Soft tissue rheumatism
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
The term soft tissue rheumatism or soft tissue rheumatism usually includes various painful diseases of "soft" tissue such as muscles, tendons, ligaments and connective tissue. Sometimes the diffuse pain of soft tissue rheumatism can appear all over the body. This is typically the case with fibromyalgia. In other cases, soft tissue rheumatism is limited to a specific area, such as bursitis. Read more about soft tissue rheumatism here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. You can find e.g.in doctor's letters or on certificates of incapacity for work. M70M75M71M77M79M60M65M76

Brief overview
- What is soft tissue rheumatism? On the one hand, a collective term for inflammatory and non-inflammatory painful diseases of soft tissue (muscles, tendons, ligaments, fatty tissue, etc.), on the other hand, expression for the pain of the "soft" body tissue
- Symptoms: Persistent or recurring soft tissue pain, impaired function of the affected structures, possibly other complaints (e.g. sleep problems and exhaustion in fibromyalgia)
- Diagnosis: Collection of the medical history, physical examination, possibly further examinations such as imaging procedures or blood tests (especially to rule out other causes)
- Therapy: Depending on the type of soft tissue rheumatism; if possible, elimination of the cause; In addition, depending on requirements, e.g. physiotherapy, physical measures (such as cold and heat applications), medication, surgical interventions
- Prognosis: Depending on the type and cause of the soft tissue rheumatism. Often lengthy treatment. Healing is not always possible (e.g. in fibromyalgia).
What is soft tissue rheumatism?
Soft tissue rheumatism (soft tissue rheumatism) is mostly used as a collective term for various inflammatory and non-inflammatory, painful diseases of the soft tissues of the musculoskeletal system. These soft tissues mainly include:
- Muscles
- Tendons, tendon attachments, tendon sheaths
- Tapes
- Bursa
- Fascia (connective tissue)
- Adipose tissue
Diseases of bones, joints and articular cartilage - such as rheumatoid arthritis, for example - do not belong to soft tissue rheumatism. This widespread joint disease is sometimes colloquially called "real rheumatism". Apart from the affected tissue structures, it differs from soft tissue rheumatism in another point:
In rheumatoid arthritis, without adequate treatment, the affected tissue (bones, cartilage) is destroyed over time. This is usually not the case with soft tissue rheumatism: the painful soft tissue is impaired in its function, but its structure is retained.
Soft tissue rheumatism does not describe a single disease. Rather, the term stands for the painful complaints of "soft tissue" and typical diseases.
Rheumatism of the muscles
The vague term "muscle rheumatism" is often used for rheumatic pain in the muscles. Some refer to polymyalgia rheumatica as the underlying clinical picture. But also in connection with fibromyalgia one often hears of "muscular rheumatism".
Soft tissue rheumatism or muscle rheumatism are neither official names of diseases nor medical terms!
Soft tissue rheumatism: types
Depending on the rheumatic disease, soft tissue rheumatism affects the whole body or only localized parts of the body.
Generalized soft tissue rheumatism
Soft tissue pain can be chronic and diffuse throughout the body. That is why some speak of generalized soft tissue rheumatism. Pain especially in the muscles and tendons in different parts of the body is typical for fibromyalgia syndrome (short: fibromyalgia). The term "chronic pain syndrome" is also widespread.
Caution: Although fibromyalgia is only one form of soft tissue rheumatism, it is often simply referred to as "soft tissue rheumatism".
Localized soft tissue rheumatism
In localized (or regional) soft tissue rheumatism, the symptoms are limited to certain areas of the body. Examples:
- Localized, bulging or nodular, painful muscle hardening (myogelosis)
- Tendonitis (tendinitis), tendinitis (tendovaginitis), irritation of the tendons (insertion tendinopathies such as tennis elbow, mouse arm or golfer's arm)
- Irritation of the bursa, inflammation of the bursa (bursitis)
- Inflammation of the subcutaneous tissue (panniculitis)
- Pathological changes in the soft tissue in the vicinity of the joint (periarthropathy), e.g. "frozen shoulder" or a tear in the rotator cuff
- Bottleneck syndromes with narrowing of individual vessels and nerves, such as in carpal tunnel syndrome
In view of this list it becomes clear: soft tissue rheumatic complaints are not uncommon.
