Valvular heart disease
Clemens Gödel is a freelancer for the medical team.
More about the experts All content is checked by medical journalists.A heart valve defect is the malfunction of one or more heart valves. Such so-called valve vitia are often asymptomatic at the beginning, but if left untreated they lead to cardiac insufficiency. Doctors detect heart valve defects with an ultrasound. Treatment is done with medication and surgical procedures. Read everything about symptoms, diagnosis and therapy of the heart valve defect here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. I09I08Q22Q23I05I35I37I36I06I07I34
Valvular heart disease: description
The term heart valve defect or valve vitium is an umbrella term for an altered, leaky (insufficient) or narrowed (stenosed) heart valve. Symptoms vary depending on the heart valve affected and the type of defect.
Heart valves have a very important valve function in the flow of blood through the heart. They ensure that the blood can only flow in one direction. The heart valves are opened and closed by the pressure and flow of the blood.
Frequency of valvular heart disease
A distinction is made between congenital and acquired heart valve defects. The bicuspid aortic valve with two instead of the usual three pockets is the most common congenital heart valve defect. The majority of heart valve defects affect the left half of the heart, where the mitral and aortic valves are located.
In Europe and North America, the most common acquired heart valve disease is mitral valve regurgitation. The aortic valve stenosis, the second most common valve vitium, has to be treated more often. It usually develops in old age, due to the calcification of the valve.
Constricted heart valves (valve stenosis)
When a heart valve is narrowed, it no longer opens sufficiently. The blood accumulates in front of the valve. If a valve leading out of the heart (pulmonary valve or aortic valve) is affected, the heart muscle has to exert more force in order to empty the heart chamber against the higher flow resistance (pressure load). This increases the size of the heart muscle. In the long term - and with further progression of the heart valve defect - the pumping power is no longer sufficient and the pumping power of the heart decreases. Heart failure develops.
The two most common heart valve stenoses are aortic valve stenosis and mitral valve stenosis. Depending on the severity, a distinction is made between low, medium or high-grade heart valve stenosis.
Leaking heart valves (valve insufficiency)
In contrast, patients whose heart valves do not close tightly are referred to as valve insufficiency. Despite the closed heart valve, the blood flows back into the section where the lower pressure prevails - during the contraction phase of the heart muscle (systole) from the heart chamber into the atrium or during the relaxation phase (diastole) from the pulmonary or main artery back into the heart chamber.
As a result of the additional blood volume flowing back (volume load), the heart chamber expands (dilation) and the heart muscle becomes thicker (hypertrophy). If the valve insufficiency progresses, cardiac insufficiency also develops.
Aortic valve insufficiency (also: aortic insufficiency) and mitral valve insufficiency (mitral regurgitation) are the two most common types of heart valve insufficiency.
Heart valve prolapse
Another form of the heart valve defect is mitral valve prolapse (prolapse = incident). The closed mitral valve leaflets bulge significantly into the left atrium during the contraction of the left ventricle. This heart valve defect is one of the most common heart valve changes in adults. Mitral valve prolapse affects women slightly more often than men. Mitral valve prolapse usually does not cause any symptoms. In some cases, however, it leads to mitral regurgitation.
Some patients have multiple heart valve defects at the same time. If a single valve is leaking and at the same time narrowed, doctors speak of a combined heart valve defect or a combined vitium.
Valvular heart disease: symptoms
Symptoms depend on the severity of the valve defect as well as its location. Many heart valve defects cause no symptoms for a long time and are therefore not noticed. But there are also acute heart valve defects such as mitral valve stenosis after rheumatic fever, which cause (clear) symptoms early on.
The heart can compensate for many valve defects for a certain period of time. In the long term, however, they overload the heart and gradually lead to cardiac insufficiency. The heart valve defect is often only noticed through the symptoms of heart failure.
Overall, the symptoms of valvular heart disease are similar in stenosis and valve insufficiency. The most important signs are pressure and tightness around the sternum and fatigue quickly. Fainting spells are also possible.
Left ventricular valvular heart disease symptoms
The symptoms of heart valve defects in the left ventricle are primarily caused by a backlog of blood in the left atrium and the pulmonary vessels. Affected people usually feel more comfortable in an upright and sitting position than in a lying position.
