Tonsillitis
and Martina Feichter, medical editor and biologistRicarda Schwarz studied medicine in Würzburg, where she also completed her doctorate. After a wide range of tasks in practical medical training (PJ) in Flensburg, Hamburg and New Zealand, she is now working in neuroradiology and radiology at the Tübingen University Hospital.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
With tonsillitis (medical tonsillitis, angina tonsillaris) the tonsils are inflamed. This usually manifests itself in a sore throat and difficulty swallowing. Often tonsillitis can be treated with medication. Only if the tonsils become infected very often are they removed. Read all about symptoms, treatment, and home remedies for tonsillitis!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. A36J35J03
Brief overview
- Common symptoms: sore throat, difficulty swallowing, reddened and coated tonsils, reddened throat wall, swollen lymph nodes, fever
- Treatment: Home remedies (neck wrap, gargling, lozenges, etc.), pain relievers, antibiotics if necessary, surgery
- Special form: Chronic tonsillitis (recurrent tonsillitis)
- Contagion: Risk of infection high in the first few days, via droplet infection
- Tonsillitis - duration: Acute tonsillitis usually heals within one to two weeks if properly treated.
- Possible complications: otitis media, sinusitis, earache, peritonsillar abscess, rheumatic fever, "blood poisoning" (sepsis)
Symptoms: This is how tonsillitis manifests itself
Symptoms such as sore throat and difficulty swallowing are typical of tonsillitis. Most often they develop within a few hours. The palatine tonsils on both sides of the uvula are clearly reddened, swollen and possibly whitish or yellowish.
The wall of the pharynx is also reddened, and the lymph nodes in the corner of the jaw are often palpably enlarged. In addition, there is an unpleasant halitosis (foetor ex ore) as another typical sign of tonsillitis. Often the sick feel weak and dull. In many cases, there is also a (high) fever. A tonsillitis without a fever is also possible.
This is how you can tell if you have tonsillitis
Differences between viral and bacterial tonsillitis
Usually it is viruses such as rhino, corona or adenoviruses that cause tonsillitis. In addition to tonsillitis, those affected often also suffer from a cold. Therefore, patients with viral tonsillitis often complain
- sniffles
- cough
- Headache and pain in the limbs
In addition to viruses, bacteria, especially streptococci, can also cause tonsillitis less often. Pus on the tonsils - recognizable by white-yellowish dots or coatings - is a typical sign of bacterial tonsillitis. The distinction between viral and bacterial tonsillitis is usually difficult. For patients who are 15 years of age or older, a special criteria system (Centor Score) helps the doctor estimate the likelihood of streptococcal tonsillitis (more precisely: an infection with group A streptococci):
- Fever over 38 degrees
- no cough
- swollen and painful cervical lymph nodes
- enlarged and coated tonsils
If all four symptoms of tonsillitis have all four symptoms, about 50 to 60 percent of the time it is a strep infection. If three of the above symptoms are present, the probability is still around 30 to 35 percent.
The Centor Score can only give a tendency, but not a diagnosis. Only the analysis of an almond swab can show with certainty whether streptococcal tonsillitis is actually present.
In order to be able to assess tonsillitis in children, there is the modified Centor Score (McIsaac Score). can be used from the age of three years. The McIsaac score contains the same criteria as the conventional Centor score. However, all children between the ages of three and 14 receive an additional point, adults aged 45 and over receive one point less. There are also other classification systems that can help distinguish between viral and bacterial tonsillitis.
Tonsillitis as a symptom and special forms
A tonsillitis is not just a clinical picture. It can also be a symptom that accompanies other diseases. There are also special special forms. Examples are:
- Glandular Pfeiffer fever
- diphtheria
- Scarlet fever
- Herpangina
- Angina Plaut-Vincent
- Syphilis and gonorrhea (gonorrhea)
- tuberculosis
- Thrush angina in fungal infection
Tonsillitis - symptoms of glandular fever from Pfeiffer's glandular fever: If tonsillitis is a symptom of this viral disease, the tonsils are dirty, white and gray. In addition, the lymph nodes in the corner of the jaw, in the neck, throat and groin area are often severely swollen.