Soft tissue rheumatism: symptoms
The term soft tissue rheumatism basically stands for the symptoms of the respective diseases: Chronic soft tissue pain that occurs repeatedly or continuously. In fibromyalgia syndrome, the pain can be felt practically anywhere in the body (in the soft tissues); in localized soft tissue rheumatism, it is limited to a specific area.
Often the affected structures are also impaired in their function (especially restricted movement). Anyone who suffers from knot-like hardening of the neck muscles, for example, can often only move their head to a limited extent. People with tennis elbow are usually unable to fully straighten the elbow joint.
Other symptoms are possible depending on the type of soft tissue rheumatic disease. Here are a few examples:
- Carpal tunnel syndrome: painful falling asleep of the hands, especially at night; tingling sensations in the palm of the hand, later also in the fingers
- Panniculitis (inflammation of the subcutaneous fatty tissue): especially on the thighs, buttocks and hips, painful nodules in the subcutaneous fatty tissue, often red and warm; possible accompanying symptoms include joint pain, muscle pain, malaise and fever
- Fibromyalgia Syndrome: Soft tissue pain often accompanied by various symptoms such as exhaustion, insomnia, gastrointestinal complaints
Soft tissue rheumatism: causes and risk factors
As diverse as the soft tissue rheumatic diseases are - so are the causes. Sometimes there is not just one trigger; rather, several factors are involved in the development of the pain. Here are some examples:
Incorrect loads and overload
Often, incorrect loads or excessive loads are the reason for persistent or recurring soft tissue complaints, for example in:
- Tennis elbow
- Golfer arm
- Snapfinger
- Bursitis (e.g. in floor layers in the knee)
- Nodular or bulge-shaped muscle hardening (myogelosis)
Repeated, heavy stresses on the wrist (e.g. from frequent work with the jackhammer) are also possible triggers for carpal tunnel syndrome. Many passionate athletes suffer painful damage to the Achilles tendon (achillodynia) due to prolonged incorrect loading and overloading.
Injuries
In some cases, injuries contribute to the occurrence of soft tissue rheumatism. Inflammation of the subcutaneous fatty tissue (panniculitis) can be just as traumatic as a frozen shoulder ("frozen shoulder"). The latter can occur, for example, as a result of an operation in the shoulder area, panniculitis after injections.
Autoimmune reactions
Collagenoses (rheumatic connective tissue diseases) also trigger symptoms typical of soft tissue rheumatism. However, they do not belong to soft tissue rheumatism, but due to their cause (malfunctioning defense system that attacks its own body tissue) to another group of rheumatic forms - the autoimmune-related, inflammatory rheumatic diseases, which also include rheumatoid arthritis.
In principle, other inflammatory rheumatic diseases can also cause soft tissue rheumatic symptoms. Polymyalgia patients complain of severe muscle pain. However, according to the current state of knowledge, it is based on an inflammation of the blood vessels (vasculitis) - giant cell arteritis. With some vasculitides, the subcutaneous fatty tissue can become inflamed - and thus cause "soft tissue rheumatism".
Soft tissue rheumatism also includes diseases that are typical of rheumatoid arthritis, such as:
- Tendinitis
- Bursitis
- Carpal tunnel syndrome
Anatomical peculiarities
Anatomical factors also sometimes play a role in the development of soft tissue rheumatism. For example, certain malpositions of the feet favor a heel spur and achillodynia - stress-dependent pain in the area of the Achilles tendon that troubles many athletes. Legs of different lengths can cause soft tissue problems in the area of the hip joint (periarthropathia coxae).
