HPV vaccination
and Martina Feichter, medical editor and biologistFlorian Tiefenböck studied human medicine at the LMU Munich. In March 2014, he joined as a student and has supported the editorial team with medical articles ever since. After receiving his medical license and practical work in internal medicine at the University Hospital Augsburg, he has been a permanent member of the team since December 2019 and, among other things, ensures the medical quality of the tools.
More posts by Florian TiefenböckMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
The HPV vaccination (colloquially: cervical cancer vaccination) is the most effective protection against infection with the human papillomavirus, which can cause cervical cancer. The Standing Vaccination Commission (STIKO) recommends the HPV vaccination for all girls and boys between nine and fourteen years of age before the first sexual activity. Read more on the topic: How does the HPV vaccination work? How often and when is it given? What are the risks? Who pays for the HPV vaccination?
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. A63B07
HPV vaccination: what is it?
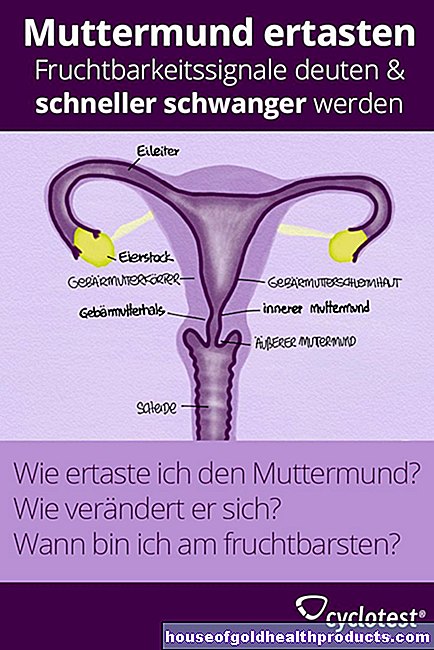
The HPV vaccination is a vaccination against human papillomavirus. These are considered to be the most important risk factor for cervical cancer. They can also trigger or promote other diseases, such as other forms of cancer or genital warts.
Two types of HPV vaccine
Two types of vaccine are available in Germany for the HPV vaccine: a double vaccine (bivalent HPV vaccine) and a nine-fold vaccine (nine-valent HPV vaccine). A quadruple vaccine was also available until August 2017, but it was replaced by the nine-fold vaccine (the two come from the same manufacturer).
- The double HPV vaccine protects against infection with the high-risk HPV types 16 and 18. These are responsible for 60 to 70 percent of all cervical cancer cases.
- The nine-fold HPV vaccine not only protects against HPV 16 and 18, but also against other high-risk types (31, 33, 45, 52 and 58) as well as against the low-risk types HPV 6 and 11. All of these virus types together are for 75 to 90 percent of all cervical cancers are responsible. The two low-risk types 6 and 11 are also considered to be the main causes of genital warts (genital warts).
Since the HPV vaccination reduces the most important risk factor for cervical cancer, it is colloquially also called "cervical cancer vaccination" or "vaccination against cervical cancer". However, this term is incorrect because the vaccination does not directly prevent cancer.
Both HPV vaccines contain proteins from the shell of the virus (capsid). The immune system forms special antibodies against these proteins. These enable a quick and targeted defense if a person comes into contact with the actual pathogen after the vaccination.
For whom is the HPV vaccination useful?
The Standing Vaccination Commission (STIKO) recommends the HPV vaccination for all girls and boys between nine and fourteen years of age. Missed vaccinations should be made up at the latest by the age of 18 (i.e. by the last day before the 18th birthday). For girls, vaccination against HPV is of course useful to protect against cervical cancer. Find out below why it is also advisable for boys.
Whether girls or boys - if possible, the HPV vaccination should take place before the first sexual intercourse, as you can get infected with HPV during your first sex - and also when petting!
The vaccination recommendation for girls has been in effect since 2007. The HPV vaccination for boys has been recommended since 2018.
Why the vaccination recommendation for boys?
Of course, only women can develop cervical cancer. Nevertheless, vaccination against HPV - the most important risk factor for this malignant tumor - makes sense not only in girls but also in boys, for several reasons:
- The HPV vaccination can reduce the risk of penile and anal cancer as well as tumors in the mouth and throat (oral sex!). As in cervical cancer, human papillomaviruses can be involved in the development of these types of cancer.
- The nine-fold vaccine against HPV not only protects girls / women from genital warts, but also boys / men.
- If men or boys are protected against infection with human papilloma viruses thanks to the HPV vaccination, they cannot pass such viruses on to their sexual partners. This means that girls also benefit when boys receive the HPV vaccination.
HPV vaccination for adults?
In women and men aged 17 and over who have not yet received an HPV vaccination, it can sometimes make sense to get one. Doctors decide this on a case-by-case basis: They will weigh up the benefits of the HPV vaccination and the risks that can be expected for the respective adult.
For example, some young adults have never had sexual intercourse. Then the vaccination against HPV can still develop its full effect at this age.
Under certain circumstances, the HPV vaccination can also be useful for an already sexually active adult - for example if someone has already been infected with HPV 16 but not yet with other HPV viruses that are contained in the vaccine (such as the high-risk type HPV 18 ). Then the HPV vaccination can at least protect the person against infection with these types of viruses.