Tonsitis - Symptoms of Diphtheria: Diphtheria is a dangerous bacterial infection, often accompanied by inflammation of the larynx or tonsillitis. The almonds are then covered with a grayish-white coating. If you try to remove the plaque, it usually bleeds. Those affected often have a putrid, sweetish halitosis, which is compared, for example, to fermenting apples.
Tonsillitis - symptoms of scarlet fever: tonsillitis from scarlet fever manifests itself in deep red tonsils, which are sometimes covered with purulent sticks. The throat wall is also mostly reddish in color. Small, whitish deposits can appear on the lining of the mouth on the inside of the cheeks. A white "raspberry or strawberry tongue" is also typical at the beginning and then red - the tongue resembles the surface of the fruits mentioned.
Tonsillitis - symptoms of herpangina: In case of tonsillitis caused by the Coxsackie A virus (herpangina), the tonsils are only slightly swollen. In addition, small vesicles (canker sores) form on the palate and cheek mucosa, which leave flat, painful defects after they burst. Fever, difficulty swallowing and a clear feeling of illness are further symptoms.
Tonsillitis - symptoms of angina Plaut-Vincent: Angina Plaut-Vincent is a rare form of bacterial tonsillitis that occurs mainly in younger men. Usually only the almond is infected on one side. It has ulcers and a green-gray coating of mucus. There is also a bad breath. Patients with this clinical picture usually do not have a fever and usually feel relatively healthy.
Tonsillitis - symptoms of syphilis and gonorrhea: Syphilis (syphilis) is a sexually transmitted disease that has several stages. In the second stage, tonsillitis sometimes develops. Symptoms of this so-called angina specifica are swollen, reddened tonsils with a veil-like, gray-white coating (plaques opalines). A large, dark red rash is often visible on the oral mucosa (plaques muqueuses). Fever does not occur.
Tripper (gonorrhea) - another sexually transmitted disease - can lead to tonsillitis, among other things.
Tonsillitis - symptoms of fungal infection
A typical pathogen is the yeast Candida albicans. Those affected usually have whitish coatings on their oral mucosa (thrush stomatitis) as well as on the tonsils. This disease, also known as thrush angina, usually occurs in patients with weakened immune systems. Fungal tonsillitis can also be the result of cortisone sprays.
Tonsillitis - symptoms of tuberculosis
Tonsillitis associated with tuberculosis is very rare. In this case, flat defects of the mucous membrane on the tonsils appear.
Tonsillitis: treatment
Treatment of tonsillitis depends on its cause, severity and whether it has occurred more often. Home remedies often help against a slight sore throat caused by tonsillitis. In conventional medicine, doctors usually prescribe painkillers. As a rule, they also work against any fever that may occur. Antibiotics are also used for bacterial tonsillitis. If the tonsillitis is chronic or recurrent, surgery may be necessary.
If complications such as a peritonsillar abscess (encapsulated pus focus) occur, inpatient treatment in a hospital may be necessary. Doctors usually operate here too.
Self-help with tonsillitis: what to do at home?
Often, mild tonsillitis develop as part of a cold. With the help of physical restraint and home remedies, you can also support the healing of your tonsillitis yourself. The symptoms can often be successfully alleviated, for example, with the following tips:
- Neck wrap
- Gargle (with solutions and tea)
- Medicinal herbal teas (for example, sage)
- Inhale
- bed rest
- moist room air
- drink enough (no acidic drinks, e.g. juice)
- prefer to eat soft, spicy foods
What else you can do at home and where the limits of home remedies are for tonsillitis, read in the article tonsillitis: home remedies.
Tonsillitis: when to see a doctor?
