for people with heart failure. As with recreational sports, exercise variation is important in making progress. Exercise for heart failure comprises three components:
- High intensity interval training (HIT): three times a week
- moderate endurance training: three to five times a week
- Strength and endurance training: two to three times a week
High intensity interval training (HIT)
The HIT usually begins with an active “rest phase”. This means that the athlete moves at medium intensity, i.e. at 50 percent of his maximum performance. The duration is usually around three to five minutes. This is followed by the intensive training phase with a load of 60 to 100 percent of maximum performance. He does this for up to three minutes.
Note: The duration of the training phases in HIT must always be adapted to the individual health and fitness of the person concerned.
With HIT, the resting phase and the intensive phase alternate and form a cycle. Several cycles follow one another in a training session. The number of cycles that form a unit is always adapted to the performance and the state of mind of the patient. The training lasts 15 to 30 minutes in total.
People with heart failure should do high-intensity interval training three times a week.
Moderate endurance training
With moderate endurance training, the training intensity remains the same over a longer period of time. In the beginning, the patient should train at 40 to 50 percent of their maximum capacity. If he sustains this intensity for ten to 15 minutes, the intensity can be increased.
The person concerned follows the so-called ÖLI rule (= more often, longer, more intensive). This means that the training frequency is increased first, then the duration and lastly the intensity.
So if the endurance training can be done for 15 minutes, the training frequency is increased to three to five units per week. In the next step, the training units are extended: instead of 15 minutes, the patient then trains for 30 to 45 minutes. Finally, the intensity is increased: Instead of 40% of the maximum performance, it first goes to 50 percent, then to 70 percent and then up to 80 percent.
Suitable endurance training for people with heart failure is, for example:
- (quick) walking
- Walking / Nordic walking
- jog
- Step aerobics
- Bicycling or bicycle ergometer
- Climbing stairs (e.g. on the stepper)
- swim
- rowing
Three to five units of endurance training of 15 to 30 minutes each are recommended for heart failure.
Strength endurance
Strength and resistance training is also important for those with heart failure. Because many sufferers show the so-called wasting syndrome in an advanced stage. This leads to a reduction in muscle mass and a loss of strength.
We recommend dynamic strength and endurance training with little weight and a lot of repetitions. In order to create a training plan, it makes sense to determine the so-called “one repetition maximum” (1-RM), i.e. the maximum weight for one repetition.
Ideally, the patient begins exercising at an intensity below 30 percent of the 1-RM for five to ten reps. The training is then slowly increased to 30 to 50 percent of 1-RM with 15 to 25 repetitions.
Note: Correct breathing is particularly important in this training: Despite exertion, pressure breathing is to be avoided.
Patients with heart failure should do strength and endurance training two to three times a week.
Heart failure: disease course and prognosis
Heart failure is incurable. Only in a few cases can the symptoms be reduced to such an extent that a completely unimpaired life is possible. However, each patient can influence whether and how far the disease progresses. By changing their lifestyle and dealing with the disease more carefully, those affected can do a lot to improve their prognosis.
In addition to lifestyle, it is above all compliance that patients have to consider. With therapy loyalty or compliance, the doctor describes the extent to which patients adhere to the prescribed and discussed therapy. This includes, for example, taking the prescribed medication regularly, even if there may be no symptoms at all at the moment. Complications and deterioration of the general condition can be prevented in advance.
Compliance also includes regular check-ups with the family doctor. If blood values (e.g. electrolytes, kidney values) are outside the normal range, more frequent checks are necessary.
Also important in the case of heart failure: If you suspect that your condition has worsened, see a doctor immediately!
Heart Failure: Life Expectancy
Statistically, half of all patients die within five years of being diagnosed with "cardiac insufficiency". However, life expectancy and quality of life of patients have increased in recent years due to the ever-improving medical care. Those affected now have a better prognosis and, despite the illness, still have a comparatively high life expectancy. In individual cases, this depends on the type (genesis) of the disease, the age of the person affected, possible concomitant diseases and personal lifestyle.
"Heart failure" is often stated as the cause of death on death certificates. This refers to acute heart failure, which in many cases leads to death.
Additional information
Book recommendations:
- Special volume on heart failure by the German Heart Foundation
Guidelines:
- Pocket guidelines "Heart failure" of the German Society for Cardiology (as of: 2016)
- National care guideline "Chronic Heart Failure" of the Working Group of Scientific Medical Societies (AWMF) et al. (Status: 2017)