When may / should not be vaccinated?
If hypersensitivity to ingredients of the vaccine is known, the HPV vaccination should not be administered.
In the case of acute, severe, febrile illnesses, the vaccination against HPV must be postponed.
How does the HPV vaccination work?
For the HPV vaccination, you can contact a pediatrician, general practitioner or gynecologist, for example. The vaccine is given by injection into a muscle (preferably in the upper arm).
A two-dose vaccination scheme is recommended for girls and boys between the ages of 9 and 14: For the primary vaccination, two doses of the HPV vaccination are given, at least five months apart. If there is less than five months between the two doses of the HPV vaccination, a third vaccination dose must be given after a few months to complete the primary series.
Three vaccination doses are also required for the basic vaccination if the HPV vaccination series is only started from the age of 15.
The schedule for the individual vaccine doses varies slightly depending on the HPV vaccine used. The intervals that should be between the individual doses also depend on whether two or three vaccine doses are planned. In any case, the vaccination series should be completed within one year.
During a series of vaccinations, one should stick to the same HPV vaccine. So if the double HPV vaccine was started, the vaccination series should also end with this. Thereafter, one could theoretically carry out another series of vaccinations with the nine-fold HPV vaccine (as protection against the additional types of virus it contains). The benefit of this is unclear, however.
Refreshing?
It has not yet been conclusively clarified whether the HPV vaccination will have to be refreshed at some point after a complete basic immunization. Previous study results indicate that girls and women are still vaccinated 12 years after vaccination.
HPV vaccination: effectiveness
The effectiveness of the HPV vaccination has been examined in numerous studies. In summary, both HPV vaccines significantly reduce the risk of infection with the high-risk virus types that are most frequently involved in the development of cervical cancer (HPV 16 and 18). The nine-fold vaccine also protects against other types of HPV that can cause cervical cancer.
Whether and to what extent a widely used HPV vaccination can actually reduce cervical cancer can only be estimated: Both vaccines have not been used long enough (on average, there is an interval of 10 to 30 years between infection with HPV and the occurrence of cervical cancer ).
Protection against other cancers as well as genital warts
All of the main types of HPV at risk for cervical cancer contained in the vaccine can also cause malignant changes in other sites (such as the vagina or anus). The vaccination also protects against this.
The nine-fold vaccine also prevents infection with the main causes of genital warts (HPV 6 and 11). The double vaccine does not offer this protection.
The effectiveness of the HPV vaccination depends on whether a girl or boy has an HPV infection at the time of vaccination. HPV viruses can be infected with the first sexual activity. Therefore, if the HPV vaccine is already given to sexually active girls or boys, it is less effective.
No substitute for preventive examinations!
As effective as the HPV vaccination can be, it still does not offer 100 percent protection against the causes of cervical cancer (or other malignant growths). Therefore, all women and girls who are vaccinated against HPV should still go to the gynecologist for cancer screening examinations on a regular basis.
HPV vaccination: side effects
Both types of HPV vaccination for girls and boys are generally well tolerated. However, as with all drugs, side effects are always possible. They hardly differ between the two HPV vaccines and usually go away on their own after a short time:
|
Side effects |
Dual HPV vaccine |
Nine-fold HPV vaccine |
|
Very often |
- Skin reactions at the injection site (redness, pain, swelling) - Headache - Muscle pain - tiredness |
- skin reactions at the injection site (redness, pain, swelling) - Headache |
|
Frequently |
- gastrointestinal complaints such as nausea, vomiting, diarrhea and abdominal pain - Itching, rash, hives - joint pain - Fever |
- nausea - Dizziness - exhaustion - Fever - Itching and bleeding at the injection site |
Sometimes you also get other side effects, such as joint pain (nine-fold vaccine), swollen lymph nodes, or fainting in response to the injection (both vaccines).
With both types of HPV vaccination it can also happen that the vaccinated person has an allergic reaction to it (for example with swelling of the face and / or breathing problems). Then you should see a doctor immediately!
HPV vaccination: possible deaths?
In the past there have been reports of isolated deaths after the HPV vaccination (about one in Germany and one in Austria). So far, however, it has not been proven in any case that the vaccination was responsible for the death of those affected.
Since the HPV vaccines were approved, international authorities have been reviewing reports of suspected vaccine side effects. Several million vaccine doses have now been administered worldwide. For reasons of chance alone, it is therefore to be expected that deaths or serious illnesses will occur again and again after a vaccination. So far, however, it has never been proven that the vaccination was responsible.
HPV vaccination: cost
The statutory health insurance companies pay for the HPV vaccination for girls and boys between the ages of nine and fourteen years and also for missed vaccinations up to their 18th birthday. As a rule, this is also done by private health insurance companies. It is best to ask your insurance company in advance.
As for the HPV vaccination for adults: Some health insurance companies also cover the costs. Here, too, it is worth asking.
HPV vaccination in short supply: who will get it?
Vaccines may become scarce. This is the case, for example, in times of crisis: a certain vaccination can no longer be properly produced and delivered due to acts of war. You can read about what doctors do when these supply bottlenecks affect HPV vaccines in our article Vaccine Shortages.
Tags: interview gpp Baby Child





















.jpg)