Liver cancer
and Martina Feichter, medical editor and biologist Updated onDr. med. Julia Schwarz is a freelance writer in the medical department.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Liver cancer is a malignant tumor in the liver. Most often it is liver cell cancer, which often develops as a result of cirrhosis of the liver. It usually only causes symptoms such as upper abdominal pain and unwanted weight loss in an advanced stage. Liver cell cancer affects men more often than women. Read more about this type of tumor and other forms of liver cancer here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. C22C24
Liver cancer: description
Liver cancer is a malignant disease of the liver. This organ performs many tasks in the body:
- The liver uses the nutrients absorbed from the intestines. For example, it stores excess sugar (glucose) in the form of glycogen. Certain vitamins and iron are also stored in the liver when the body doesn't need them.
- The organ is involved in controlling the sugar, protein and fat metabolism.
- The liver produces the bile that is necessary for the digestion of fat in the intestines.
- It produces the factors for blood clotting as well as the starting materials for the formation of sex hormones and the body's own fats.
- As the central detoxification organ, the liver converts and breaks down pollutants, drugs, alcohol and certain endogenous substances. The breakdown of old red blood cells also takes place here.
These tasks are vital for the body. A liver disease such as liver cancer can have a correspondingly serious impact. The malignant tumor occurs when cells in the liver degenerate so that - instead of performing their tasks - they begin to multiply in an uncontrolled manner and displace healthy tissue in the process. The functioning of the liver increasingly suffers as a result.
Different types of malignant liver tumors
Malignant tumors within the liver can have different origins. Accordingly, a distinction is made between primary and secondary liver tumors.
Primary liver tumors
A primary liver tumor has its origin directly in the liver - doctors speak of liver cancer here. Depending on which cells degenerate, different forms of liver cancer result. These include:
- Liver cell cancer (hepatocellular carcinoma, HCC): In the vast majority of cases, primary liver tumors are hepatocellular carcinoma - a malignant tumor that arises from degenerated liver cells (hepatocytes).
- Intrahepatic cholangiocarcinoma (iCC): This primary liver tumor develops from the bile ducts within the organ and is more common in women than men. Bile duct cancer can also develop from bile ducts outside the liver and is then called extrahepatic cholangiocarcinoma (eCC).
- Hemangiosarcoma of the liver: This rare form of liver cancer starts in the walls of the blood vessels in the liver. Such a malignant blood vessel tumor can develop not only in the liver, but also in other parts of the body.
Secondary liver tumors
Secondary liver tumors are liver metastases, i.e. settlements (daughter tumors) of a cancerous tumor in another region of the body. This original tumor (primary tumor) is often located in the lungs, breast, uterus, prostate, or gastrointestinal tract. Individual cancer cells of the primary tumor can reach the liver via the blood and settle there. In Europe, such liver metastases are more common than liver cancer.
Only liver cancer is treated below!
Frequency of liver cancer
Liver cancer is relatively rare in Europe: According to the World Health Organization (WHO), 58,079 men and 29,551 women were newly diagnosed with it in 2020. The disease occurs predominantly in old age.
In many European countries and the USA, the incidence of liver cancer has increased significantly over the past 35 years. The reasons for this are probably the increasing number of cases of cirrhosis of the liver, obesity and diabetes mellitus as well as the many new cases of hepatitis C in the 1960s, 1970s and 1980s - all of which are risk factors for liver cancer.
Liver cancer: symptoms
You can find out which symptoms can express liver cancer in the article Liver Cancer - Symptoms.
Liver cancer: causes and risk factors
The exact causes of liver cancer are not yet fully understood. However, there are numerous known risk factors that favor the development of (primary) liver cancer. There are differences between the different types of primary liver cancer. Here are the most important:
Hepatocellular Carcinoma Risk Factors
Cirrhosis of the liver
Liver cell cancer develops in more than 80 percent of cases as a result of shrunken liver (cirrhosis of the liver). The main causes of liver cirrhosis and thus of liver cell carcinoma are:
- chronic inflammation of the liver caused by hepatitis C or hepatitis B viruses
- chronic alcohol consumption
- Non-alcoholic fatty liver (develops mainly as a result of being very overweight and / or type 2 diabetes mellitus)
A chronic hepatitis B infection and a non-alcoholic fatty liver can also lead directly to liver cancer - without liver cirrhosis as a "detour".
With liver cirrhosis, liver tissue increasingly dies and becomes scarred (liver fibrosis). The liver tries to compensate for the progressive loss of functional tissue by forming many new liver cells - cell division is thus stimulated. Because errors in the genetic code can occur every time a cell divides, this increases the risk that cancer cells will develop. Therefore, liver cell cancer is a common consequence of liver cirrhosis.
