Lymphedema
Sabine Schrör is a freelance writer for the medical team. She studied business administration and public relations in Cologne. As a freelance editor, she has been at home in a wide variety of industries for more than 15 years. Health is one of her favorite subjects.
More about the experts All content is checked by medical journalists.Lymphedema is swelling under the skin that is caused by impaired lymphatic drainage: the fluid from the intercellular spaces can no longer be sufficiently transported away via the lymphatic system, so that it builds up - a swelling occurs. Lymphedema can be congenital or develop over a lifetime. Read more about the causes, diagnosis and treatment of lymphedema here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. Q82I89I97

Brief overview
- Description: swelling in the tissue due to congested lymphatic fluid; Differentiation between congenital (primary) and acquired (secondary) lymphedema; the latter is much more common
- Symptoms: visible swelling, but decreasing due to elevation up to extreme, irreversible swelling as well as skin changes (growths, inflammations, poorly healing wounds)
- Causes: In congenital lymphedema, malformations of the lymphatic system. In acquired lymphedema, operations and radiation as part of cancer therapy or the tumor itself
- Diagnosis: taking the medical history (anamnesis), physical examination (palpation, Stemmer sign, box toe), possibly scintigraphy
- Treatment: Elevation, combination of compression therapy, lymphatic drainage, exercise training and skin care; rarely surgery
Lymphedema: description
Lymphedema is one of the most common types of edema. The swelling usually occurs in one part of the body (regional lymphedema) - the leg or arm are often affected. The swelling can appear on one or both sides.
Much less often it extends to the whole body. Doctors then speak of generalized lymphedema. For example, it is the result of a congenital malformation of the lymphatic vessels.
Lymphedema can be congenital (primary) or acquired (secondary):
- Primary lymphedema is rare. About one to ten percent of all lymphedema is congenital, which does not mean that all primary lymphedema shows up from birth. Rather, the accumulation of fluid develops later and depending on how pronounced the disorders in the lymphatic system are. Women are affected significantly more often than men. Congenital lymphedema usually begins in areas that are far from the center of the body. For example, thick, cuboid toes (box toes) with rough skin on the top are typical.
- Secondary lymphedema is much more common (at least 90 percent) than congenital. Initially, they usually develop close to the body - for example from where the damage (surgery, radiation, etc.) to the lymphatic vessels took place - and from there they spread to the limbs.
Lipo-lymphedema is a special form of lymphedema.The lymphedema develops on the basis of lipedema - a swelling as a result of a pathologically altered fat distribution. If the lipedema is not treated, this can block the lymphatic drainage in the long term and thus trigger lymphedema.
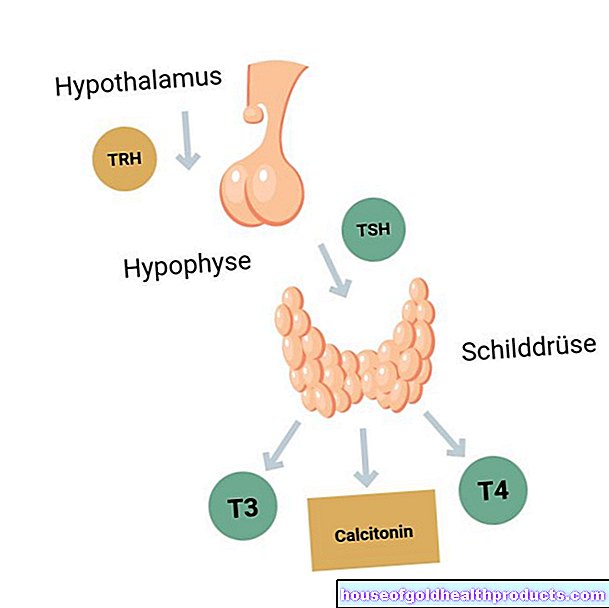
The lymphatic system
A finely branched network of lymph vessels runs through the body. It basically fulfills three important functions.
