Lipedema
and Carola Felchner, science journalistClemens Gödel is a freelancer for the medical team.
More about the expertsCarola Felchner is a freelance writer in the medical department and a certified training and nutrition advisor. She worked for various specialist magazines and online portals before becoming a freelance journalist in 2015. Before starting her internship, she studied translation and interpreting in Kempten and Munich.
More about the experts All content is checked by medical journalists.Lipedema is a disorder of fat distribution in the legs and / or arms. Often water is also stored in the affected tissue (edema). Lipedema occurs almost exclusively in women. It is treated with conservative measures (such as physiotherapy) and surgical procedures. Read everything you need to know about the topic here: How can you recognize lipedema? How does lipedema develop? Which doctor is the right one for diagnosis and treatment? What can be done about fat distribution disorder?

Lipedema: Brief Overview
- Symptoms: symmetrical increase in fat tissue on the legs (and / or arms), pressure and tension pain, tendency to bruise
- Therapy: Physiotherapy (e.g. lymph drainage, compression); Liposuction (in severe cases and when other therapies are ineffective)
- Cause: not clearly clarified; hormonal and genetic reasons are suspected;
- Prognosis: no cure possible; With the right therapy, however, the symptoms can be alleviated and the progression of the disease can be stopped;
- Responsible specialist: dermatologist, vein specialist (phlebologist), lymph specialist (lymphologist)
Lipedema: symptoms
With lipedema, there is an increase in fat tissue on the extremities. The legs are affected in most patients. That is why laypeople sometimes speak of saddlebag syndrome. But there are also patients in whom lipedema develops on the arms (especially the upper arms). Occasionally, both arms and legs are affected. Very rarely, other parts of the body develop lipedema (abdomen, etc.).
Lipedema is almost always symmetrical, which means that both legs and / or both arms are affected. Side differences are extremely rare.
Lipedema of the legs can also include the buttocks evenly. However, the feet are left out. The hands are also spared in the case of lipedema on the arms. A so-called "fat collar" can be noticed at the transition between the lipedema and the hands or feet.
Lipedema can or does not have to occur in connection with general obesity. But it is also often observed in very slim women. So lipedema has nothing to do with the body's constitution!
The lipedema swelling is usually soft. It can hardly be reduced by raising your legs (or arms). This is different from edema (accumulation of water in the tissue).
Inflammations and infections can develop in the skin folds that arise from the increase in fatty tissue.
In the subcutaneous fatty tissue of the affected extremities, small nodules can often be felt, which can become larger as the disease progresses. In the later stages, so-called dewlaps (fat flaps) are formed.
-
Lipedema: "Swimming relieves"
Three questions for
Dr. med. Michael R. Schmidt-Kulbe,
Aesthetists -
1
Cellulite or lipedema - how do I tell the difference?
Dr. med. Michael R. Schmidt-Kulbe
Lipedema is a fat distribution disorder that occurs symmetrically. Legs and arms appear very voluminous, hands and feet as well as the core of the body remain slim. Cellulite usually occurs on the back of the thigh and only spreads further forward from there to the inside and outside of the thighs as it progresses. In the case of cellulite, the connective tissue is damaged and the fat deposits underneath appear visually.
-
2
Lipid edema is painful. What can you do?
Dr. med. Michael R. Schmidt-Kulbe
Pressure pain is common in lipedema. They stem from the fact that the fat cells press off small blood vessels and promote water retention. Lymphatic drainage, compression stockings, and exercise can alleviate the symptoms. This will reduce the congestion in the tissue. Swimming, for example, is good, it is similar to a massage and is also gentle on the joints. If you are overweight, losing weight also helps relieve the pain because the joints are relieved.
-
3
When does liposuction make sense?
Dr. med. Michael R. Schmidt-Kulbe
Generally speaking, only from a very advanced stage. Liposuction is the only way to permanently improve the symptoms. However: health insurances do not pay them! You have to reckon with at least 5,000 euros for the treatment. The advantage: then you have up to ten years of rest. Before having an operation, however, one should first have exhausted the possibilities of conservative therapy.