Signs of mitral valve stenosis usually only appear when the opening of the mitral valve is roughly halved. Symptoms can be similar to chronic bronchitis. The focus is on shortness of breath during exertion and later also at rest, (nocturnal) cough, tiredness and rapid fatigue. Sometimes dizziness occurs. Typical symptoms of a long-standing mitral valve stenosis are also cardiac arrhythmias and noticeable reddish-bluish cheeks (so-called cheeks).Mitral cheek) as a sign of poor oxygen supply.
Typical signs of mitral regurgitation are shortness of breath (especially at night and when lying flat) and coughing at night. Patients experience cardiac stumbling and / or palpitations, signs of a cardiac arrhythmia, especially in advanced disease. Pulmonary edema occurs as a result of the backlog of blood in the lungs. If the blood builds up into the right ventricle, neck veins protrude. Due to the unfavorable flow conditions, blood clots can develop in the left atrium, which enter the circulation and cause serious complications (e.g. stroke).
Common symptoms of aortic valve stenosis are fluctuations in blood pressure and low blood pressure with attacks of dizziness and fainting. Since the coronary arteries are supplied with blood from the aorta, the increasingly working heart muscle receives too little blood. Patients experience pain or pressure in the chest (angina pectoris), which may increase with exertion. Difficulty breathing and sometimes muscle pain occur during exertion.
With aortic regurgitation, those affected complain of shortness of breath. One can observe a strong pulsation of the carotid artery (Corrigan's sign), which can lead to an indicated nod of the head with each heartbeat (Musset's sign). Increased pulsation of the vessels (Quincke's sign) is also noticeable in the area of the nail beds.
Right ventricular valvular heart disease symptoms
If the heart valves in the right half of the heart (pulmonary and tricuspid valves) no longer work properly as a result of heart valve defects, there is a long-term risk of right-sided heart failure. Right-sided heart valve defects only lead to noticeable symptoms when they are already well advanced. The complaints arise from the strain on the right ventricle and the right atrium, which are weakened by the extra work.
As a result, the blood can no longer be pumped into the lungs in sufficient quantities and accumulates in front of the heart. This can lead to the following symptoms:
- Shortness of breath
- Quick fatigue
- Blue discoloration of the (mucus) skin (cyanosis)
- Water retention in the legs (edema) and abdomen (ascites)
- Blood congestion in the superficial vessels of the neck
- Exercise-related pain in the chest and liver (under the right costal arch)
- Congestion in other organs such as the stomach (loss of appetite, nausea) or kidneys (risk of kidney failure)
Valvular heart disease: causes and risk factors
Heart valve defects can either be congenital or acquired. The majority of heart defects are acquired.
Congenital heart valve defects
The most common congenital heart valve defects include aortic valve stenosis and pulmonary valve stenosis. Congenital heart valve defects are often more serious than acquired damage and often develop before the eighth week of pregnancy. In addition to genetic diseases, harmful influences during pregnancy such as rubella infection, drug or alcohol consumption by the mother often cause congenital heart valve defects.
A heart valve defect in the aortic valve in younger people is usually the result of a faulty valve system. The aortic valve then only consists of two instead of three pocket valves (so-called bicuspid aortic valve).
Acquired valvular heart disease
Wear and calcification of the heart valves can lead to various heart valve defects with age. The aortic valve is particularly often calcified. Calcifications cause valve constrictions as well as leakage.
Inflammation
Infections and inflammations of the heart muscle (myocarditis) or the lining of the heart (endocarditis) sometimes also cause heart valve defects. Usually it is a heart valve insufficiency. The rarer heart valve defects in the right half of the heart are also primarily caused by infections in the inner wall of the heart.
In addition to mostly bacterial pathogens, autoimmune diseases such as systemic lupus erythematosus (PE) can lead to endocarditis (Libman-Sacks endocarditis). In its late stages, sexually transmitted syphilis sometimes causes inflammation of the main artery (aorta) that spreads to the aortic valve (syphilitic aortitis).
Rheumatic fever
Some germs can also indirectly cause a heart valve defect: For example, in rheumatic fever, the immune system reacts excessively to an infection with streptococci, a common bacterial pathogen that causes tonsillitis. Its surface resembles the body's own structures - these are, so to speak, "mistaken" for the bacterium by the immune system. One speaks of a cross reaction. Under certain circumstances, this also affects the inner wall of the heart and the heart valves.