Drainage of the lymph
They divert protein-containing fluid (lymph) from the spaces between cells in the tissue. The finest lymphatic channels (lymph capillaries) unite from there to form increasingly larger lymph vessels and ultimately form lymph trunks. Via the last section, the lymph ducts, the lymph finally reaches the so-called venous angle between the cervical and clavicular veins (venous angle, left and right) and thus back into the bloodstream.
In order to transport the lymph, the lymph vessels contract. Muscles and joints act as pumps for the lymphatic vessels and thus support the evacuation of the fluid. In addition, the lymph vessels as well as the veins have valves that facilitate further transport.
Defense function
Before the tissue water flows back into the bloodstream, it usually passes through several lymph nodes. There it is cleaned of pathogens. The lymphatic system is therefore an important part of the body's defenses.
Transport of blood lipids
The fats absorbed in the intestine easily reach the lymph capillaries, which are open in the tissue and usually have patchy walls. They then reach the bloodstream via the lymphatic system. This fatty lymph is also called chyle (the fats are absorbed and transported as chylomicrons, chylos is Greek and means table juice).
lymph
The lymph is a white-yellowish liquid and, depending on the exact protein and fat content, clear to cloudy. During the day, around two to three liters of lymph fluid develop in the interstitial spaces. The fluid comes from the blood capillaries - for example, through increased pressure that forces the fluid out of the blood vessels. About ten percent of this interstitial fluid then drains off as lymph.
Development of lymphedema
In the case of lymphedema, more fluid enters the tissue than flows off via the lymphatic system - the lymph accumulates, which causes the tissue to swell. The accumulation of fluid in the tissue space increases the distance between the cells and the fine blood vessels. As a result, these can no longer supply the cells with sufficient nutrients, which can cause the cells to perish. Lymphedema must therefore be treated as early as possible to avoid major damage.
Lymphedema: stages and symptoms
Depending on the severity, doctors divide lymphedema into four stages:
- Lymphedema stage 0: With latent (invisible) lymphedema, those affected do not yet have any symptoms. Parts of the lymphatic system are already damaged, but the healthy part can still take over the removal of the lymph.
- Lymphedema stage 1: The lymphedema can now be recognized by a visible swelling, but it is still reversible - the lymphedema can regress, for example, by elevating the extremity. The swelling is soft and can be pressed in with a finger. If you take your finger away, a dent remains temporarily. In addition, the so-called Stemmer's mark is negative for diagnostics: wrinkles can be lifted on the back of the fingers and toes.
- Lymphedema stage 2: Due to the accumulated, protein-rich tissue fluid, additional connective tissue has already formed (fibrosis) and hardened (sclerosis). As a result, dents can no longer be pressed in, and even elevating affected limbs does not allow the swelling to subside. Stemmer's sign is positive - a fold of skin cannot be lifted on either the back of the finger or the back of the toe.
- Lymphedema stage 3: This stage is also known as elephantiasis. It is characterized by extreme swelling. More connective tissue has formed under the skin. The skin is thickened and hardened, wart-like growths complete the picture. Third-stage lymphedema symptoms also include discoloration or impaired nail growth. In addition, the skin's barrier function is disrupted. chronic inflammation. This promotes bacterial infections (e.g., erysipelas). In general, the skin in the affected area is extremely sensitive and wound healing is severely impaired.
Lymphedema: causes
Doctors differentiate between congenital (primary) lymphedema and acquired (secondary) lymphedema.
Causes of Primary Lymphedema
Primary lymphedema is based on congenital malformations of the lymphatic system. For example, there are too few lymph vessels or lymph nodes are missing. In other cases, the lymph vessels are narrowed, hardened, or widened.
The undesirable developments can be hereditary (hereditary). However, non-hereditary (sporadic) undesirable developments of the lymphatic system are more common. However, both are based on changes in the genetic make-up that lead to the incorrect development of the lymphatic system.