-
Dr. med. Michael R. Schmidt-Kulbe,
AesthetistsDr. med. Michael R. Schmidt - Kulbe is an aesthetic medicine specialist and has been heading the "Center for Aesthetics and Anti-Aging" in Berlin since 2007.
Lipedema: pain and bruising
Important lipedema symptoms are also a feeling of tension and pain in the affected areas of the body, such as the legs. These can feel heavy and hurt especially after long periods of standing and walking. Patients also often report pain to touch and pressure. Lipedema pain can be so severe, especially in the later stages of the disease, that those affected move less and are significantly restricted in everyday life.
Lipedema symptoms also include an increased tendency to bruise: Even minor injuries cause a "bruise". But there is no coagulation disorder in the whole body. Presumably, the vessels in the affected tissue are more vulnerable. This means that bruises form faster than other people.
The lipedema progresses
Lipedema is a progressive disease. This means that the lipedema symptoms increase if left untreated: a first-degree, mild lipedema can develop into an advanced lipedema with a large increase in adipose tissue.
This is emotionally very stressful for many of those affected. Many patients feel increasingly uncomfortable in and with their body. Self-esteem suffers, and anxiety and depression can develop. Especially when the diagnosis is made late and those affected are incorrectly diagnosed as (self-inflicted) overweight, this can put a lot of strain on the psyche. The usually lengthy treatment can also contribute - especially if it does not lead to success.
Differences from other diseases
Often the symptoms of lipedema are confused with the signs of other diseases. For example, being very overweight (obesity = obesity) can cause similar symptoms. The same applies to lymphedema and lipohypertrophy: Lymphedema occurs when fluid and protein accumulate in the tissue because the transport via the lymphatic system is disturbed. Like lipedema, lipohypertrophy is caused by a local increase in adipose tissue. But it never causes pain for those affected.
The following table lists the most important differences between lipedema, lymphedema, lipohypertrophy and obesity:
Lipedema |
Lymphedema |
Lipohypertrophy |
obesity |
|
Symmetrical increase in fat tissue on both legs and possibly on the buttocks (and / or on both arms). Feet and hands are left out. Otherwise, the person concerned is usually slim. So the body looks clearly disproportionate (disproportion). |
Asymmetrical (one-sided) increase in adipose tissue. If a leg or arm is affected, the foot / hand is usually also affected. Body looks slightly out of proportion. |
Symmetrical increase in fat tissue on both legs (and buttocks). Body looks clearly disproportionate. |
Excess fat deposits more or less all over the body. Normal or slightly uneven body proportions. |
|
With water retention in the tissue (edema). |
With water retention in the tissue (edema). |
No water retention in the tissue (edema). |
Water retention in the tissue (edema) possible. |
|
Pressure pain. |
No pressure pain. |
No pressure pain. |
No pressure pain. |
|
Significant tendency to bruise. |
No tendency to bruise. |
Risk of bruising. |
No tendency to bruise. |
The individual clinical pictures can also occur in combination. For example, if someone has lipedema and obesity at the same time, the two symptoms mix.
Lipedema: treatment
Lipedema treatment is difficult and controversial. To date, the cause of the disease is not known. The lipedema cannot be treated causally and also cannot be cured. The course of the disease can, however, be mitigated - through conservative and / or surgical therapy methods.
The goal of lipedema treatment is to relieve the patient's symptoms, especially pain. It also aims to prevent the disease from progressing and complications from occurring. In addition, all factors that favor lipedema should be reduced. Above all, these include:
- Obesity
- Water retention in the tissue (edema)
- mental stress
Lipedema: physiotherapy
The conservative treatment of lipedema is based on physiotherapeutic measures. The umbrella term for this treatment method is "complex physical decongestion therapy" (KPE). It is particularly promising in the case of simultaneous lymphedema (lipolymphedema).
The therapy includes manual lymph drainage in the form of scooping, turning and pump handles. The therapist first performs this on the trunk away from the lipedema in order to generate suction, and then also in the area of the lipedema itself.At the beginning, manual lymphatic drainage can be planned for one hour a day for three to four weeks.
Immediately after each session, the affected area should be wrapped or a compression stocking should be put on. This compression treatment reduces lipedema only slightly. However, it can slow down the progression and prevent lymphedema from developing as a result of lipedema.