Other non-rheumatic diseases
In some patients, soft tissue rheumatism is the result of other diseases that usually do not belong to the large area of rheumatism. Panniculitis, for example, often turns out to be a side effect of infections (e.g. with bacteria). Panniculitis can also be associated with diseases of the pancreas and benign or malignant neoplasms of tissue (neoplasias such as lymphomas).
Diabetes mellitus makes you more susceptible to both frozen shoulder and snap fingers. The latter can also occur in connection with rheumatoid arthritis. Diabetes and other metabolic diseases (such as gout or increased blood lipid levels) can also trigger stress-dependent pain in the Achilles tendon (achillodynia).
Medication and drugs
Occasionally, drugs or addictive substances are (partly) responsible for soft tissue rheumatic complaints, for example in the area of the muscles or in the case of panniculitis. Achillodynia is sometimes caused by therapy with cortisone or fluoroquinolone antibiotics (e.g. ciprofloxacin).
Other risk factors of soft tissue rheumatism
Other factors that increase the risk of soft tissue rheumatic complaints include:
- Obesity: Being very overweight not only stresses the joints, but also tissue. Obesity, for example, is one of the risk factors for carpal tunnel syndrome.
- Genetic material: According to the current state of knowledge, DNA also plays a role in some soft tissue rheumatic diseases. In fibromyalgia and carpal tunnel syndrome, for example, doctors assume that there is a certain genetic predisposition.
- Mental stress and stress: These are also partly involved in the development of soft tissue rheumatic complaints, such as painful, nodular muscle hardening (myogelosis).
- Cold, wet and co: Even the weather can contribute to soft tissue rheumatism. If, for example, inflammation of the subcutaneous fatty tissue (panniculitis) can be traced back to a long stay in freezing temperatures, doctors speak of cold panniculitis.
Unknown cause
Despite known risk factors, the cause of some patients with soft tissue rheumatism remains unexplained. So it is not yet known exactly how fibromyalgia syndrome comes about. Neither inflammatory processes nor signs of wear and tear seem to be responsible. Instead, experts suspect that disturbed pain processing in connection with other factors such as genetic predisposition and psychological stress is involved in the development of fibromyalgia.
In other diseases with soft tissue rheumatism, the cause sometimes remains in the dark. This can be the case with frozen shoulder ("frozen shoulder") and panniculitis, in which case one speaks of "primary frozen shoulder" or "idiopathic panniculitis".
Soft tissue rheumatism: examinations and diagnosis
It is not always easy for a doctor to identify the disease behind soft tissue rheumatism - the symptoms can be very diverse.
anamnese
The beginning of the diagnosis is a detailed conversation to collect the medical history (anamnesis). The doctor has the patient describe all the complaints in detail. He also asks about:
- possible injuries
- Pre-existing and underlying diseases
- taking medication
- Occupation, activity performed
- possibly practiced sport
Physical examination
The doctor can obtain further information from a physical examination. For example, myogeloses can be felt as knot-shaped or bulge-shaped, limited indurations in the muscles. Pressing on the hardening can be very painful for the patient. Even with inflammation of the subcutaneous fatty tissue (panniculitis), the doctor can feel for lumps that are slightly sensitive to pressure. The overlying skin is often reddened and warmed.
Palpation and pressure are particularly important when fibromyalgia is suspected. With this disease, certain parts of the body react very sensitively to pressure ("tender points" or pain points).
As part of the physical examination, the doctor can also test the functionality of painful structures. For example, if there is pain in the shoulder area, he will check the mobility of the shoulder joint.