Causes of Secondary Lymphedema
Secondary lymphedema is often the result of surgery and radiation as part of cancer therapies. The tumor itself can also be the trigger for the formation of secondary lymphedema (malignant lymphedema).
Lymphedema after surgery or radiation therapy
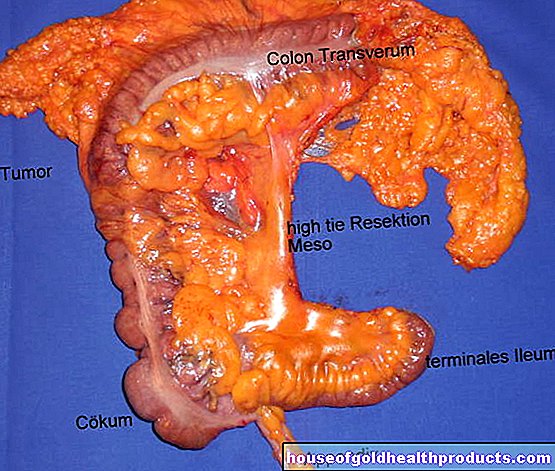
When a tumor is surgically removed, the nearby lymph nodes are often removed as well. The procedure can impair the drainage pathways in such a way that they can no longer remove the lymph and result in secondary lymphedema.
Radiation therapy for cancer can also affect the lymph nodes and vessels. The same applies to major surgical interventions, for example after a serious accident.
Malignant lymphedema
Secondary lymphedema without surgery or radiation occurs when a cancerous tumor compresses or completely destroys the existing lymphatic tract. The result is what is known as malignant lymphedema.
Lymphedema: diagnosis
If you notice symptoms of lymphedema, you should consult a doctor. He will examine you in detail and initiate the appropriate treatment.
First, the doctor asks you about your medical history (anamnesis):
- Do your parents also struggle with lymphedema?
- When did you first notice the swelling?
- Does the edema regress, for example by lying up?
When answering questions, the doctor also goes into your previous illnesses and asks about operations that may have recently been carried out.
Physical examination for lymphedema
The doctor then examines the affected part of the body and looks for typical swellings and skin changes. By feeling the edema, he can determine whether the tissue is soft or has already hardened.
Stemmer's sign provides further information: The doctor lifts the skin on the fingers or the tops of the toes. If no crease remains, this indicates lymphedema in an advanced stage (2-3) (positive Stemmer's sign). Sometimes the doctor also uses an ultrasound to show the extent of the lymphedema and possible flow obstacles.
Lymph scintigraphy
If after these examinations there are still doubts as to whether it is actually lymphedema, a lymph scintigraphy can provide final certainty. In this nuclear medicine examination method, the doctor (or his assistant) injects a radioactively marked active ingredient (tracer), which can only be removed via the lymphatic system. This removal can be represented graphically.
In this way, the doctor can clearly identify disorders in the lymphatic drainage. Examining the lymphedema in this way takes about an hour. Sometimes the doctor makes later recordings after several hours in order to be able to assess the course over time.
Depending on the suspected cause, further examinations follow, for example a magnetic resonance tomography with contrast agent (contrast medium MRI) or a genetic diagnosis.
Lymphedema: treatment
Most of those affected are preoccupied with one question: Can lymphedema be cured? The answer to this is: With the right treatment, the pathological swellings can at least be reduced well.
Conservative treatment
Experts recommend a combination of compression therapy, lymphatic drainage, exercise training, and skin care. It can be helpful to treat lymphedema with home remedies. The focus here is on a balanced diet and sufficient exercise.
It is also important to know that the treatment of lymphedema is time-consuming, especially at the beginning, and not always easy. In addition, the treatment may be with you for a lifetime. With your cooperation, however, you will prevent complications such as severe inflammation. In addition, a slightly improved lymphedema often makes your everyday life easier.
Compression therapy
With the help of compression stockings or armbands, slight pressure is applied to the lymphatic vessels. This makes it easier to remove the accumulated tissue fluid in the legs or arms.