Pain is the most annoying symptom of tonsillitis, especially in the first few days. First of all, you can try to deal with the pain with measures such as neck wraps or lozenges, special lozenges as well as sprays and antiseptic and locally anesthetic gargle solutions from the pharmacy.
If these measures aren't enough, you can try over-the-counter pain relievers - such as acetaminophen or ibuprofen. The drugs have a pain-relieving (analgesic) and fever-lowering (antipyretic) effect, and some also have anti-inflammatory (anti-inflammatory) effects. However, you may only use these substances if you are not allergic to the active ingredients.
If you are pregnant or chronically ill, for example with your kidneys, heart or liver, or if you have known stomach problems, allergies or blood clotting disorders, you should only take the medication after consulting a doctor! Paracetamol is also not advisable in the case of glandular fever (EBV infection), as it puts additional strain on the liver.
Painkillers only alleviate the symptoms, they do not fight the pathogens.
If the immune system does not succeed in eliminating the virus or bacteria that cause the disease, despite rest and "gentle support", or if the tonsillitis is very severe, you should consult a doctor.
You should also seek medical help for tonsillitis in the following situations:
- abnormal breathing sounds
- difficult breathing
- severe unilateral pain, especially when chewing, swallowing, or opening the mouth
- Illness duration of more than three days without improvement
- persistent increase in complaints
- acute rheumatic fever in the family
- severe general illnesses
- high fever, especially if it cannot be brought down with medication
-
Tonsillitis: "In the past, the operation was faster"
Three questions for
Dr. med. Bernd Schuster,
Specialist in ear, nose and throat medicine -
1
How do I know if I have tonsillitis and not just a cold?
Dr. med. Bernd Schuster
You have a severe sore throat with painful swallowing difficulties. Pus sticks on the tonsils are usually only seen when bacteria cause the inflammation. In the case of a viral infection, the tonsils tend to be tense and slightly reddened, but they can also show smeary gray-white coatings, such as in Pfeiffer's glandular fever. However, laryngitis can also trigger a sore throat.
-
2
Who is prone to tonsillitis?
Dr. med. Bernd Schuster
It's kind of a vicious circle: the more often you have tonsillitis, the more susceptible you are. This is because the small tubules in the tonsils become scarred when they become infected. Viral or bacterial infections are particularly easy to develop behind this. In some patients, the quality of life suffers so much from the constant inflammation that the tonsils are removed.
-
3
There used to be more tonsil operations, why?
Dr. med. Bernd Schuster
The guideline now says that tonsils should only be operated on if you have had six or more bacterial tonsillitis a year that require antibiotic treatment. A high bar! Maybe too high. You have to weigh up each individual case carefully and, if necessary, operate if this alleviates the symptoms - even if, according to the guideline, an operation should not yet be carried out.
-
Dr. med. Bernd Schuster,
Specialist in ear, nose and throat medicineDr. Schuster runs a private practice in Munich with a focus on ENT medicine and plastic surgery.
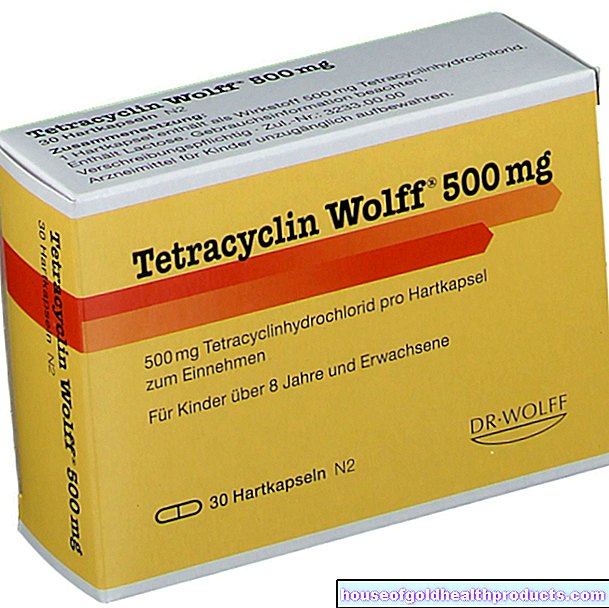
Medical treatment for bacterial tonsillitis
If the doctor can detect streptococcal tonsillitis or if it is very likely, the doctor usually prescribes antibiotics, primarily of the penicillin V type. Those who cannot tolerate this active ingredient are given other antibiotics (such as cefadroxil or erythromycin), which are also effective against streptococci .