There are other physical therapy procedures that can help with lipedema. This includes, for example, shock wave therapy. It improves blood circulation in the tissue. Some patients also receive what is known as intermittent pneumatic compression. In this process, alternating low and high pressures are exerted on the affected area.
Inpatient physiotherapy is often recommended for patients with severe lipedema.
Massage and elevation of the legs usually hardly improve the lipedema symptoms. They also rarely prevent the disease from progressing.
Lipedema: Sport supports therapy
If you have lipedema, you should exercise and exercise regularly. Although this cannot reduce the number of fat cells, it still makes sense: Physical activity ensures that you remain mobile and agile - many patients avoid any activity because of the pain. Exercise therapy is particularly important if lipedema occurs together with severe obesity.
Tip: Choose a sport with a low risk of injury and smooth, steady movements (no heavy braking). For example, swimming, aqua aerobics, fast walking and cycling are suitable.
Water aerobics can help
Lipedema: Diet has little direct influence
Many people think that lipedema is simply the result of excessive weight gain and that it can be eliminated by losing weight. But that's not true. A strict diet therefore hardly helps against lipedema and can even do harm: If you fixate on saving calories, although it does not make the lipedema go away, this can have a negative effect on the course of the disease and the mental health of the patient. Experts even suspect that a number of lipedema patients may have an eating disorder (such as anorexia) at the same time.
There is also no special lipedema diet that helps against the symmetrical increase in fat tissue on the legs and / or arms. Lipedema patients should simply eat a balanced, healthy diet. This generally promotes health. If you are overweight at the same time, a healthy diet can also help to shed excess pounds. Patients can get tips from their nutritionist.
More conservative measures
Lipedema treatment also includes skin care. It prevents inflammation and infection in the affected skin area. Therefore, you should always apply lotion to the skin so that it does not become dry and cracked. Small injuries should be treated immediately to prevent them from becoming infected or infected.
Psychological support for the patient is an important part of holistic lipedema therapy. Many patients suffer from depression, anxiety and / or eating disorders. Those affected should definitely receive psychological help.
Lipedema: liposuction
Lipedema can be treated surgically with liposuction. Diseased subcutaneous fatty tissue is permanently removed. The procedure is carried out, for example, if the symptoms persist or even increase despite conservative lipedema therapy (such as physiotherapy). Even if the subcutaneous fatty tissue continues to increase despite consistent conservative treatment, liposuction is indicated.
Liposuction is not a method to get rid of excess pounds if you are overweight!
Liposuction can improve the symptoms of most patients over many years. Above all, the pain and the tendency to bruise can be reduced by the procedure - as can the circumference of the affected extremities. In addition, many of those affected do not need any more conservative measures (e.g. compression) after liposuction, or at least to a lesser extent than before.
In the case of pronounced lipedema and lipolymphedema, large, flabby bags of tissue can remain after decongestion therapy and weight reduction. Then a special plastic surgical procedure (dermolipectomy) can be more useful than liposuction.
Procedure of liposuction
Liposuction for lipedema should only be performed at specialized centers - either on an outpatient or inpatient basis. The doctor uses a cannula to inject a large amount of a special irrigation fluid into the lipedema tissue. This so-called tumescent solution contains, among other things, a local anesthetic, table salt and adrenaline. It is then sucked out of the tissue along with a lot of fat. This technique is also called "wet" liposuction. It can be supported by a water jet or vibration:
- Water jet-assisted liposuction (WAL): After administering the Tumszens solution, the fat is removed with a fan-shaped water jet and suctioned off.
- Vibration liposuction: The suction cannula is set in vibration. Since fat cells are slower than blood vessels and nerve cells, they are loosened and sucked out.
After the procedure, patients should get back on their feet quickly (mobilization) and receive physical therapy. In this way, swelling, which often occurs after liposuction, can be avoided or reduced.
A maximum of around five liters can be removed in one session. In severe cases, several sessions are usually necessary to significantly reduce lipedema.
As with any surgical procedure, (severe) side effects are also possible with liposuction. Among other things, the lymphatic system can be injured. Secondary lymphedema can develop as a result.
