Erythromycin
Updated onBenjamin Clanner-Engelshofen is a freelance writer in the medical department. He studied biochemistry and pharmacy in Munich and Cambridge / Boston (USA) and noticed early on that he particularly enjoyed the interface between medicine and science. That is why he went on to study human medicine.
More about the experts All content is checked by medical journalists.Erythromycin belongs to the class of macrolide antibiotics and is used against bacterial infections. Since the active ingredient covers a similar spectrum of activity as penicillin, it is often used as a substitute for a penicillin allergy. Erythromycin is generally considered to be well tolerated, but it can lead to undesirable interactions with some other active ingredients. Here you can read everything you need to know about the effects and use of erythromycin, dosage and side effects.
This is how erythromycin works
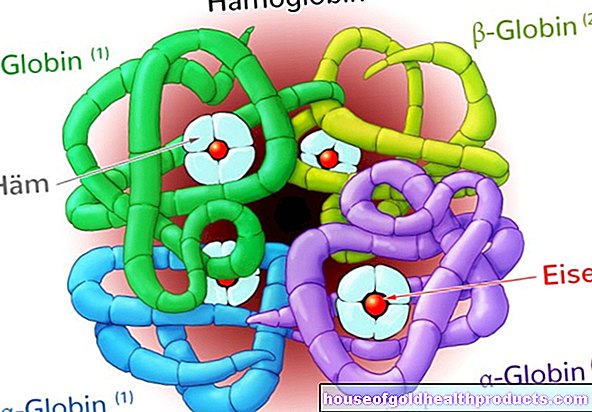
Macrolide antibiotics such as erythromycin have a growth-inhibiting effect on bacteria, i.e. they have a bacteriostatic effect:
In order to be able to grow, bacteria (like other organisms) have to produce a wide variety of proteins. The blueprints for these proteins are stored in the genome. Erythromycin prevents the bacteria from reading the information from their genetic make-up, so that protein synthesis is not possible - the bacteria cannot grow.
They do not die as a result, but the patient's immune system can bring them under control better and faster. This can usually prevent the infection from spreading and worsening.
The erythromycin contained in tablets or capsules is usually chemically modified in such a way that it is not immediately destroyed by the stomach acid and is also better absorbed in the intestine. Examples of such variants are erythromycin ethyl succinate or erythromycin lactobionate.
Uptake, breakdown and excretion
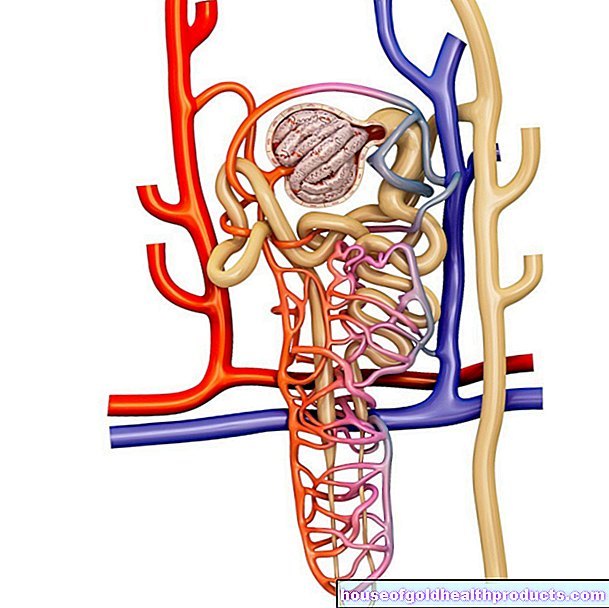
Only about 40 percent of the orally administered amount of active ingredient passes from the intestine into the blood, where the highest active ingredient concentrations are measured after one to five hours. The antibiotic is very tissue-permeable and thus reaches all areas of the body very well - except for the central nervous system (brain and spinal cord).
It is partially metabolized by the liver and excreted in the stool mainly in the bile.
When used on the skin as an erythromycin cream or erythromycin ointment, the active ingredient is hardly absorbed into the organism.
When is erythromycin used?