Other antibiotics are only used when the pathogenic bacteria have become insensitive (resistant) to the standard active ingredients or the patient cannot take the latter.
It is important: the antibiotics must be taken for as long as the attending physician has prescribed them. Do not stop taking the medication prematurely - even if the symptoms improve beforehand! Some bacteria can then still romp around in the body, which can then trigger inflammation again or develop resistance to the antibiotic.
Resistant bacterial strains can develop with any antibiotic therapy. For this reason, antibiotics should not be used prophylactically in tonsillitis, but only come into consideration if a bacterial cause is proven or very likely.
Medical treatment for viral tonsillitis
Antibiotics only work against bacteria, so they are not used for viral infections. Doctors only use them for viral tonsillitis if there has been an additional bacterial infection on the diseased mucous membranes (superinfection).
Treatment for viral tonsillitis is therefore usually limited to treating symptoms such as fever and pain. In addition to pain medication, home remedies and physical restraint can accelerate the recovery process.
Physical rest is particularly important in the case of infections. Even initially harmless diseases can cause potentially life-threatening myocarditis when exposed to excessive stress.
With Pfeiffer's glandular fever, internal organs (spleen, liver) can swell and there is a risk of a ruptured spleen. This complication is life threatening and requires inpatient treatment in a hospital. Therefore, physical protection is extremely important here too.
Chronic tonsillitis: what to do?
Chronic tonsillitis occurs when the tonsil tissue becomes inflamed again and again or the inflammation never subsides completely. Either (dead) material of the germs collects in the depressions (crypts) of the tonsils, which cause persistent inflammation. Or acute infections keep coming back. The deposited cell material often also serves as an ideal breeding ground for the pathogens. Doctors refer to recurring tonsillitis as recurrent tonsillitis.
You can learn more about symptoms and treatment of chronic tonsillitis in the article Chronic tonsillitis.
Tonsillitis: when to operate
If tonsillitis occurs frequently, the tonsils are often completely removed. This so-called tonsillectomy is one of the most frequently performed medical interventions in this country. The surgeons remove the tonsils either with heat (e.g. laser treatment, radio frequency device) or with scissors or a snare.
There is also the option of partially removing the tonsils (tonsillotomy). It is a little gentler than the complete removal of tonsils. However, it is not certain how effective a tonsillotomy can prevent re-tonsillitis in the long term.
You can find out more about the procedure, benefits and risks of tonsillectomy in the article tonsillectomy.
Tonsillitis: treatment with homeopathy
Many patients also turn to naturopaths with the question “What helps with tonsillitis?”. Homeopathy is particularly popular among the alternative healing methods. However, it is not a substitute for necessary conventional medical treatment.
Depending on the symptoms, the homeopathic remedies Aconitum, Belladonna, Apis or Pyrogenium are recommended for acute tonsillitis.
The concept of homeopathy and its specific effectiveness are controversial in science and not proven beyond doubt by studies.
Tonsillitis: where it comes from
The tonsillitis (tonsillitis) is an inflammation of the tonsils, which sit on the right and left in the throat. It is one of the most common reasons people see a doctor. Children and adolescents are more likely to develop tonsillitis than adults.
Viruses are usually the cause of tonsillitis. Bacteria cause tonsillitis less often, usually of the streptococcal type. The pips or yellow-whitish deposits on the inflamed tonsils, which are typical of bacterial tonsillitis, consist of dead bacteria and dead cells of the immune system. The tonsillitis can occur unilaterally or bilaterally.