The mitral valve is particularly often affected by rheumatic fever. Streptococcal infections are therefore treated with antibiotics for prevention, especially in childhood. As a result, cases of mitral valve stenosis, for example, are already declining in industrialized nations.
Heart attack
A heart attack also sometimes causes heart valve defects. The lack of oxygen damages the so-called papillary muscles in the heart chambers, which attach tendon threads to the large leaflet valves (mitral and tricuspid valves). If they no longer function properly or if they even tear, they no longer hold the valve leaflet attached to them. This then strikes back into the atrium during the contraction of the heart chamber. There is a risk of an acute, severe leak in the corresponding heart valve.
If the ventricle wall expands after a myocardial infarction, this may also cause a leaky heart valve defect. This also threatens with dilated cardiomyopathy, a heart muscle disease in which the heart chamber expands.
Aortic dissection
Acute aortic valve insufficiency can also result from what is known as aortic dissection. The inner wall (intima) of the main artery (aorta) tears and blood penetrates between its wall layers. Usually such aortic dissections occur in the area of the aorta close to the heart. Sometimes the wall tears up to the fibrous ring to which the aortic valve is attached. This deforms the aortic valve in such a way that it no longer closes tightly.
Cardiomegaly
Various diseases such as high blood pressure, heart muscle diseases, disorders of the thyroid function or severe anemia (anemia) can lead to abnormal heart enlargement (cardiomegaly). Since the heart valves do not grow with them, they become leaky.
Autoimmune diseases
Autoimmune diseases such as Takayasu arteritis (inflammation of the large blood vessels) or genetic disorders of the connective tissue metabolism (e.g. Marfan syndrome) also cause heart valve defects such as aortic or mitral valve insufficiency.
Valvular heart disease: examinations and diagnosis
The specialists in heart valve defects are cardiologists and cardiac surgeons. They first ask you questions like:
- Do you suffer from shortness of breath or heart pain under stress?
- How many stairs can you climb without a break?
- Have you recently had an acute fever?
- Have you recently had a medical procedure, including at the dentist?
- Are you known to have any heart disease?
- What other illnesses do you suffer from?
After that, the doctor will examine you thoroughly. He pays attention to external signs of a heart valve defect, such as changes in breathing, color and texture of the skin and any accumulations of fluid in the tissue (edema). Then he listens to heart and lungs. Heart valve defects often cause typical heart murmurs.
electrocardiogram
Heart valve defects sometimes trigger cardiac arrhythmias. For example, mitral stenosis often causes what is known as atrial fibrillation. The doctor recognizes this on the basis of an electrocardiogram (EKG). If cardiac arrhythmias occur repeatedly, but only sporadically, a long-term ECG, which the patient carries for at least 24 hours, may help.
Laboratory examination
A blood test provides, among other things, evidence of an active inflammatory process. Doctors also use it to determine (in) direct heart values, such as creatine kinase (CK) and BNP (brain natriuretic peptide). Especially if endocarditis is suspected, several blood cultures must also be taken, in which microbiologists search for bacteria. Another important blood test is blood gas analysis (from capillary blood or arterial blood). This is because the oxygen content of the blood can provide important information in the case of major heart valve defects.
Imaging examinations
If the physical examination suggests a heart valve defect, the doctor will perform a heart ultrasound ((Doppler) echocardiography). With its help, the examiner recognizes, for example, the heart contour and changes in the heart valves. He also sees - using Doppler technology - how the blood flows through the heart valves.
Some heart valve defects lead to blood congestion with water retention in the lungs. These will show up in a chest x-ray. Doctors can use it to assess the size and shape of the heart at the same time.
Detailed images are obtained by means of sectional imaging. MRT technology (cardio MRT) or computed tomography (CT) are used for this. In the case of a pure heart valve defect, however, they are rarely used.
Stress tests
Both cardiac ultrasound and ECG can also be performed under physical strain (on the ergometer or with cardiac stimulating medication). These examinations clarify stress-dependent symptoms. Heart valve defects often only show up with exertion in their early stages. So exercise tests help to assess the severity of heart valve defects.
