Ependymoma
Ricarda Schwarz studied medicine in Würzburg, where she also completed her doctorate. After a wide range of tasks in practical medical training (PJ) in Flensburg, Hamburg and New Zealand, she is now working in neuroradiology and radiology at the Tübingen University Hospital.
More about the experts All content is checked by medical journalists.The ependymoma is a very rare tumor in the brain or spinal cord. It forms in the cerebral waterways and often causes increased intracranial pressure with headaches and nausea. Mostly children around the age of 6 are affected. The tumor is operated on or irradiated. The prognosis depends on various factors and varies greatly. Here you can read everything you need to know about ependymoma.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. D43C71D33

Ependymoma: description
The ependymoma is a tumor that can form both in the brain and in the spinal cord. Most often children are affected in the first ten years of life. The ependymoma makes up ten percent of all brain tumors in childhood and is therefore the third most common tumor of the central nervous system in this age group. Every year around two in a million children develop ependymoma. But adults can also develop this tumor, albeit much less often: In them, the ependymoma only makes up two to three percent of all brain tumors.
An ependymoma is formed from ependymal cells. These line the inner wall of the cerebral chambers (ventricles) and the spinal canal (spinal canal), in which the cerebrospinal fluid (liquor) is located. In principle, the tumor can form anywhere on these inner walls. In children and in all age groups, however, it occurs preferentially in the 4th ventricle of the posterior fossa. From there, the ependymoma often spreads towards the cerebellum, brain stem, or upper cervical medulla. An ependymoma in the spinal canal is more common in adults.
Metastasis
In certain cases, individual tumor cells can secrete and reach another location such as the spinal cord via the cerebral waterways. If they grow at this new location and multiply there, one speaks of a metastasis. Some scientific studies assume that about two percent of all ependymomas develop metastases, others speak of about 30 percent. If the ependymoma returns after successful therapy (relapse), it metastasizes in almost every second patient.
WHO classification
The World Health Organization (WHO) divides ependymoma like all other brain tumors into different degrees of severity:
- Grade I: subependymoma and myxopapillary ependymoma
- Grade II: ependymoma
- Grade III: anaplastic ependymoma
The subependymoma is a benign tumor. It bulges out into the inner chambers of the brain and is often only discovered by chance.
The myxopapillary ependymoma is also benign. It grows exclusively in the lowest part of the spinal canal and occurs in adults.
Anaplastic ependymoma is most common in children. It grows very quickly and has a poor prognosis because it grows into the adjacent tissue - in contrast to the 1st and 2nd degree tumor types, which are usually well demarcated from healthy brain tissue.
Ependymoma: symptoms
Because of its close proximity, an ependymoma can very quickly obstruct the cerebral waterways. But if the brain water no longer drains properly, the pressure on the brain increases. This causes severe headaches that can hardly be relieved by medication. Most of the time, the headache occurs at night or in the early hours of the morning and gets better as the day progresses. They return regularly and become more and more intense over days and weeks. If the intracranial pressure continues to rise, those affected are often nauseous. Some have to pass over. In extreme cases, they can become tired and sleepy or even go into a comatose state.
Especially in younger children, the head circumference can increase due to an ependymoma (macrocephalus). In some patients, the tumor manifests itself as a seizure. In addition, you may experience discomfort when walking, seeing, sleeping and concentrating. An ependymoma can also cause paralysis.
Ependymoma: causes and risk factors
Why an ependymoma develops has not yet been definitively researched. People who have been irradiated as part of cancer therapy have an increased risk of developing the disease. Children are sometimes irradiated with leukemia (white blood cancer) or the malignant eye tumor retinoblastoma and as a result develop a brain tumor more often years after the irradiation.
Ependymomas in the spinal cord are associated with the hereditary disease neurofibromatosis type 2.
Ependymoma: examinations and diagnosis
Patients with symptoms of brain cancer often go to their family doctor or pediatrician first. He asks about the exact complaints and their course, any previous and underlying illnesses and the general state of health (collection of the medical history = anamnesis). If he finds evidence of a malignant tumor in the central nervous system, he usually refers the patient to a specialized center for cancer (oncology) for further examinations. Doctors from different disciplines work together there to make the correct diagnosis. Various technical examinations are usually necessary for this.
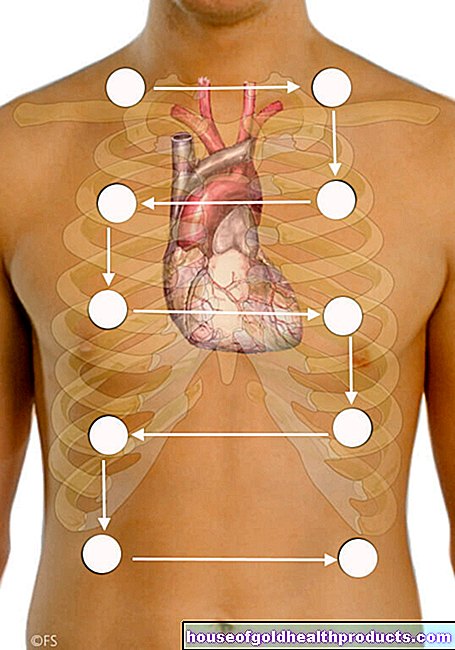
The best way to visualize an ependymoma is magnetic resonance imaging (MRI). Most often, a contrast agent is injected into a vein of the patient before the examination. The tumor absorbs this contrast agent and lights up irregularly in the MRI image. This allows you to determine its location, size and extent very well.
The cerebral fluid examination (liquor diagnosis) supplements a detailed diagnosis of the ependymoma. Individual tumor cells can be detected here. In addition, a tissue sample is usually taken from the tumor and examined under a microscope. This is necessary in order to be able to optimally tailor the subsequent therapy to the patient.
Ependymoma: treatment
The first therapeutic step in an ependymoma is the surgical removal of the tumor as completely as possible.With tumors in the spinal cord, this goal can often be achieved nowadays. Tumors in the brain, on the other hand, can usually not be completely removed. If remnants of the tumor remain in the body or if the tumor has already spread, radiation therapy follows. In the case of a second or third degree ependymoma, this is also carried out after the tumor has been completely removed. This can reduce the risk that the tumor will recur. Chemotherapy is rarely carried out in studies for ependymoma. It is controversial whether it brings a decisive advantage.
Symptoms of the tumor such as headache or nausea are treated with medication. In the case of an ependymoma, therapy with cortisone preparations is also an option. They cause the brain tissue to swell and in this way reduce existing intracranial pressure.
Examination and treatment
You can read more information on examinations and therapy in the article on brain tumors.
Ependymoma: disease course and prognosis
The prognosis for an ependymoma depends on various factors and can therefore be very different. Among other things, the decisive factor is where the tumor is located, whether it can be completely removed surgically and whether it has already spread.
If the tumor region is completely removed with re-irradiation, 60 to 75 percent of patients are still alive five years later and 50 to 60 percent still live ten years later - prerequisite: the disease does not progress. If the ependymoma could not be completely removed and those affected received re-radiation, the 10-year survival rate is only 30 to 40 percent.
Tags: toadstool poison plants medicinal herbal home remedies interview