Substances toxic to the liver (hepatotoxins)
Various toxins can also cause liver cancer, such as aflatoxins. These are very potent, cancer-causing (carcinogenic) toxins that are produced by the mold (Aspergillus flavus). The fungus often colonizes nuts and grains when they grow under poor conditions (drought) and are then stored moist. Liver cancer caused by mold toxin is significantly more common in tropical-subtropical countries than in Europe.
Other hepatotoxins that can promote liver cell carcinoma are, for example, the semimetal arsenic and the toxic gas vinyl chloride (raw material for polyvinyl chloride, PVC).
Iron storage disease (hemochromatosis)
The congenital disorder of iron metabolism also increases the risk that liver cancer will develop from degenerate liver cells: In hemochromatosis, the body deposits excessive iron in the body, including in the liver. The increased iron content damages the tissue in the long term and can cause liver cirrhosis - as mentioned above, a major risk factor for liver cell cancer.
Intrahepatic Cholangiocarcinoma (iCC) - Risk Factors
Chronic biliary inflammation, which can have various causes, increases the risk of bile duct cancer inside (and outside) the liver. For example, biliary tract cancer often occurs in patients with primary sclerosing cholangitis (PSC). This is a chronic, autoimmune-related inflammation of the bile duct.
Other possible triggers of chronic bile duct inflammation and thus a risk factor for bile duct cancer are chronic infections, for example with typhoid bacteria, hepatitis B or hepatitis C viruses, HIV or various parasites (such as the Chinese liver fluke).
Hemangiosarcoma of the liver - risk factors
This type of liver cancer is mainly caused by exposure to various toxins. For example, the vinyl chloride mentioned above can promote not only liver cell carcinoma but also malignant vascular tumors. In other cases, hemangiosarcomas turn out to be long-term damage to the previously used X-ray contrast agent Thorotrast or as a result of radiation damage.
Anabolic steroids, which some athletes and bodybuilders misuse to build muscle, represent another risk factor for a cancer tumor originating from the blood vessels.
Liver cancer: examinations and diagnosis
The right person to contact if you suspect liver cancer is your family doctor or a specialist in internal medicine and gastroenterology.
In people with certain risk factors for liver cancer (such as liver cirrhosis, chronic hepatitis B or C infection), regular examinations for the early detection of liver cancer can be useful.
Medical history and physical examination
At the beginning, the doctor will collect your medical history in a detailed discussion (anamnesis). He will ask you to describe your symptoms to him in detail and ask you about your general state of health, your lifestyle and any underlying illnesses. Possible questions in this regard are, for example:
- Are you known to have chronic inflammation of the liver (hepatitis) or cirrhosis of the liver?
- Have you made trips abroad to Asia or Africa in the last few years?
- How much alcohol do you drink every day? Were there times in life when you drank more?
- Do you have frequently changing sexual partners? (-> Increased risk of hepatitis B and C)
The conversation is followed by a physical examination: In liver cancer, the liver may be so enlarged that the doctor can feel it under the right costal arch. In cirrhosis of the liver - the most important risk factor for liver cancer (more precisely: liver cell cancer) - the liver surface is typically bumpy and irregular. That can also be felt.
As a rule, the doctor also taps the stomach with his fingers (percussion). In this way, he can determine whether there is water in the abdomen (ascites = ascites). This is often the case with severe liver diseases such as liver cancer.
Based on the medical history and physical examination, the doctor can already roughly assess whether there is possibly liver cancer. However, further examinations are always necessary for a reliable diagnosis.
Blood tests
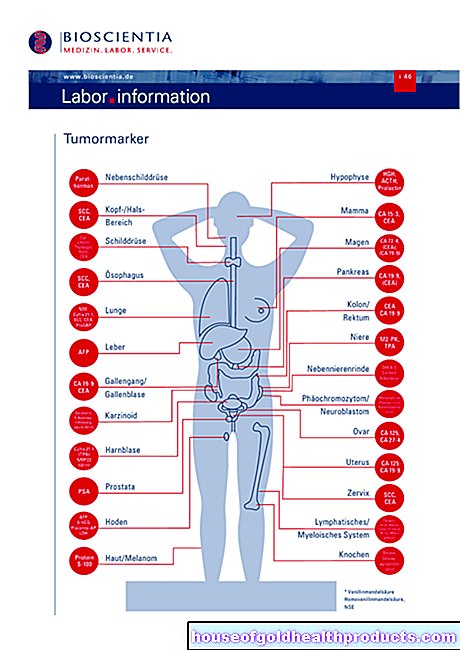
Blood tests if liver cancer is suspected are primarily used to detect a hepatitis infection and so-called tumor markers. Tumor markers are substances that are increasingly formed by tumor cells. In the case of liver cell cancer - the most common form of liver cancer - the alpha-1-fetoprotein (also: alpha-fetoprotein, AFP) is increased in the blood. However, the AFP level alone does not allow a reliable diagnosis: On the one hand, it is often not increased in the early stages of liver cancer. On the other hand, an increased AFP level can also have reasons other than liver cancer. These include, for example, virus-related liver inflammation (viral hepatitis), liver cirrhosis, testicular tumor and pregnancy.
