Placenta previa
Mareike Müller is a freelance writer in the medical department and assistant doctor for neurosurgery in Düsseldorf. She studied human medicine in Magdeburg and gained a lot of practical medical experience during her stays abroad on four different continents.
More about the experts All content is checked by medical journalists.Placenta previa (placenta previa) refers to the misalignment of the placenta in pregnant women. A typical symptom is vaginal bleeding late in pregnancy. Depending on its extent, the placenta previa can be life-threatening for both mother and child. Read everything you need to know about placenta previa here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. O44
Placenta previa: description
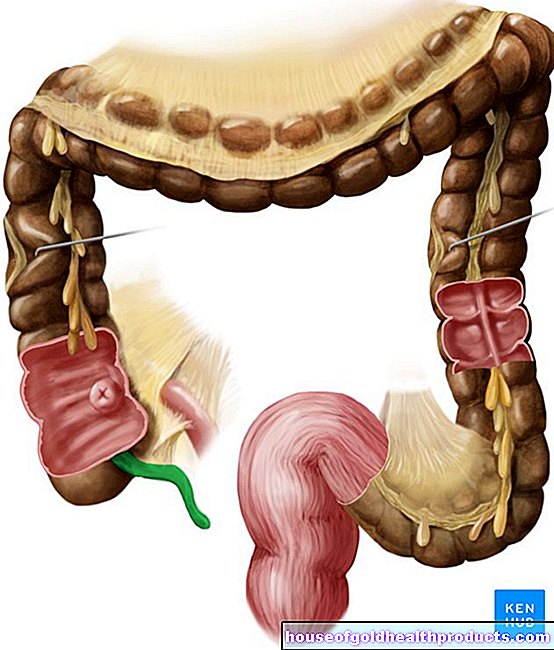
A placenta previa (placenta previa) is a not normally seated placenta in the uterus. The placenta is a disc-shaped organ about five to 20 centimeters in diameter. It is two to four centimeters thick and weighs an average of about 500 grams The placenta is used to supply the unborn child with nutrients and oxygen. It also produces important hormones such as progesterone, estrogen and hCG (human chorionic gonadotropin), which are important for maintaining pregnancy.
A placenta previa more or less completely covers the inner cervix, i.e. the exit of the uterus through which the child has to pass at birth. Usually the placenta is located well away from the exit of the uterus. Depending on the extent of the misalignment, a distinction is made:
- Deep-seated placenta: It does not reach the cervix, but sits closer to it than usual.
- Placenta previa marginalis: The placenta touches the inner cervix, but does not obstruct it. Together with the deep-seated placenta, the placenta previa marginalis accounts for about half of all placenta previa.
- Placenta previa partialis: The placenta partially obstructs the inner cervix. It accounts for about a third of the location anomalies.
- Placenta previa totalis: The placenta completely covers the inner cervix. It is present in about 20 percent of the cases.
Overall, placenta previa occurs in about one in 200 pregnancies.
Placenta previa: symptoms
The placenta previa usually manifests itself as a sudden onset of vaginal bleeding. It is most likely to occur in the second half of pregnancy, most commonly at the end of the second trimester or the beginning of the third trimester. In some cases it can be accompanied by convulsions.
The bleeding can be massive and endanger the life of both mother and child. Always consult a doctor if you have vaginal bleeding during pregnancy!
Placenta previa: causes and risk factors
Normally, the placenta moves in the course of pregnancy in the direction of the mother's head, i.e. towards the upper end of the uterus. This happens due to the growth of the uterus. This ensures that the birth canal is exposed. If the placenta does not move, a placenta previa develops. At the end of pregnancy, the uterus expands so that the placenta previa can tear and painless bleeding occurs.
There are several factors that can make you more likely to develop placenta previa. These include:
- smoking
- old age of the expectant mother
- unusual shape of the uterus (uterine abnormality)
- many pregnancies in the past
- Multiple pregnancy
- Cocaine abuse
- Scars in the uterus, for example from operations, caesarean sections or abortions (scraping)
- In vitro fertilization (artificial insemination)
Placenta previa: examinations and diagnosis
If you experience vaginal bleeding during pregnancy, see your gynecologist. He will first ask you in detail about your medical history (anamnesis). Possible questions are:
- What week of pregnancy are you in?
- Do you have pain?
- Have you been pregnant once or several times before?
- Do you smoke?
Your doctor will then examine you. He will feel your stomach to determine any hardening and the position of the child. He then examines the vagina to locate the source of the bleeding.
In addition, he performs an ultrasound examination through the abdomen (transabdominal sonography). At the end of the second trimester, it can provide information about the location of the placenta. For this, the patient's urinary bladder should be about half full so that the relationships between the individual organs can be determined. Then the patient and doctor can decide together which mode of delivery - natural or caesarean section - should be carried out.
Placenta previa: treatment
If you have a placenta previa marginalis or partialis during a preventive examination, the doctor will advise you to rest in bed. Any activity should be kept to a minimum. In addition, the small pelvis should be spared. This means that you shouldn't have sex, insert anything into your vagina, or rinse it. If there is a risk of premature birth, the doctor can prescribe medication to inhibit labor. This includes, for example, atosiban. Glucocorticoids (betamethasone) can also be given to help the unborn child develop more quickly.
If bleeding occurs due to placenta previa, the therapy must be carefully considered. The danger that exists in the event of heavy bleeding for both the mother and the unborn child must be considered.Overall, the risk of bleeding placenta previa must be weighed against the risk of premature birth. If the pregnancy has progressed beyond the 36th week, the birth is usually initiated. A caesarean section is then almost always done. In the case of heavy bleeding with a large amount of blood loss, the pregnant woman may need to be given blood products (blood transfusion).
Placenta previa: disease course and prognosis
The course of a placenta previa can vary greatly from person to person. A deep placenta and a placenta previa marginalis can go unnoticed without complications. Other forms such as the placenta previa totalis, on the other hand, can be associated with heavy bleeding and great danger to life. While some bleeding with placenta previa comes to a standstill spontaneously - i.e. without any treatment - others can be life-threatening for both the mother and the unborn child. Stopped bleeding may bleed again after a few days or weeks. With the right treatment and the conscious handling of the disease, many patients with placenta previa can give birth to healthy children.
Tags: palliative medicine Diseases Baby Child