Tame compulsion with a brain pacemaker
Christiane Fux studied journalism and psychology in Hamburg. The experienced medical editor has been writing magazine articles, news and factual texts on all conceivable health topics since 2001. In addition to her work for, Christiane Fux is also active in prose. Her first crime novel was published in 2012, and she also writes, designs and publishes her own crime plays.
More posts by Christiane Fux All content is checked by medical journalists.They wash their hands or scrub the floors excessively over and over again. Others have to check that the stove is off and that the doors and windows are closed - not just once, but several times. Still others compulsively count objects: red cars they encounter, buttons on the shirt of the person opposite, the glasses in the closet. Such obsessive-compulsive disorder, which makes life difficult for around two percent of the population, is difficult for outsiders to understand.
Interfering signal in the brain
In fact, it is also clear to those affected that what they are doing lacks a rational basis. They still feel the almost irresistible urge to perform “their” compulsive act. If they do not, restlessness builds up in them, which can increase to unbearable tension and irrational fears. "The cause of this phenomenon could be a kind of interference signal in the brain," explains Dr. Andreas Horn from the Clinic for Neurology with Experimental Neurology at the Charité in conversation with
Information flow in loops
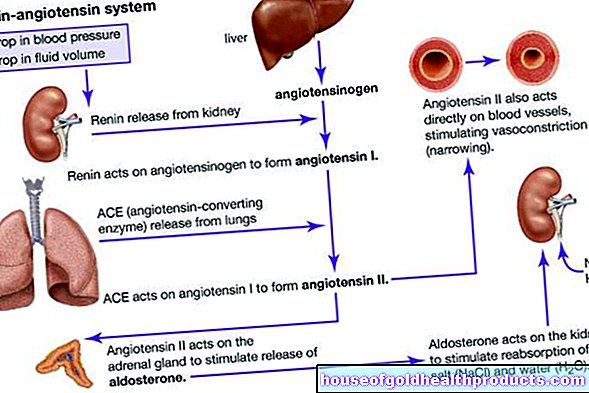
The decision as to whether or not to perform an action is made in the interplay between the outer cerebral cortex, which houses higher brain functions, and the basal ganglia deep in the brain stem. They are among the oldest brain structures and are connected to the cerebral cortex via loops through which information flows. So far, the function of the basal ganglia has only rudimentarily been clarified. However, this function seems to include initiating meaningful actions on the one hand and suppressing undesired reactions on the other.
"Feedback like at a concert"
It is precisely this corrective function of the basal ganglia that seems to be disturbed in people with obsessive-compulsive disorder. "You can imagine it to be similar to feedback when the microphone is too close to the loudspeaker at a concert and produces a high-pitched sound that overlays actual death," says Horn.
If such an interfering signal occurs in the brain, the actual information can no longer flow properly. This also applies to the feedback from the cortex to the basal ganglia, which includes that we have already checked the focus. Usually, after completing such a task, our brains tick the box, which creates a sense of satisfaction in the reward center.
"The drive remains"
However, if the process of ticking is blocked by the interfering signal, the unsettling feeling remains that the task has not been completed. “The drive remains. The patients know very well that they have already checked the stove - but the urge to go there again remains, ”explains Horn. "It's like a vicious circle that becomes independent."
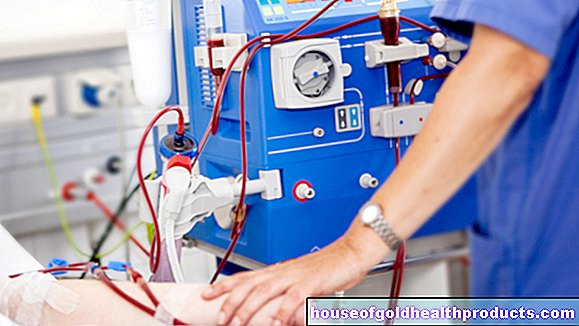
Electrodes planted deep in the brain
This is exactly where the deep brain stimulation comes in, which works in a similar way to a pacemaker. Instead of being placed on the heart, fine electrodes are placed at certain points deep in the brain. There they send out very weak electrical signals to bring the disturbed brain activity into balance so that the information between the cortex and basal ganglia can flow better again, according to the hypothesis. A cable connects the electrodes to a small device that is implanted in a skin pocket, usually in the chest area.
Effect in Parkinson's disease well documented
The occurrence of such interference signals has already been well documented in people with severe Parkinson's disease. They are already using deep brain stimulation more often. It can significantly alleviate typical Parkinson's symptoms: the uncontrolled shaking (tremor), the insecure, tripping steps as well as the "freezing", the sudden freezing of movement. If medication is no longer sufficient for such symptoms as the disease progresses, placing electrodes in the brain is another treatment option.
Parallels between Parkinson's and Obsessive-Compulsive Disorder
It has now been confirmed that the method can also help people with severe obsessive-compulsive disorder, for whom the usual therapies do not work. "The interconnection of the loop between the basal ganglia and the cerebral cortex is relatively similar for motor functions and the associative system that is responsible for making decisions," explains Horn. So what works for Parkinson's patients could probably work for people with obsessive-compulsive disorder as well.
This is indicated by a recent study: "In the four centers that were involved in our study, the obsessive-compulsive symptoms of the 50 patients in total have improved by 30 to 50 percent," reports Horn, whose institute at the Charité evaluates the results itself but no patients treated.
Up to 90 percent improvement in symptoms
In order to understand the effect, the study participants answered a questionnaire before and after inserting the electrodes for deep brain stimulation, which recorded obsessive-compulsive symptoms and their severity. But the range of success is wide: While the procedure hardly improved some patients, the symptoms were reduced by 90 percent in others.
"We assume that some patients were not stimulated at the optimal target point," says Horn. So a comparison was made between where the electrodes were placed in patients in whom the procedure had a very good effect and where in those who had benefited little or no benefit at all.
Promising bundle of fibers
In fact, the researchers have now identified a promising bundle of fibers in the brain. It connects the frontal cortex and the so-called subthalamic nucleus - a basal ganglion that is responsible for impulse control. "We hope that if we stimulate more specifically here, all patients benefit - or at least most of them," says Horn. This now needs to be checked in further studies.
Better navigating through the fog
Basically, the findings have confirmed the target area for placing the electrodes, but refined them in the process. “You can think of it like this: Up until now, during operations we always used our boat to navigate towards an island that was covered in fog. Now we can see the island and perhaps even the jetty and steer closer to it, ”says the first author of the study, Ningfei Li, describing the usefulness of the study.
Exposure therapy remains the first treatment option
The main treatment strategy for obsessive-compulsive disorder will continue to be what is known as exposure therapy. In doing so, the patient - accompanied by his therapist - exposes himself to the situation, which he finds difficult to bear, of not being allowed to perform his compulsive act. This resistance to compulsion increases restlessness and discomfort in him, possibly to an extent that is difficult to bear.
Override obsessive-compulsive disorder
The human psyche is programmed in such a way that if the feared catastrophe does not occur, tension and stress will subside by itself. Each time the patient experiences this "all clear", brain structures and interconnections solidify and strengthen, which confirm that it is okay not to check the stove again. "Everything we do affects our brain," says Horn.
Thanks to its plasticity, the organ is constantly changing and is constantly being reconfigured. For example, compulsive actions can be overwritten by alternative action - or by an electrical impulse from outside.