The AFP value is more important for monitoring progress than for diagnosing liver cancer.
Various liver values are also measured in the blood as general parameters of liver function. These include liver enzymes (such as AST / GOT and ALT / GPT), liver synthesis parameters (vitamin K-dependent blood coagulation factors, albumin, cholinesterase) and, typically, elevated values (gamma-GT, AP, bilirubin) in biliary congestion.
Imaging procedures
An ultrasound examination (sonography) enables an initial assessment of the condition of the liver. It can make structural changes in the organ and possibly a tumor visible. Clearer images are obtained by administering a contrast agent (contrast-enhanced ultrasound, CEUS).
In addition, magnetic resonance imaging (magnetic resonance imaging, MRI) and / or computed tomography (CT) are often used. They provide more detailed images than a normal ultrasound - especially if the patient is given a contrast agent during the examination, as is usually the case.
MRI and CT not only help to clarify suspected liver cancer, but also to look for any daughter tumors (metastases) in other parts of the body.
The importance of the various imaging procedures depends on the individual case. If, for example, liver cell cancer (hepatocellular carcinoma) is suspected in patients with liver cirrhosis, an MRI with contrast agent administration is recommended as an imaging diagnostic method.
If an MRI cannot be performed (e.g. for patients with a cardiac pacemaker) or if it provides an unclear finding, a computed tomography (CT) and / or a contrast-enhanced ultrasound examination (CEUS) is used for diagnosis.
biopsy
Sometimes liver cancer can only be diagnosed with certainty if a tissue sample is taken and examined under a microscope in the laboratory. The tissue sample is taken by means of a puncture: the doctor, under ultrasound or CT control, inserts a fine hollow needle through the abdominal wall into the liver and thereby extracts tissue from the suspect area. The patient receives a local anesthetic for the procedure so that he does not feel any pain.
Liver cancer: classification according to spread
Like other tumor diseases, liver cancer is divided into different stages according to the UICC (Union internationale contre le cancer). The classification depends on the spread of the tumor. This, in turn, is defined using the so-called TNM classification: T stands for tumor size, N for lymph node involvement (Latin: nodus) in the tumor area and M for metastases (daughter settlements) in more distant body regions (distant metastases). The classification can be used to describe exactly how far a tumor has spread to the surrounding tissue. The staging according to UICC thus depends directly on the TNM classification.
TNM classification in liver cancer:
Tumor size (T):
- T1: A single (solitary) tumor that has not yet invaded blood vessels.
- T2: Solitary tumor with vascular involvement or several (multiple) tumors with a maximum diameter of five centimeters.
- T3: Several tumors with a diameter of more than five centimeters or tumors with involvement of a larger branch of the portal vein and the hepatic vein.
- T4: tumor (s) with involvement of adjacent organs or tumor (s) with perforation of the peritoneum.
Lymph nodes (N):
- NX: Lymph node involvement cannot be assessed.
- N0: Lymph nodes are not affected by cancer cells.
- N1:. Lymph nodes are infected with cancer cells.
Distant metastases (M):
- MX: distant metastases cannot be assessed.
- M0: No distant metastases.
- M1: Distant metastases present (e.g. in the lungs).
UICC stages:
|
UICC stadium |
TNM classification |
|
Stage I. |
Up to T1 N0 M0 |
|
Stage II |
Up to T2 N0 M0 |
|
Stage III |
Up to T4 N0 M0 |
|
Stage IVa |
Each T N1 M0 |
|
Stage IVb |
Every T, every N and from M1 |
Liver cancer: treatment
Liver cancer therapy depends on several factors, including the stage of the cancer, the age, and the general condition of the patient. Various treatment methods are available, which can be used alone or in different combinations:
An operation offers the chance to cure the liver cancer patient by removing the diseased part of the liver (partial resection) or the entire liver. In the second case, the patient receives a donor liver (liver transplant) as a replacement.