Acute inflammation of the tonsils usually starts quickly. In the majority of patients, however, the symptoms improve significantly after just three days. Tonsillitis usually heals on its own within a week or two. In the case of bacterial tonsillitis, however, the administration of antibiotics may be necessary to support and accelerate the healing process.
Doctors speak of chronic tonsillitis if the inflammation has persisted for more than three months. The course can vary. The inflammation is often smoldering in the tonsils, and patients are symptom-free or have only mild tonsillitis symptoms. Now and then an acute inflammatory process flares up on this floor.
The currently valid guidelines do not use the term "chronic tonsillitis". Instead, the experts speak of recurrent tonsillitis, a recurring tonsillitis. You can find out more about this in our article Chronic tonsillitis.
Tonsillitis: causes and risk factors
A tonsillitis can be triggered by various pathogens. These can easily become attached to the fissured surface of the tonsils. In principle, this is even good:
As part of the immune system, one of the tasks of the tonsils is to intercept pathogens that have entered the throat and thus prevent them from infecting the airways. The tonsils contain numerous immune cells that render invading pathogens harmless. Therefore, permanent natural inflammatory processes basically take place in the tonsils. If the organism is weakened, for example by a flu-like infection, this defense can be disturbed, the inflammation can spread and tonsillitis can develop.
Bacterial tonsillitis - causative agent
In fact, tonsillitis is in many cases preceded by a viral infection (e.g. a cold), which may then be followed by a bacterial attack on the tonsils - usually with ß-hemolytic streptococci of Lancefield group A (Streptococcus pyogenes). The result is bacterial (purulent) tonsillitis. Other pathogens can also cause bacterial tonsillitis:
- Various streptococcal strains
- Staphylococci
- Haemophilus influenzae type b
- Corynebacteria
- Nokardia
- Neisseria gonorrhoeae
The special form Angina Plaut-Vincenti (ulcerative tonsillitis) is usually a mixed infection: screw bacteria (especially Treponema vincentii) and fusobacteria (especially Fusobacterium nucleatum) trigger tonsillitis.
Viral tonsillitis - causative agent
In the case of a viral tonsillitis, the inflammatory processes in the tonsil tissue are caused, for example, by typical "cold viruses" from the group of rhinoviruses. Other possible triggers are
- Coronavirus
- Adenoviruses
- Influenza viruses and parainfluenza viruses
- Epstein-Barr virus (causative agent of Pfeiffer's glandular fever)
- Enteroviruses such as coxsackieviruses
- RS virus especially of tonsillitis in children
Angina agranulocytotica
For example, because of strong chemotherapy, as in the case of blood cancer, or because of other drugs such as metamizole, some people hardly have any immune cells. Doctors call this agranulocytosis. This can lead to tonsillitis with dirty ulcers, strong bad breath and fever. In addition, those affected feel seriously ill. However, lymph nodes typically do not swell because the immune cells that accumulate there are hardly present.
A tonsillectomy cannot be performed in angina agranulocytotica!
Is tonsillitis contagious?
Since the pathogens can also be found in saliva, tonsillitis is contagious - provided that the infection actually causes tonsillitis, because an infection proceeds differently depending on the pathogen and from person to person. Cold viruses are often the cause of tonsillitis. But by no means all colds are accompanied by tonsillitis.
Other people can become infected with the usual pathogens of tonsillitis through germ-containing droplets. Doctors speak of droplet infection here.
Since the risk of infection with tonsillitis is high, especially in the first few days, you should avoid contact with other people as much as possible during this time.
If tonsillitis is treated with an antibiotic, the risk of infection can be greatly reduced after just one day. If none is prescribed, for example for viral tonsillitis, the patient is contagious for one to two weeks.
Unlike chickenpox, for example, you are not immune to re-infection after tonsillitis.
Tonsillitis: examinations and diagnosis
Severe sore throats and difficulty swallowing, fatigue and fever often lead those affected to the doctor. He will first ask a few questions about the medical history (anamnesis). Possible questions are, for example:
- How long have the complaints existed?