Cardiac catheter
With the help of a so-called cardiac catheter examination, doctors measure, among other things, the pressure conditions in the heart and use contrast media to show whether coronary vessels are narrowed.
If the examiner injects contrast medium into the left ventricle of the heart (ventriculography or levocardiography), not only the shape and function of the ventricle but also possible vitia are shown.
Some heart valve defects can be "repaired" right away as part of this examination. This is one of the reasons why this invasive examination is usually at the end of the diagnosis - unless an acute vascular disease of the heart (CHD, myocardial infarction) is suspected. Doctors want to rule out these diseases with a cardiac catheter before a heart valve defect operation.
Final assessment
The detailed diagnostics allow the severity classification, which is different for each heart valve. This classification is an important basis for therapy planning. Among other things, it is important to determine the ejection fraction. This value indicates in percentages how much of the blood that has flowed into the heart chamber is pumped out again per stroke. In healthy hearts, the value is around 60 to 70 percent.
Valvular heart disease: treatment
The treatment plan for valvular heart disease depends on the type of heart valve defect, the valve affected, the severity, and also the general condition of the patient. Doctors also use measurements of heart function when choosing a therapy. All factors are individually weighed in order to work out the best therapy for the individual affected. Doctors not only want treatment to alleviate symptoms. The therapy also improves the prognosis and stabilizes the heart valve function.
Before each treatment, doctors speak to the person concerned in detail again. They mainly address the following questions:
- What is the patient's wish?
- Is it a serious heart valve defect?
- Are there any symptoms associated with the valvular heart disease?
- How old is the patient?
- Do the therapeutic benefits outweigh the risks?
- Which medical center is suitable for the procedure?
Basically there are drug, interventional and surgical therapeutic approaches. If possible, an underlying medical condition should be treated first. This applies in particular to the treatment of acute illnesses (e.g. a heart attack), infections and autoimmune diseases.
Medication
Medicines help reduce cardiac arrhythmias, lower blood pressure, increase the pumping power of the heart and prevent blood clots. To this end, doctors prescribe drugs that increase urine output in order to reduce the (volume) stress on the heart (diuretics). Other drugs lower the heart rate and thus reduce the work of the heart (beta blockers). After using heart valves made of “foreign material”, anticoagulant medication is often necessary.
Endocarditis prophylaxis
In addition, in the case of a heart valve defect, it must always be remembered that antibiotic infection prophylaxis should be carried out before medical interventions that involve the risk of infection and the resulting inflammation of the heart. For this reason, those affected should inform their treating physicians about the presence of a (treated) heart valve defect so that they can prescribe antibiotic therapy if necessary. This applies in particular to dental treatments as well as examinations and treatments in the area of the gastrointestinal tract.
Interventional treatment
In medical jargon, interventional or percutaneous procedures are interventions that are carried out very specifically and with little damage to the surrounding tissue. The differentiation from a so-called minimally invasive procedure is not always easy. In the treatment of heart valve defects, an interventional procedure means the use of cardiac catheters, as they are also used to diagnose heart valve defects.
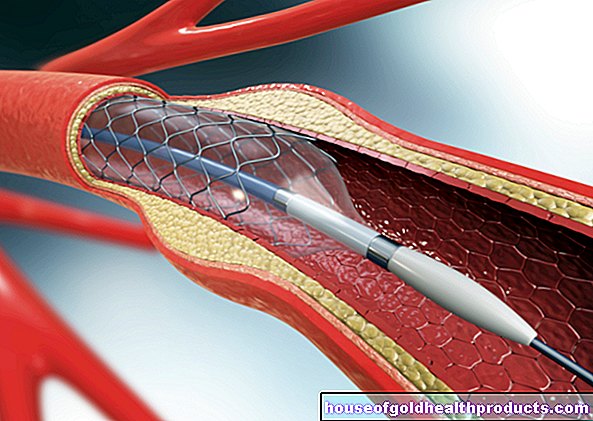
Narrowed valves can be widened, for example, with an inflatable balloon that is advanced into the heart via an inguinal vessel and the large vessels (balloon valvotomy or balloon valvuloplasty). No major surgery is then necessary, but valve weakness can occur after such an "explosion". A folded heart valve replacement can also be inserted into the heart with the help of a catheter. Only biological heart valves can be used with this procedure. However, treating a heart valve defect is not always possible with an interventional procedure.
surgery
Modern surgical procedures not only allow larger, open surgery to be carried out, but also minimally invasive operations. In a minimally invasive operation, the instruments are inserted through smaller incisions. The most common aortic and mitral valves are treated surgically.