In most cases, however, liver cancer is too advanced for surgery by the time it is diagnosed. Instead of an operation or to bridge the time until the liver transplant, local measures that destroy the tumor (local ablative therapy methods) can be considered.
If liver cancer cannot be completely eliminated either surgically or locally ablatively, patients can be treated with transarterial (chemo- or radio-) embolization and / or medication. Sometimes high-precision radiation therapy (high-precision radiotherapy) can also be considered. The aim of these treatments is to slow down tumor growth and extend the survival time of those affected.
Surgery / liver transplant
In liver cancer, the surgeon tries to surgically remove the affected liver tissue as completely as possible. In the case of a small tumor, it is usually sufficient to remove part of the liver (partial liver resection). Since the liver generally has great potential for regeneration, up to 85 percent of the liver tissue can be surgically removed. As long as the remaining 15 percent of the liver is healthy and fully functional, the liver can continue to do its job. The remaining healthy liver cells gradually replace the removed tissue.
If the liver cancer has spread to so many areas of the organ that a partial surgical resection is no longer possible, the entire organ can possibly be removed and replaced with a donor liver. However, such a liver transplant is only considered for a few patients because various prerequisites have to be met. For example, the tumor must be limited to the liver and must not have formed any daughter tumors (liver cancer metastases) - for example in lymph nodes.
Local ablative procedure
There are several local ablative methods of treating liver cancer. Here are the most important:
In radiofrequency ablation (RFA, RFTA, RITA), the doctor inserts a probe into the malignant tumor under ultrasound or CT guidance. The tumor tissue is then heated to over 100 degrees Celsius using radio frequency waves. In this way, tumor areas with a diameter of up to three to five centimeters can be destroyed. If there are several tumor foci, several sessions are usually necessary. They are each carried out under short anesthesia.
With microwave ablation (MWA), too, the tumor tissue is locally heated and thus destroyed. However, even higher temperatures (up to 160 degrees) are used here than with radio frequency ablation (RFA).
Another locally ablative therapy method for liver cancer is percutaneous ethanol or acetic acid injection (PEI). The doctor injects alcohol (ethanol) or acetic acid through the abdominal wall into the affected area of the liver. Both substances cause the cancer cells to die. The surrounding healthy tissue, on the other hand, is largely spared. The percutaneous ethanol or vinegar injection is usually repeated in several sessions at intervals of several weeks.
Experts recommend radiofrequency or microwave ablation as a local ablative procedure for the treatment of liver cell cancer (hepatocellular carcinoma). Percutaneous injections of ethanol or acetic acid have proven to be less effective than RFA, for example.
Transarterial (chemo-) embolization (TAE / TACE)
Embolization is the targeted closure of blood vessels. As part of liver cancer therapy, this can be done with the vessels that supply the tumor with blood:
Through an access in the inguinal arteries, the doctor pushes a flexible cannula (catheter) up to the hepatic artery under X-ray control. Each liver tumor is supplied with oxygen and nutrients through one or more branches of this artery. In the next step, the doctor injects small plastic particles into these vessels via the catheter, thereby closing them - the cancer cells, which are now cut off from the blood supply, die.
This therapy method is called transarterial embolization (TAE). It can be combined with local chemotherapy: the doctor also injects an active ingredient into the vicinity of the tumor via the catheter, which kills cancer cells (chemotherapeutic agent). Then one speaks of transarterial chemo-embolization (TACE).
Transarterial radio embolization (TARE)
This procedure is often called Selective Internal Radiotherapy (SIRT). It is a new type of local radiation treatment from the inside. It can be considered if liver cancer cannot be surgically removed and has not yet formed any daughter settlements:
Again, a catheter is inserted through the groin into the hepatic artery. The doctor then uses this catheter to insert numerous tiny, radioactive spherules into the vessels that supply the tumor. This has two effects: On the one hand, the vessels are closed so that the tumor is cut off from the blood supply. On the other hand, the cancer cells are exposed to a high local dose of radiation that kills them.
High precision radiotherapy
In high-precision radiotherapy, a high dose of radiation is directed very precisely from the outside onto a precisely defined area of the body - the tumor or a metastasis. The procedure is also called stereotactic radiation ("Stereotactic Body Radiotherapy", SBRT). It can be considered when other local therapies for the treatment of liver cancer are not possible.
