Taming Diabetes
Luise Heine has been an editor at since 2012. The qualified biologist studied in Regensburg and Brisbane (Australia) and gained experience as a journalist in television, in the Ratgeber-Verlag and in a print magazine. In addition to her work at , she also writes for children, for example for the Stuttgarter Kinderzeitung, and has her own breakfast blog, “Kuchen zum Frühstück”.
More posts by Luise Heine All content is checked by medical journalists.So far, diabetics do not have many options when it comes to treatment: Type 1 diabetics can only balance the consequences of their illness with medication, type 2 diabetics also try to tweak their lifestyle.
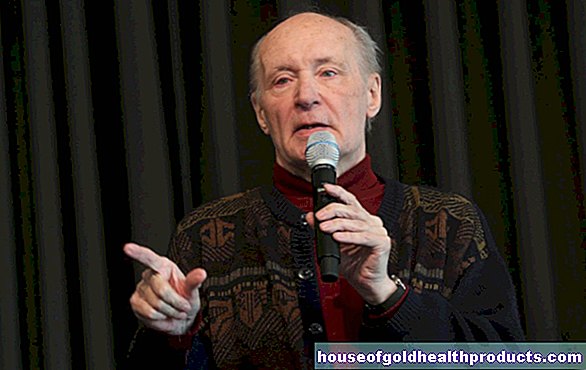
Munich scientists led by Prof. Heiko Lickert have now embarked on a completely new therapeutic path: They want to send diabetes into remission - in other words, at least temporarily weaken or even reverse the symptoms of the disease. The researchers have already tested this in the animal model.
Beta cells are at the center of the diseases
To understand the new thrust, one has to look at how diabetes develops. The focus is on the so-called Langerhans island cells. These accumulations of cells in the pancreas form the control center for regulating blood sugar. The beta cells are a particularly important part of the islet cells. They produce the body's own insulin. Normally. Because for this they have to be programmed correctly.
When cell identity is lost
In the course of the development of diabetes, however, many of them lose their cell identity, they “dedifferentiate”. "In type 2 diabetes, this is triggered, for example, by stress, such as too much glucose or too many lipids," explains Lickert. What is exciting is that the cells do not die in the process; they are still there, but not active. This is how you protect yourself from prolonged work stress.
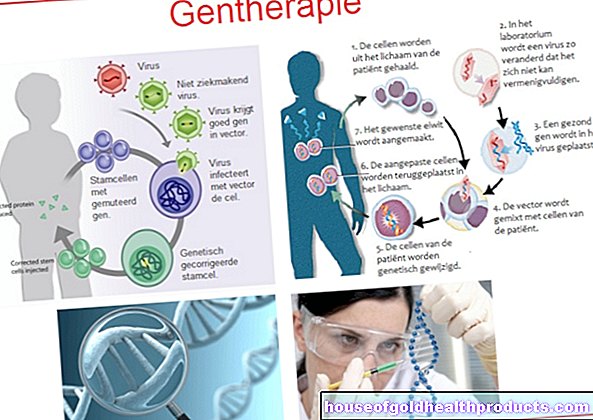
The scientists' idea was to remind these limping cells of their task again so that the regulation of blood sugar works again. The diabetes could be sent into remission in this way. To investigate this, they treated mice in which the beta cells had previously been artificially dedifferentiated with various drugs.
Efficient combination of active ingredients
The most successful was the combination of the glucagon-like peptide-1 (GLP-1), estrogen and a long-acting insulin. GLP-1 acts as a smuggler, which specifically smuggles the active ingredients estrogen and insulin into the beta cells.
This trio had the greatest positive effect on the normalization of blood sugar levels and on the glucose tolerance of the cells. But the insulin production of the beta cells and their number also increased. "We were surprised ourselves how well the regeneration works with it," says Lickert.
Slicer molecule for active ingredients
A special highlight for him was that with the GLP-1 as a key, the beta cells can be specifically addressed and activated. In this way, active ingredients can be channeled into the cells and possible side effects can be reduced.This is important in the case of estrogen, as the hormone can also have an effect on other parts of the body - and not just positively. Because it stimulates cell reproduction, estrogen is suspected to increase the risk of cancer.
Combat the symptoms, not the cause
“At the moment, nothing on the market is stopping the disease,” explains Lickert. Even the new approach would not change that. For this reason, a lifestyle change in type 2 diabetes is always part of the therapy so as not to stress the cells again. One advantage of the new combination, however, would be that it does not contribute to weight gain like insulin does.
Special case of type 1 diabetes
Although type 1 diabetes is basically a completely different disease than the much more common type 2 diabetes, the new therapeutic approach could also help here. Type 1 diabetes is caused by the immune system attacking the isulin-producing beta cells. So it is an autoimmune disease.
"With type 1 diabetics, you first have to get a grip on the immune system," says Lickert. At the moment, for example, there is the approach of blocking the helper cells that attack the beta cells. Tinkering with the immune system, however, harbors some dangers. That is why the therapy is only carried out for two weeks in children in the early stages of the disease. After all, the outbreak of the disease can be postponed for up to two years.
“Our long-term idea is not only to suppress the immune response, but also to regenerate the beta cells.” This is where the new active ingredient combinations come into play. It could reactivate the remaining beta cells just as it does in type 2 diabetics. That way, the disease could possibly be delayed even longer.
Research takes patience
A key point here is balancing the risks and benefits of a new drug. Estrogen is just not completely safe. Therefore: "Next we want to try to attach other substances to GLP-1 to see what else has a good protective effect for the beta cells," says Lickert.
However, there is still a long way to go before the method can actually be used in therapy. The researchers next want to test whether the targeted transport system also works in human cell cultures. “That means at least another three years of research,” says the scientist. Only then did the various clinical studies start. Only when these are successful would a corresponding drug come onto the market. Ten years can easily go by.
New notch
Now that he and his colleagues know exactly how they can specifically transport substances that can protect beta cells into them, they can systematically search for them. "It is a new notch that we can strike in order to counter the diseases - one in which we can prevent some of the side effects of other drugs."
Tags: diet sports fitness womenshealth