- What are the symptoms (fever, sore throat, rash, shortness of breath, etc.)?
- Do you experience pain when chewing, swallowing, or opening your mouth?
- Has the tonsillitis developed again (acute tonsillitis) or is it a recurring problem (chronic tonsillitis)?
Physical examination
The doctor then checks whether reddening, swelling or plaque can be seen on the throat and tonsils. He also scans the lymph nodes, especially on the neck and back of the head. They can be swollen with tonsillitis.
The examination and the symptoms described are usually sufficient for the doctor to diagnose "tonsillitis".
Throat swab
If there is suspicion that the tonsillitis is caused by certain bacteria (beta-hemolytic streptococci of group A, GABHS for short), the doctor will take a throat swab. To do this, he strokes the back of the pharynx with a special cotton swab in order to take a sample of the saliva there. Any streptococci that may be present in the smear can then be detected with a rapid test or in the laboratory: The result of the rapid test is available after a few minutes, but the test does not detect every streptococcal infection. The analysis of the smear in the laboratory is more reliable - using a bacterial culture. But that takes a day or two.
Further investigations
In some cases, further tests may be necessary. For example, if an encapsulated pus focus (abscess) is suspected, the doctor will perform an ultrasound examination. In some cases, blood tests can also be useful, for example to rule out other diseases.
Tonsillitis: disease course and prognosis
The course of tonsillitis depends on many factors.These include the type of tonsillitis as well as the physical condition and immune system of the patient.
In the case of acute tonsillitis, the symptoms usually decrease significantly after a few days. Symptoms go away completely within a week or two. It may take a little longer for the swelling of the tonsils to subside.
If bacterial tonsillitis is treated with antibiotics, the duration of the illness is shortened.
Complications of tonsillitis
Sport should be avoided with (purulent) tonsillitis, as the immune system already needs a lot of energy to fight germs. Otherwise, tonsillitis can become chronic or cause complications. Because physical exertion also increases the risk that bacteria are carried to other organs via the bloodstream.
In addition, complications often arise when a bacterial, purulent tonsillitis has not been treated with antibiotics at all or has been treated too briefly. There is also an increased risk of complications during pregnancy.
Here is an overview of important complications of purulent tonsillitis:
Middle ear and sinusitis
A middle ear infection (otitis media) usually occurs when the ventilation of the so-called ear trumpet (connection from the nasopharynx to the middle ear) is prevented by the swelling of the mucous membrane. It is similar with a sinus infection. Earache or pressure pain over the maxillary and frontal sinuses are then typical symptoms. Middle ear and sinus infections are common comorbidities and / or consequences of tonsillitis, especially in childhood.
Peritonsillar abscess
In the case of tonsillitis with peritonsillar abscess, an inflammatory focus is encapsulated between the tonsil and the surrounding connective tissue (peritonsillitis). Most of the time, the pharynx wall bulges significantly inwards on the affected side. Those affected often have severe sore throats and swallowing pain and can only open their mouths minimally (jaw clamp). Other symptoms are
- lumpy language
- increased salivation
- "Wry neck" with the head tilted to one side
- Breathing sounds (stridor)
- possibly shortness of breath with increasing swelling and thus narrowing of the airway
People who smoke while having tonsillitis are more likely to develop an abscess. Another risk factor is poor oral hygiene.
Rheumatic fever
Streptococcal tonsillitis can result in a rheumatic fever. This is a kind of autoimmune reaction that is triggered by cell components of the streptococci. Most of the time, those affected get a fever again. In addition, a circular, reddish rash (erythema annulare rheumaticum) and painful joint inflammation can occur. The latter can last for many years or flare up again and again if the course is unfavorable.