An operation may require the use of a so-called heart-lung machine. For this purpose, the heart function is taken over by a machine during the operation. The heart can then be temporarily stopped with medication and the blood can be diverted through the machine.
When should a heart valve defect not only be treated with medication?
The right time for the procedure is not always easy to determine. On the one hand, it should not be carried out too early in order to avoid complications from the operation and, above all, the possibly necessary lifelong blood thinning. On the other hand, too late an intervention can significantly worsen the prognosis due to heart damage that has already occurred.
Heart valve replacement - different types
In the case of a heart valve defect, mechanical valves or bio-prostheses from humans or animals (heart components from cattle or pork valves) are possible valve replacements.
Metallic heart valves last a very long time. However, blood coagulation must be inhibited for life with special medication, as otherwise blood clots can accumulate on the artificial valve, block it or loosen it and lead to a vascular occlusion.
With a biological valve replacement, no “blood thinning” is necessary. For this, biological heart valves have to be replaced after a certain period of time, as their shelf life is limited. In addition to normal wear and tear, this can be due to the fact that the immune system recognizes the valves as foreign bodies and attacks them. A distinction is made between biological replacement valves from animals (xenograft), from a deceased person (homograft) and heart valves grown from stem cells of the affected person (autograft). How long such a mouth will last is difficult to predict and depends on many factors.
A new and not yet established concept of heart valve replacement for a heart valve defect is so-called tissue engineering. The idea behind this is that synthetic or biological heart valve scaffolds are overgrown with cells of the affected person after they have been introduced into the heart. This reduces interactions with the immune system and allows the valves to grow and become vital.
Choosing a new heart valve
The balance between the long service life of the prosthesis and lifelong “blood thinning” must be decided on an individual basis. As a rule, biological heart valves are only used from the age of 60 due to their limited shelf life. Metallic heart valves are more likely to be selected for younger patients or those affected who have to take blood thinners for life for other reasons. Exceptions are women who want to have children and who do not want to be prescribed anticoagulant medication.
After the use of a valve prosthesis, a valve pass should be issued, an inspection should take place at least once a year and endocarditis prophylaxis should always be considered. Endocarditis prophylaxis is the preventive administration of antibiotics in treatments that involve a risk of infection. This must also be taken into account in particular for dental interventions.
Aortic regurgitation and stenosis
The main goal of drug treatment is to reduce the stress on the heart. A purely drug therapy requires close cardiological monitoring. More often it is only carried out as a bridging measure to relieve symptoms until the operation. An aortic valve defect should be treated surgically or interventionally if symptoms worsen and cardiac function deteriorates. The procedure should take place before a significant reduction in cardiac function.
Under certain conditions, aortic valve insufficiency, as well as aortic valve stenosis, can be treated with the help of catheter technology ("TAVI": Transaortic Valve Replacement). For this purpose, a folded replacement valve is inserted into a small tube over a groin vessel through the large arteries into the heart, where the valve can be unfolded and fastened.
In a Ross operation, the aortic valve is replaced by the pulmonary valve. The much less stressed pulmonary valve is in turn replaced by a human donor valve. This method has the advantage that no lifelong blood thinning is necessary, the long-term function is very good and the physical resilience is almost unrestricted. The main disadvantage is a possible malfunction of the dispenser flap. A Ross operation can only be performed by experienced specialists.
Doctors sometimes use balloon valvuloplasty to bridge the gap until the final treatment, for example in the case of acute deterioration in the patient's condition. In doing so, they widen the valve using a balloon, which they guide on a catheter through the blood vessels to the heart. This method is also used with children. A valve prosthesis is difficult for them because it cannot grow with them.
If, in addition to the aortic valve insufficiency, there is a bulging (aneurysm) of the main artery close to the heart, this is usually treated at the same time as the valve operation (Bentall operation).