Medication
Targeted drugs
In 2007, sorafenib, the first targeted drug for the treatment of liver cancer, was approved. It is a so-called multi-kinase inhibitor: By blocking certain enzymes, it delays the growth of the tumor and the blood vessels supplying it. Sorafenib can be prescribed for advanced liver cancer.
In addition to sorafenib, other enzyme inhibitors (multi-kinase and tyrosine kinase inhibitors) are now available for liver cancer therapy, including regorafenib and lenvatinib.
Combination therapy with the artificially produced monoclonal antibodies atezolizumab and bevacizumab is an option for certain patients with liver cell cancer. Atezolizumab inhibits a protein (PD-L1) produced by cancer cells, which ensures that the body's immune system does not act against the tumor cells. By blocking PD-L1, atezolizumab can lift this "brake" on the immune system so that the body can act more effectively against the malignant cells.
Bevacizumab specifically inhibits the growth factor VEGF. This is produced by tumors in order to stimulate the formation of new blood vessels - for a better supply of the tumor. By inhibiting VEGF, bevacizumab can reduce the supply and thus the growth of the malignant tumor.
The active substance ramucirumab is another monoclonal antibody that can be given in certain cases of liver cell cancer. It occupies certain binding sites (receptors) of the growth factor VEGF and thus blocks its effect.
Treatment with targeted drugs is only considered for selected patient groups.
Systemic chemotherapy
Against many cancers, doctors use systemic (= affecting the whole body) chemotherapy - drugs that generally inhibit the growth of rapidly dividing cells (such as cancer cells).
Such chemotherapy is not used as standard in adults with liver cell cancer because it is generally of little effect here. In individual cases, however, it can be considered, for example in the end-stage liver cancer as a pain-relieving (palliative) measure. The course of liver cancer cannot be stopped entirely, but it can at least be slowed down.
In contrast to adults, children and adolescents with liver cell cancer respond well to systemic chemotherapy in almost half of all cases. That is why it is standard in the treatment of this group of patients.
Liver cancer: disease course and prognosis
Whether liver cancer is curable depends on the stage of the disease: the earlier the disease is detected, the better the liver cancer prognosis.
However, the malignant tumor is often only discovered at an advanced stage. The therapeutic options are then limited. As with most tumor diseases, the following applies to liver cancer: life expectancy and chances of recovery are poor if the diagnosis is made later. At this point in time, the cancer cells have already spread to other organs and formed daughter tumors (liver cancer metastases). In the most common form of liver cancer - hepatocellular carcinoma (liver cell cancer) - five years after diagnosis, an average of 15 percent of the affected women and men are still alive (five-year survival rate).
Liver cancer: prevention
If you want to prevent liver cancer, you should avoid the known risk factors (see above) if possible:
- Drink only moderate amounts of alcohol or, if you have chronic liver disease (cirrhosis, chronic hepatitis, etc.), no alcohol at all. The luxury food can cause massive damage to the liver and cause liver cirrhosis within years - a significant risk factor for the development of liver cancer.
- Eat a balanced, low-fat diet with plenty of fresh vegetables and fruits as well as grains and whole foods. This will not put excessive strain on the liver. In addition, such a diet - together with regular physical activity - prevents obesity and diabetes, two other risk factors for liver cancer.
- Don't eat moldy foods (such as cereals, corn, peanuts, or pistachios). These belong in the garbage - just removing visibly infected parts is not enough. The mold has long formed invisible threads that run through the food.
- It is also advisable not to use tobacco. The consumption of cigarettes etc. is also associated with an increased risk of liver cancer.
- People with chronic liver disease should drink coffee because it can counteract the progression of scarring (fibrosis) in the liver in these patients and lower the risk of liver cancer (more precisely: liver cell cancer). The effect seems to be most pronounced with a coffee quantity of three or more cups a day.
- In addition, the proper treatment of chronic liver diseases (such as cirrhosis, hepatitis B or C) is important in order to reduce the risk of liver cancer.
- The hepatitis B vaccination (HBV) protects against liver inflammation caused by hepatitis B viruses. It is recommended by default for all infants from 2 months of age. It is also advisable for certain risk groups. Read more about it here.
- To date, there is no vaccine to prevent hepatitis C. However, other measures (e.g. not sharing drug equipment such as syringes) can reduce the risk of hepatitis C infection and thus of liver cancer.
- If possible, patients with non-insulin-dependent diabetes should be treated with the blood sugar lowering drug metformin. It reduces the risk of liver cancer (more precisely: liver cell cancer) in those affected.





-mit-mickymaus-am-tannenbaum.jpg)