Liposuction is not always paid for by health insurance companies. Then patients have to pay for the costs themselves.
Lipedema: causes and risk factors
Lipedema occurs when subcutaneous fat tissue increases locally: the fat cells enlarge and multiply. In addition, more or less much water is stored. This is an ongoing process. The affected area of the body can increase in size over time.
The exact causes of lipedema are not known. But experts have some guesswork. For example, the hormonal system and genetic predisposition seem to be decisive in the development of lipedema. At the same time, according to current knowledge, there is no evidence that an incorrect diet, too little exercise or other types of “misconduct” can cause lipedema.
Hormones
The importance of (female) hormones in the development of lipedema is supported by the fact that women are almost exclusively affected, especially in phases of hormonal changes. That would be during and after puberty, pregnancy and menopause. Above all, the hormone estrogen is ascribed an important role in the development of lipedema. Fat cells react to estrogen through special docking points (receptors) on their surface.
In the few men with lipedema, a hormonal disorder can always be detected. This also suggests that hormones are involved in the development of lipedema. For example, some of the men affected have a liver disease that disrupts hormone metabolism (for example, cirrhosis of the liver due to chronic alcohol consumption). Others suffer from a lack of testosterone or growth hormone or are receiving hormone therapy (for example for prostate cancer).
The hormonal changes and disorders lead to imbalances in the internal weight control of the body, the nerves in the adipose tissue and also to inflammatory processes.
Genetic predisposition
Often several members of the same family develop lipedema. This suggests a genetic predisposition. Presumably, genes that are important for the construction of blood vessels play a role in the development of lipedema.
Vascular damage
In addition to the adipose tissue disorder, an inflammatory malfunction of the vessels in the subcutaneous tissue of the patient is also suspected in the case of lipedema. The vessels in the affected area are said to have “leaks” that promote the transfer of fluid into the tissue. This also makes you more prone to bruising and can contribute to the pain.
Lipedema: examinations and diagnosis
The diagnosis of lipedema is often not easy. There are many other diseases that cause similar symptoms. In addition, some doctors are not very familiar with the clinical picture of lipedema. This is why lipedema is not diagnosed at all in some people or is diagnosed at an advanced stage. If you suspect lipedema, you should therefore contact a specialist. These include dermatologists and vein and lymph specialists (phlebologists and lymphologists).
Doctor-patient conversation
First, the doctor will talk to you in detail to collect your medical history (anamnesis). Possible questions from the doctor are:
- Do you have pain, a feeling of tension or heaviness in the affected area of the body?
- Are you prone to bruising in the affected area?
- How long have you had these symptoms? Have they changed over time?
- Do you take hormone preparations (men and women) or are you in a phase of hormonal changes (women, e.g. menopause)?
- What have you done so far against the strong increase in fatty tissue (weight loss attempts, sport, etc.)
- Are there any similar cases in your family?
The doctor may also ask you about your mental health, for example whether you have anxiety, eating disorders, or depression. Answer it honestly to the doctor. This will make diagnosis easier and help the doctor choose the right treatment for you.
Physical examination
Together with the findings from the conversation, a targeted physical examination is usually sufficient for the doctor to be able to make the lipedema diagnosis. The symmetrical increase in fat tissue on the extremities with an otherwise slim trunk provides a clear indication.
In addition, in advanced lipedema (arms, legs) there is a kind of “fat collar” over the ankles or ankles. This is followed by a so-called caliber jump from the thick arms / legs to the relatively narrow hands / feet, which are spared from the proliferation of fatty tissue. However, this does not apply if there is lymphedema in addition to lipedema (lipolymphedema).
The so-called Stemmer symbol is used to differentiate between lipedema and lymphedema, for example on the leg. It is positive if no folds of skin can be lifted off the forefoot. In the case of lymphedema, this is not possible due to the tension caused by the stored lymph. In the case of lipedema, on the other hand, it does: The skin on the foot (on the hand) can be lifted off a little. But be careful: Since there are also mixed forms of lipedema and lymphedema, a negative Stemmer sign does not rule out lipedema!