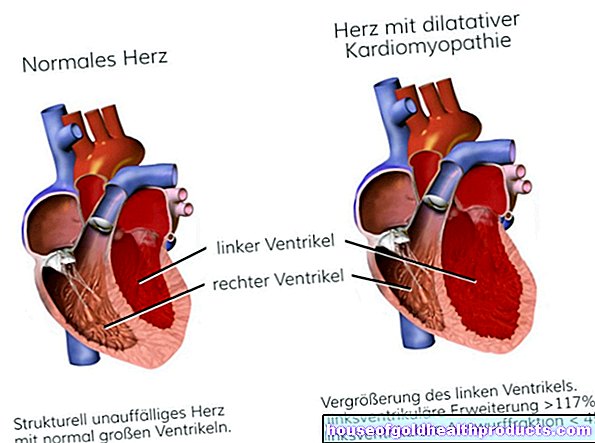
In addition, heart inflammation can develop in the course of rheumatic fever. Affected is either the inner layer of the heart (endocarditis), the heart muscle (myocarditis) or the pericardium (pericarditis) - or all structures (pancarditis). This inflammation can cause the heart to stop beating steadily. Endocarditis is decisive for the long-term prognosis because it can result in permanent heart valve defects (mostly mitral valve, also aortic valve).
The acute rheumatic fever can also affect the nervous system and manifest as so-called "chorea minor". This disease shows up a few weeks to months after the tonsillitis has subsided. Symptoms are lightning-fast shooting movements of the arms, throat and throat. These twitches come on suddenly and cannot be controlled.
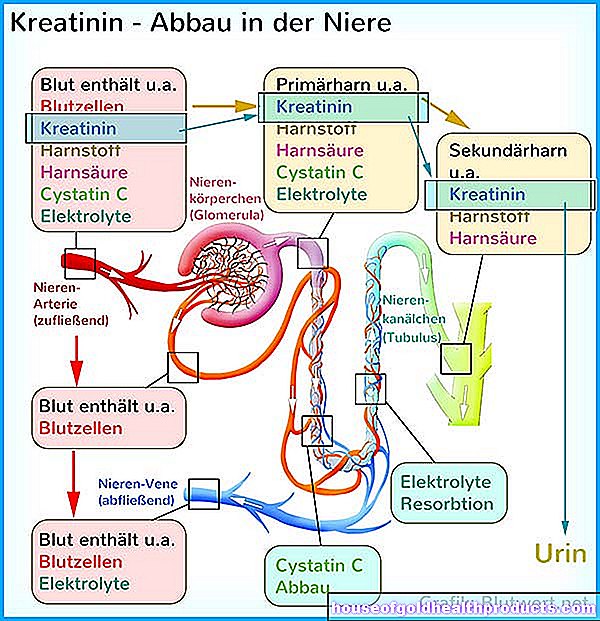
Inflammation of the kidney corpuscles (acute post-streptococcal glomerulonephritis)
In some patients, acute kidney inflammation (more precisely: inflammation of the kidney corpuscles) is the result of tonsillitis. A sign of this is, for example, blood in the urine. Sometimes, however, it is only a very small amount of blood that is barely visible to the naked eye, but can only be reliably detected in the laboratory (occult blood). Other possible symptoms are
- Flank pain
- Decreased urination due to less urine
- High blood pressure (such as with a headache)
- Edema
- Feeling sick
Around half of those affected have no symptoms, but in some cases they still develop permanent kidney damage.
Streptococcal tonsillitis can also trigger kidney inflammation in children. In severe cases, the kidney can even fail completely. Most of the time, however, the children recover within a few days.
sepsis
Sometimes bacteria that caused tonsillitis get into the bloodstream and spread around the body. One speaks here of bacterial blood poisoning (sepsis). It is a serious, life-threatening clinical picture in which many organs of the body can lose their functionality. Intensive medical care is necessary here.
Additional information:
Guideline:
- Therapy of inflammatory diseases of the tonsils - tonsillitis (status: 08/31/2015, validity extended to 08/30/2020)
Tags: desire to have children sports fitness healthy workplace