Lymphatic drainage
This is a special massage technique that can decongest the tissue. It is therefore also called manual or physical decongestion therapy. Lymph drainage is one of the recognized remedies and is paid for by health insurance companies according to a doctor's prescription. Mostly perform specially trained physiotherapists performed.
Exercise training
Targeted movement trains the muscles, which, like a pump, support the lymph vessels in the removal of tissue fluid. The exercises are individually tailored to the patient in the physiotherapy practice. For example, a person with lymphedema on the leg receives different exercises than a patient whose arm is affected.
Skin care
Since the skin can suffer badly from lymphedema, it is important to care for it and keep it supple. It is advisable to regularly apply moisturizing lotions to the affected areas of the skin.
Deep oscillation and other measures
The currently valid guidelines also assign deep oscillation a decongestant and pain-relieving effect. However, the investigations relate to a specific device that has to be handled correctly in order to be able to help.
There is currently no evidence showing that these methods work and benefit the patient for further measures against lymphedema such as thermotherapy, soft lasers or lymph tapes.
Medicines and food supplements
There are currently no drugs that work directly against lymphedema. The use of appropriate preparations only makes sense in the event of complications such as pain or infections. Hydrochloric drugs (diuretics) usually do not help either. On the contrary: Excessive use can even promote lymphedema!
Lymphedema, which is caused by infection with certain roundworms, the filariae, has a special position. Doctors counteract this so-called lymphatic filariasis with special drugs such as diethylcarbamazine or ivermectin.
Food supplements can be useful in some cases of secondary lymphedema, especially if a blood test reveals the deficiency of certain substances. Studies have shown that selenium, for example, can support the conservative therapy of some lymphedema. However, uncontrolled selenium intake can also lead to an overdose and corresponding health problems. You can find out more about this in our article on selenium.
Before taking any supplements, talk to your doctor. Experts generally recommend a previous blood test.
Lymphedema surgery
Sometimes conservative measures do not help to control lymphedema. Then surgical intervention can be useful. However, experts only recommend this if there is no malignant lymphedema - i.e. fluid accumulation due to cancer - and the patient is not unnecessarily endangered by the operation.
Surgeons operate on lymphedema differently depending on the cause. If you want to restore the lymphatic drainage as naturally as possible, you usually use one of these three methods:
- Microsurgical autogenous lymphatic vessel transplantation: For lymphedema in which the pathways are interrupted. Here the surgeons transplant lymph vessels from a healthy region of the body.
- Interposition of autogenous veins: Against lymphedema, in which the lymph vessels are damaged over a short distance and no other lymph vessels are available or are less accessible. The surgeons use the body's own vein sections to bridge the gap.
- Flap surgery: displacement of healthy tissue adjacent to the lymphedema, including its lymph vessels
Doctors may also transplant entire lymph nodes from a healthy region to the damaged one. If all veins are well connected, it can also help to connect the lymph vessels with veins (lympho-venous, lymphonodulo-venous anastomoses) - i.e. before the lymph ducts naturally lead the lymph into the bloodstream in the vein angle.
Sometimes liposuction also works against pronounced lymphedema. Lymphedema that is particularly advanced is surgically reduced. Surgeons cut out the affected skin, underlying fatty tissue and the muscular skin to varying degrees and seal the surgical area with a skin graft or a flap, for example.
Lymphedema: self-treatment with home remedies and other tips
To support medical treatment, many people with lymphedema keep an eye on their diet: Losing excess weight can help keep lymphedema in check. In addition, experts suspect that a balanced, low-salt diet is also useful for lymphedema.
However, the general benefit of a special diet for lymphedema has not yet been scientifically proven. According to currently valid guidelines, a special diet, such as the MCT diet (MCT = medium-chain triglycerides), can only help in very rare malformations of the lymphatic system with high-fat lymph and protein loss.
Decongestant breathing exercises as well as self-massage have been shown to have an effect on many lymphedema. Your physical therapist will tell you exactly how the two methods work.
Tags: sports fitness desire to have children pregnancy