The doctor carefully inspects the affected area and pays attention to skin changes. For example, he checks whether the skin in the affected area of the body is taut and whether lumps in the subcutaneous tissue can be felt. The affected area is usually very painful and easily vulnerable. In addition, inflammation and infections can develop in the skin folds in particular in the case of lipedema.
Finally, the doctor makes a note of exactly which changes are noticed where in your body and how pronounced these are. During follow-up examinations, he can see how the disease is developing in you. The doctor will also measure your weight and height, calculate your body mass index (BMI) and determine the circumference and volume of your arms and legs to monitor the progress. It is also useful to calculate the ratio of waist size to hip size or height.
Lipedema classification
Lipedema can be classified according to various criteria:
According to the location of the lipedema, doctors differentiate the thigh type, whole-leg type, lower leg type, upper arm type, whole arm type and forearm type. Many patients also have mixed images (such as thigh and upper arm types).
According to the structure and surface of the skin (morphology), a distinction is made between the following three lipedema stages:
- Lipedema stage 1: smooth skin surface, evenly thickened and homogeneous subcutaneous tissue
- Lipedema stage 2: uneven, predominantly wavy skin surface; knot-like structures in the subcutaneous tissue
- Lipedema stage 3: pronounced increase in circumference in the affected body area with overhanging body parts (dewlaps)

In addition to lipedema, lymphedema can develop at any stage. This is favored by factors such as being very overweight (obese) and lack of exercise.
Imaging and functional studies
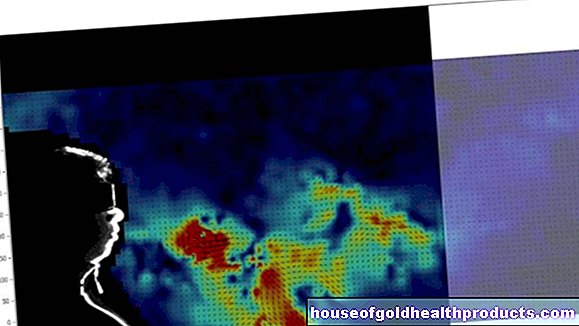
Imaging exams are not required to diagnose lipedema. Experienced examiners can, however, examine the affected region with ultrasound in order to assess the size of the lipedema and the condition of the blood vessels.
With special examinations, the doctor can assess your lymphatic system more precisely. These include so-called (functional) lymphoscintigraphy and indirect lymphangiography. This allows lymphedema to be diagnosed or ruled out.
Magnetic resonance imaging (MRI) or computed tomography (CT) is only performed in isolated cases in lipedema patients.
Alternative diagnoses
As mentioned in the Symptoms section, there are a number of conditions that are similar to lipedema. The distinction is not always easy. A specialist can therefore best differentiate between lipedema and other possible causes of your symptoms. These differential diagnoses include:
- severe overweight (obesity)
- Lymphedema
- Lipohypertrophy
- Lipoma (circumscribed, encapsulated and harmless fat tumor)
- Phlebedema (edema caused by weak veins)
- other forms of edema such as myxedema (edema-like swelling of the subcutaneous tissue due to a thyroid disease)
- Dercum's disease (obesity dolorosa)
- Madelung syndrome (increase in fat tissue in the neck and neck area, around the shoulder region or in the pelvic area)
- Fibromyalgia (chronic rheumatic disease with severe muscle pain)
Lipedema: disease course and prognosis
Lipedema is a chronic, progressive disease. Their course cannot be generally predicted. It is largely dependent on additional illnesses such as obesity.
If lipedema has been found, it should always be treated. In this way you can prevent it from progressing and (further) reducing the quality of life of the person affected. According to current knowledge, a cure for lipedema is not possible. With modern therapy methods, however, the symptoms of the disease can be significantly alleviated in many patients and the fat distribution disorder can be alleviated.
In contrast to other diseases such as vascular changes or other forms of edema, lipedema alone does not increase the risk of chronic wounds (ulcers) or blood clots (thrombosis).
Additional information:
Book recommendations:
- Lipedema: Recognize in good time and treat it correctly. Effective help without surgery (Dr. med Thomas Weiss, 2015, southwest)
Guidelines:
- S1 guideline "Lipedema", German Society for Phlebology (as of 2015)