Chloramphenicol
Benjamin Clanner-Engelshofen is a freelance writer in the medical department. He studied biochemistry and pharmacy in Munich and Cambridge / Boston (USA) and noticed early on that he particularly enjoyed the interface between medicine and science. That is why he went on to study human medicine.
More about the experts All content is checked by medical journalists.The active ingredient chloramphenicol is an antibiotic. It is used against bacterial infections caused by pathogens that are sensitive to the antibiotic. Although chloramphenicol acts as a broad-spectrum antibiotic against many germs, it is only used as a reserve antibiotic because of possible serious side effects, i.e. when an antibiotic of the first choice does not work. Here you can read everything you need to know about chloramphenicol: effect, use and side effects.
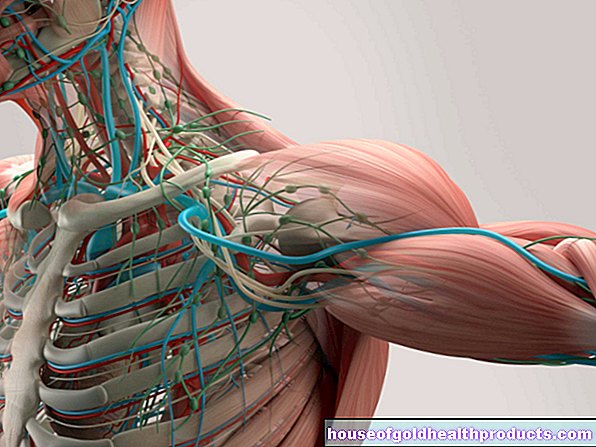
This is how chloramphenicol works
The antibiotic chloramphenicol has a specific effect on bacterial cells and hardly affects human or animal cells. At the site of the bacterial infection, it penetrates the bacteria and prevents the production of bacterial proteins there, which are essential for the metabolism, division and thus reproduction of the pathogens. Chloramphenicol thus has a bacteriostatic effect, i.e. it inhibits growth. But it has no bactericidal, i.e. bacteria-killing effect. But just because the bacteria can no longer multiply rapidly (usually exponentially) due to the antibiotic, the human immune system has a good chance of successfully fighting the infection.
In Germany, chloramphenicol is usually only applied topically, i.e. directly at the place where it is supposed to work, for example as a cream, solution, eye ointment or in the form of eye drops. Since the antibiotic is easily accessible to the tissues, part of the active ingredient is absorbed into the blood through the skin. It is quickly metabolized by the liver and excreted in the urine.
When is chloramphenicol used?
Originally, chloramphenicol was used to treat typhoid fever (caused by the bacterium Salmonella enterica) brought on the market. However, it is now used against many other bacterial infections as well. In developing countries, the antibiotic is used far more frequently than in Germany because of its low cost, where it is often only used as a reserve antibiotic for serious infectious diseases such as plague, diphtheria, dysentery, typhus and malaria. It is also occasionally used for bacterial skin, eye and ear infections.
Due to the possible formation of resistance and the associated loss of effectiveness against bacteria, the active ingredient chloramphenicol may only be used for a short time for a maximum of 14 days.
This is how chloramphenicol is used
The antibiotic chloramphenicol is mostly used locally. In acute cases, it is used every one to two hours for eye infections (e.g. in the form of eye drops); for skin infections, it is usually used one to three times a day (for example as a cream). The duration of treatment depends on the severity of the infection. After the infection has subsided, the therapy should be continued with a lower dose of chloramphenicol for about two to three days in order to prevent the development of resistance.
Especially abroad, chloramphenicol is also administered as an injection by doctors, especially in the case of very serious infections.
What are the side effects of chloramphenicol?
When chloramphenicol is used locally, there are generally hardly any side effects, as only a small amount of the active substance enters the blood. On the other hand, especially when taken orally or injected, side effects in the gastrointestinal tract such as belching and diarrhea often occur (i.e. in one in ten to one hundred people treated). The treatment triggers allergic reactions, hypersensitivity reactions, increases in liver enzyme levels, and liver damage in one in 1,000 to 1 in 10,000 patients.
The most severe and potentially life-threatening chloramphenicol side effect occurs in one of more than ten thousand people treated, so-called “aplastic anemia” - regardless of the dose and sometimes only weeks or months after treatment. This damages the bone marrow, which means that hardly any blood cells are produced there. This leads to extreme tiredness, bleeding and possibly other serious infections.
What should be considered when using chloramphenicol?
As soon as the active substance chloramphenicol enters the blood, it is metabolized in the liver, which involves enzymes that also break down many other active substances. When used at the same time, their degradation can be inhibited, which means that they can then be present in the body in excessively high and sometimes toxic concentrations. Some antidepressants, antiepileptics, anticoagulants, agents to inhibit gastric acid production, calcium channel blockers (for high blood pressure and angina pectoris), sedatives, antifungal agents, other antibiotics, cholesterol-lowering agents and agents for irregular heart rhythms are affected by this possible interaction. Before starting treatment with chloramphenicol, patients should tell their doctor that they are taking other medications.
Chloramphenicol should not be used together with active substances that also have a negative effect on the bone marrow and blood formation. Examples of this would be sulfonamides (antibiotics), phenylbutazone (anti-rheumatism agent, pain reliever) and phenytoin (anti-seizure agent, anti-epileptic agent).
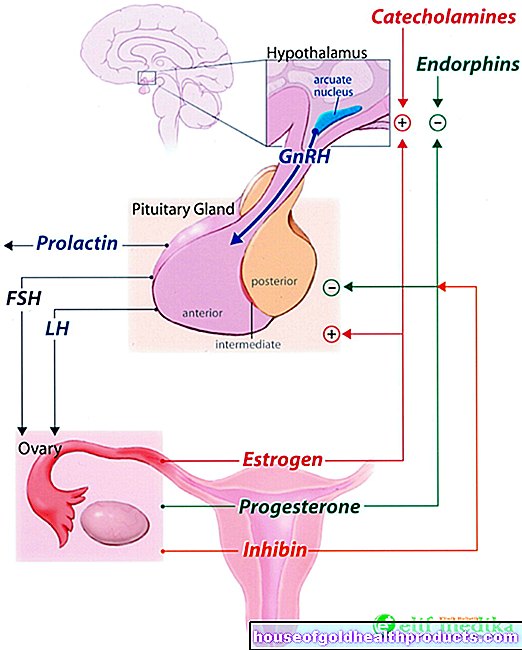
Chloramphenicol is good tissue and placental barrier and passes into breast milk, which is why pregnant and breastfeeding women should not be treated with the antibiotic. The same applies to infants under three months of age, as they cannot yet metabolize chloramphenicol via the liver. It accumulates in the children, giving them a characteristic gray skin color ("gray-baby-syndrome"). Without prompt treatment, this can be fatal.
Chloramphenicol should also not be used in severe liver and kidney problems.
How to get medicines with chloramphenicol
Preparations with chloramphenicol, which are often made directly in pharmacies as a prescription in Germany, require a prescription and are therefore only available according to a doctor's prescription.
How long has chloramphenicol been known?
The antibiotic chloramphenicol was discovered in 1947 by the professor of plant pathology David Gottlieb and from the bacterium Streptomyces venezuelae won. It was introduced into everyday clinical practice in the USA as early as 1949. Because of its comparatively simple chemical structure, the antibiotic was produced completely chemically at an early stage. Chloramphenicol has also been included in the list of essential drugs by the World Health Organization (WHO), which are intended to meet the basic medical needs of a society.
Tags: sleep diet palliative medicine











.jpg)