Mitral valve stenosis
Initially, mitral valve stenosis can be treated with medication. These can also relieve milder symptoms. Diuretics in particular are helpful in reducing the volume load on the narrowed mitral valve. Any existing cardiac arrhythmias should also be checked with medication. As with aortic valve insufficiency, surgery should be considered in good time in the case of mitral valve stenosis if the symptoms progress or the measured heart function is reduced.
As an interventional treatment, the valve can be widened (balloon mitral valvuloplasty). This form of valve repair with the aim of separating the fused valve edges can also be performed as part of an open operation (surgical commissurotomy). If there are contraindications, doctors replace the valve with a prosthesis.
Mitral valve regurgitation and mitral valve prolapse
The principles for treating mitral valve regurgitation are similar to those for mitral valve stenosis. Intervention for the treatment of such a heart valve defect should be performed if there are symptomatic and (or better before) signs of impaired cardiac function.
Except as bridging, drug treatment is not recommended for all forms of mitral regurgitation. A distinction is also made between repair and replacement operations in the case of mitral valve regurgitation.
Nowadays, a mitral valve repair can also be carried out as an interventional procedure. A clip (MitraClip) is inserted into the heart. The clamp is then fixed in such a way that it holds the so-called cusps of the mitral valve together and compensates for the heart valve defect.
Heart valve insufficiency or mitral valve prolapse can also be repaired as part of an operation. In the case of mitral regurgitation, a ring can be placed in the valve area to correct the heart valve defect. A gathering with special threads can reduce the flap weakness. If repair is not possible, the valve can be surgically replaced. The repair (reconstruction) is preferred to a valve prosthesis.
Special threads are also used in the case of mitral valve prolapse: the cardiac surgeons use them to sew the papillary muscle tendons to the edge of the mitral valve. Sometimes doctors first have to reduce or remove the abnormally large sail (the part that bulges) and then sew parts of it back on.
Pulmonary valve regurgitation
The rare pulmonary valve weakness is usually caused by pulmonary hypertension (pulmonary hypertension). This heart valve defect is therefore treated by lowering the high pressure in the blood vessels in the lungs. Since pulmonary valve insufficiency usually does not cause any symptoms and does not significantly limit heart function, interventions are rarely necessary. However, a valve replacement is useful, for example, if the opening area of the pulmonary valve continues to enlarge.
Pulmonary valve stenosis
Pulmonary valve stenosis can be treated with medication. If the pulmonary valve stenosis is advanced, repair or valve replacement can be performed. Interventional and surgical procedures are also available for this type of heart valve defect, such as those used in mitral stenosis (balloon expansion, surgical commissurotomy).
Tricuspid valve regurgitation and tricuspid valve stenosis
These rare heart valve disorders are treated as soon as they affect cardiovascular function. Their symptoms are usually mild. If medication does not help, the valve can be repaired first. In the case of tricuspid valve insufficiency, for example, shirring the edge of the valve and inserting a ring for stabilization (ring annuloplasty) is suitable. There is also the option of replacing the valve.
Sport for valvular heart disease
Whether and in what form sport is possible for patients with heart valve defects depends on the type of malformation. The individual condition and well-being of the patient also play a role in the sports recommendation.
Before patients with a heart valve defect start any physical activity, they should always consult their doctor.
Patients with an acquired heart valve defect should have a performance diagnosis carried out once a year during the cardiological examination. An exercise ECG can determine the maximum performance of the heart. On this basis, the doctor can decide which activities the person concerned can take up.
Whether people with a congenital heart valve defect can be physically active always depends on the individual condition of the patient. There are no general recommendations.
Course of the disease and prognosis
Heart valve defects can not only limit the quality of life, but also the life span, as the entire cardiovascular system suffers. The prognosis for heart valve defects depends primarily on which heart valve is affected and whether the heart valve defect has already impaired heart function. If left untreated, a major valve defect will lead to cardiac insufficiency over time and a poor prognosis.
Mild heart valve defects often do not initially require an operation, but still require treatment. It is important to check a detected heart valve defect regularly (at least annually). The heart specialist checks how well the previous treatment is working and whether he needs to take new measures. Take advantage of these examinations, because they can improve the prognosis for heart valve defects in the long term.
Tags: dental care elderly care pregnancy