The areas of application of erythromycin include bacterial infections with pathogens that are sensitive to the active ingredient. These include, for example:
- Lung infections
- whooping cough
- Ear, nose and throat infections
- Skin conditions such as acne
- Internal organ infections
- Sexually transmitted diseases such as gonorrhea (gonorrhea) and syphilis (syphilis)
This is how erythromycin is used
The antibiotic can be applied externally as an erythromycin cream, gel or ointment or used as a solution for skin diseases such as acne. It is usually used twice a day.
The antibiotic is taken in the form of tablets, capsules or drinking solutions or suspensions, as a rule, three to four times a day for a limited period of time. The erythromycin dosage is up to four grams per day, correspondingly less in children and adolescents.
Erythromycin infusion solutions are also available for the inpatient treatment of severe infections. You will be fed directly into a vein via a "drip".
So that antibiotic therapy using creams, ointments, tablets, etc., can work optimally, patients should strictly adhere to the doctor's instructions for use - also with regard to the duration of therapy, which is generally seven to eight days (in the case of severe infections, up to ten days). If the symptoms improve before the end of the recommended period of use, you should still not stop taking the antibiotic on your own - stopping therapy prematurely can cause the infection to flare up again.
What are the side effects of erythromycin?
The active ingredient erythromycin is generally considered to have very few side effects. The most common side effects are gastrointestinal disorders such as abdominal pain, nausea, vomiting and diarrhea in one in ten to one hundred patients.
Occasionally (i.e. in around one in a hundred to a thousand people treated), increased liver enzyme values, skin reactions and - especially with long-term and repeated administration - infections of the gastrointestinal tract with resistant pathogens develop.
What should be considered when using erythromycin?
Contraindications
Erythromycin must not be used in:
- severe liver dysfunction
- simultaneous use of ergotamine or dihydroergotamine
- congenital QT interval prolongation (the QT interval is a specific section in the ECG)
- simultaneous use of terfenadine, pimozide, astemizole, cisapride or domperidone
- simultaneous use of certain drugs for arrhythmias (antiarrhythmics), psychoses (antipsychotics) or depression (tricyclic antidepressants)
- simultaneous use of methadone or budipine
- concomitant use of statins (drugs against high blood lipid levels) that are metabolized by the CYP3A4 enzyme system (lovastatin, simvastatin, atorvastatin)
Interactions
Interactions can occur in particular when erythromycin is used together with active substances that are broken down in the same way (via the CYP450 3A4 enzyme system) in the liver. This can lead to increased or even toxic drug concentrations in the body.
Particular caution is therefore required when combining erythromycin with:
- certain anti-epileptic drugs (phenytoin, valproic acid, carbamazepine)
- Sleeping pills and sedatives (benzodiazepines) such as diazepam, midazolam and alprazolam
- Colchicine (gout drug)
- Immunosuppressants such as ciclosporin, tacrolimus, and sirolimus
- Digoxin (for heart failure)
- Potency drugs (PDE-5 inhibitors) such as Sildenafil and Vardenafil
- Vitamin K antagonists (anticoagulants) such as phenprocoumon
- Calcium channel blockers (for high blood pressure) such as felodipine and nifedipine
- Theophylline (for asthma and COPD)
Age restriction
Erythromycin can be used from infancy. The individual dosage is basically based on body weight.
A dose reduction may be necessary in patients with liver disease or symptoms.
pregnancy and breast feeding period
Erythromycin can be used during pregnancy if the doctor deems it necessary.
The antibiotic is also suitable for use during breastfeeding. In individual cases, however, the infant may have thinner stools. Then breastfeeding should be interrupted for the duration of the antibiotic therapy.
This is how you get drugs with the active ingredient erythromycin
Because erythromycin can interact with many other active ingredients and its use should be carefully considered in many cases, the antibiotic is only available with a prescription in pharmacies in Germany, Austria and Switzerland.
The ointments, solutions and gels available in Germany and Switzerland are not commercially available as finished preparations in Austria. However, they can be prepared directly in the pharmacy as prescribed by a doctor.
Since when is erythromycin known?
The active ingredient erythromycin was discovered in 1949 in soil samples from the Philippine province of Iloilo. First it was named "Ilotycin", later it was renamed "Erythromycin" because it was obtained from the soil bacterium "Streptomyces erythreus".
From 1952 erythromycin was marketed commercially. It served as a precursor to many newer antibiotics such as clarithromycin and azithromycin.
Tags: laboratory values alcohol drugs tcm