Further investigations
Depending on the type of soft tissue rheumatism symptoms and the suspected cause, further examinations are sometimes indicated - to confirm the suspected diagnosis and to rule out other possible diseases. Some examples:
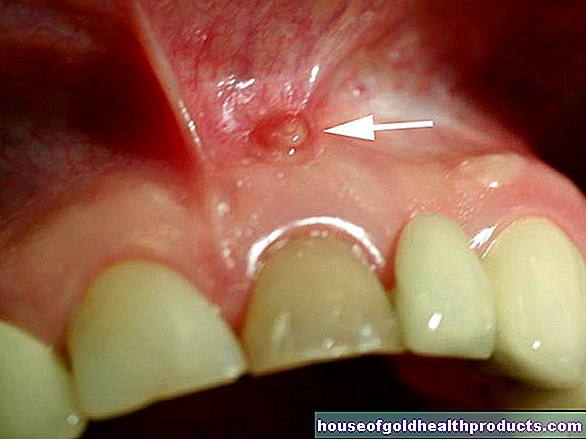
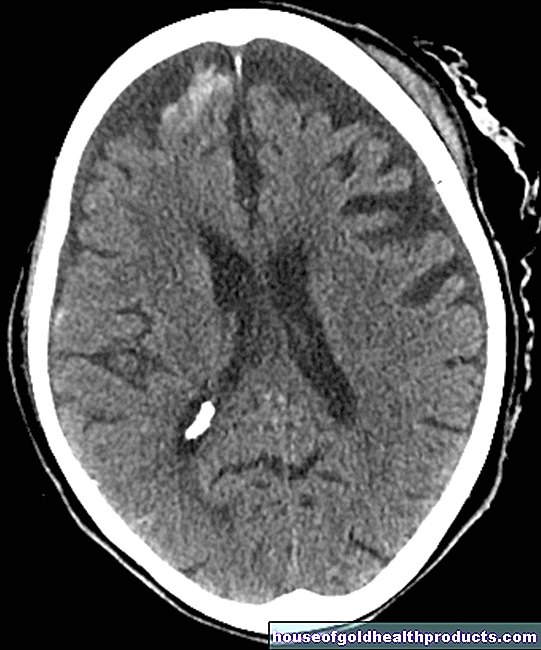
- Imaging methods such as ultrasound, X-rays, magnetic resonance imaging (magnetic resonance imaging, MRT) or computed tomography (CT) can be useful for clarifying tendon sheath or bursitis, heel spurs, achillodynia and "frozen shoulder", among other things.
- Blood tests help, for example, if fibromyalgia (generalized soft tissue rheumatism) is suspected - blood values such as blood sedimentation, leukocytes, creatine kinase and rheumatoid factor are normal in this soft tissue rheumatism, but sometimes conspicuous in other diseases with similar soft tissue rheumatoid symptoms (such as polymyalgia rheumatica, rheumatoid arthritis).
- Tissue sample (biopsy), such as a skin biopsy in the case of inflammation of the subcutaneous fat (panniculitis)
Soft tissue rheumatism: therapy
The treatment for soft tissue rheumatism is primarily determined by the type of complaints and their cause. Medicines with pain relievers and anti-inflammatory effects (especially non-steroidal anti-inflammatory drugs) are almost always prescribed to alleviate soft tissue rheumatic symptoms.
Treatment of underlying and comorbidities
Whenever possible, the cause of soft tissue rheumatic complaints should be treated or eliminated. If, for example, painful, circumscribed muscle hardening (myogelosis) has developed as a reaction to a joint disease, this must be treated. Anyone who develops a golfer's arm because he plays golf a lot, but with the wrong technique, should learn the correct stroke technique.
Various treatments for soft tissue rheumatism
Further measures can specifically help against the symptoms of soft tissue rheumatism. This is particularly important in cases in which the cause of the symptoms is poorly known or cannot be treated. Here are possible further treatment steps for soft tissue rheumatism:
Cold and heat applications
Cooling helps, for example, with soft tissue rheumatism due to inflammation of tendons, tendon sheaths, tendon attachment points and bursa. Some sufferers also find heat or cold applications beneficial in the case of stiff shoulder, heel spurs or soft tissue rheumatism near the joint (periarthropathy).
In the case of acute irritation and inflammation, cooling tends to provide relief, otherwise warmth provides relief for soft tissue rheumatic complaints.
cortisone
In some cases of soft tissue rheumatism, the doctor will prescribe anti-inflammatory cortisone either as an ointment, in tablet form, or as an injection. The doctor gives the latter, for example, in the tendons or joints in the case of tendinitis, stiff shoulder or carpal tunnel syndrome.
Physiotherapy and occupational therapy
Controlled physiotherapy, stretching exercises, special joint and muscle training can have a positive effect on soft tissue rheumatism. This is the case, for example, with complaints close to the joints, such as frozen shoulder (more under Frozen Shoulder Treatment). These measures and regular exercise are also an important part of fibromyalgia treatment.
In some cases of soft tissue rheumatism, on the other hand, it is particularly important to rest and protect the affected region! This relief helps, for example, with tennis elbow, bursitis and tendonitis or heel spurs.
massage
Sometimes a special massage (transverse friction massage, for example in the case of tendinitis) can alleviate the symptoms of soft tissue rheumatism.
OP
Surgical interventions are an option in severe cases when conservative measures are unsuccessful. For example, doctors operate on carpal tunnel syndrome when conventional measures (immobilization, cortisone) are no longer effective. Surgical intervention may also be considered in the case of persistent soft tissue rheumatism symptoms in the shoulder area.
Further treatment options for soft tissue rheumatic diseases
Soft tissue rheumatism therapy for heel spurs can also include special shoe insoles, shock wave therapy or radiation therapy (more under heel spur treatment).
In the case of panniculitis, other immunosuppressants (drugs to suppress the immune system), antimalarials or chemotherapeutic agents are used in addition to cortisone, depending on the underlying disease. The latter are agents that can damage pathogens or tumor cells.
In the case of fibromyalgia, psychological treatment and relaxation procedures can also be helpful.
In addition, many people with generalized soft tissue rheumatism consider diet to play a major role in symptom relief - so far without any scientific evidence. You can read more on the subject under Fibromyalgia Therapy and Fibromyalgia Diet.
Soft tissue rheumatism: course and prognosis
Is soft tissue rheumatism curable? Many of those affected are interested in this question, but there is no general answer. The prognosis in individual cases depends primarily on the disease of soft tissue rheumatism and whether it has a known and treatable cause.
If, for example, it is possible to permanently avoid the chronic overuse that triggered a tennis elbow, it can usually be treated successfully - especially if the therapy is started early. However, treatment can be quite lengthy. The same often applies to other forms of soft tissue rheumatism such as other tendon disorders or soft tissue complaints near the joints (periarthropathies).
The treatment of fibromyalgia, where soft tissue rheumatism basically affects the whole body (generalized soft tissue rheumatism), also requires a lot of patience: the disease is usually not curable. However, the right long-term treatment can significantly reduce the symptoms of most sufferers.
Soft tissue rheumatism: prevention
The variety of forms and causes of soft tissue rheumatism complaints make prevention difficult. However, you can try to avoid known triggers if possible, for example incorrect loading and overloading of muscles, tendons, etc. in sport and at work.
To prevent soft tissue rheumatism, it is advisable to follow occupational health recommendations!
In addition, preventive measures against some basic and concomitant diseases of types of soft tissue rheumatism are fundamentally useful. For example, a healthy diet, a healthy body weight and regular exercise can reduce the risk of type 2 diabetes - a metabolic disease that can promote stiff shoulder, snap fingers and soft tissue rheumatism complaints of the Achilles tendon (achillodynia), among other things.
In some cases of soft tissue rheumatism, however, prevention is not possible, for example in the case of fibromyalgia, the cause of which is not yet known precisely.
Tags: stress menopause elderly care





















.jpg)