Blood in the stool
and Sabine Schrör, medical journalistMarian Grosser studied human medicine in Munich. In addition, the doctor, who was interested in many things, dared to make some exciting detours: studying philosophy and art history, working on the radio and, finally, also for a Netdoctor.
More about the expertsSabine Schrör is a freelance writer for the medical team. She studied business administration and public relations in Cologne. As a freelance editor, she has been at home in a wide variety of industries for more than 15 years. Health is one of her favorite subjects.
More about the experts All content is checked by medical journalists.Blood in the stool is easy to fear. But colon cancer is not always behind it. Usually, comparatively harmless diseases such as gastrointestinal infections, intestinal polyps or hemorrhoids are the cause. Stomach ulcers and inflammatory bowel disease also often cause bloody stools. In any case, blood in the stool should always be checked by a doctor. In the following you will find everything you need to know about the symptom "blood in the stool".

Brief overview
- Description: Red blood in the stool (hematochezia) usually indicates a source of bleeding in the middle or lower gastrointestinal tract. Black blood in the stool (tarry stool, melena) usually signals bleeding in the upper gastrointestinal tract (between the esophagus and the duodenum).
- Causes: Bleeding in the digestive tract of various causes, e.g. gastrointestinal ulcer, chronic heartburn, varicose veins in the esophagus (esophageal varices), mucosal damage from drugs (such as ASA) or violent vomiting, Crohn's disease, ulcerative colitis, intestinal polyps, protrusions of the intestinal wall (diverticulosis ) that can become inflamed (diverticulitis), infections, vascular obstruction in the intestine (mesenteric infarction), hemorrhoids, tumors (such as stomach cancer, colon cancer).
- When to the doctor Always to rule out serious illnesses as the cause. This is especially true if there are additional symptoms such as stomach or abdominal pain, pain during bowel movements, nausea and vomiting, persistent exhaustion or fatigue, significant weight loss in a short time and / or night sweats.
- Diagnostics: taking the medical history (anamnesis), physical examination, gastroscopy, colonoscopy (possibly only rectoscopy), double balloon enteroscopy, video capsule endoscopy, ultrasound, nuclear medicine procedures, selective arteriography, blood and stool examination
- Treatment: Acute bleeding is stopped (for example by means of sclerosing, rubber band ligation or adrenaline injection). Blood substitutes are necessary for high blood loss and blood transfusions in severe cases. In addition, if possible, the cause (gastric ulcer, Crohn's disease, hemorrhoids, etc.) is treated accordingly in order to prevent renewed bleeding.
Blood in the stool: causes and possible diseases
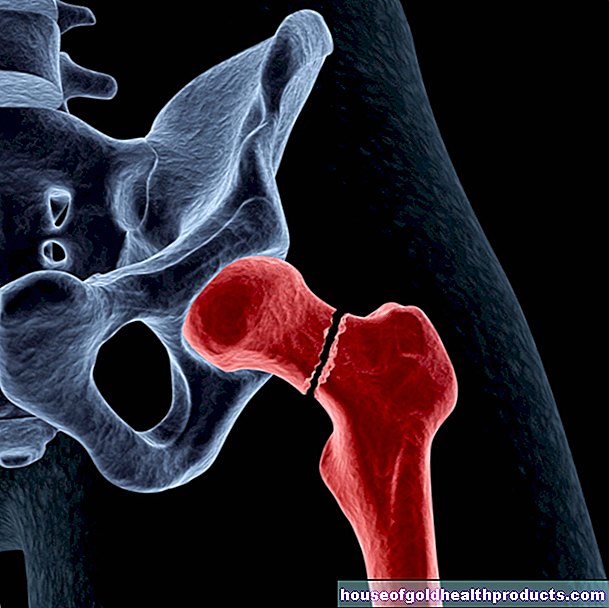
Bloody stool is a sign of bleeding in the digestive tract. The source of bleeding can be in the oropharynx, esophagus, stomach, small or large intestine or in the anus.
Bleeding in the upper digestive tract
If the blood in the stool comes from the upper digestive tract, the following may be considered:
- Gastrointestinal ulcers: Gastric ulcer and duodenal ulcer are the most common cause of upper digestive tract bleeding. It is often triggered by an infection with the Helicobacter pylori bacterium.
- Medication: Various medications can cause bleeding in the upper digestive tract if taken for a long time, for example the pain reliever and fever medication acetylsalicylic acid (ASA).
- Chronic heartburn: If aggressive stomach acid rises repeatedly into the esophagus, the lining of the esophagus can become inflamed (esophagitis or reflux esophagitis). The affected mucous membrane can then start to bleed.
- Liver diseases: Various diseases of the liver cause the venous blood flow to be diverted, which can lead to varicose veins in the esophagus (esophageal varices). These tear easily, which can be associated with life-threatening bleeding.
- violent vomiting: this can tear the mucous membrane between the stomach and esophagus. Doctors speak of Mallory-Weiss syndrome here. It often occurs in alcoholics with previously damaged mucous membranes.
- Stomach cancer: A malignant tumor in the stomach can also be the cause of blood in the stool.
Bleeding in the middle and lower digestive tract
Various conditions that affect the middle and lower digestive tract can also cause blood in your stool. These include:
- Tumors in the small or large intestine: They are the most common cause of bleeding in the middle and lower digestive tract. However, these tumors do not necessarily have to be malignant (colon cancer). There are also benign growths in the intestines that can be responsible for blood in the stool.
- Inflammatory bowel disease: Especially in younger people, blood in the stool can be caused by Crohn's disease or ulcerative colitis. While the latter only affects the colon and rectum, Crohn's disease can cause inflammation throughout the digestive tract. The exact causes of both diseases are not known.
- Intestinal polyps: These are predominantly benign protrusions of the mucous membrane in the large intestine. They usually do not cause any symptoms, but they can start to bleed as they grow in size. In addition, they can develop into the preliminary stage of colon cancer. Therefore, intestinal polyps above a certain size are usually removed. Postoperative bleeding may occur after such an operation.
- Diverticulum: Intestinal diverticula are protrusions of the intestinal wall (mostly in the large intestine). The clinical picture is called diverticulosis and is quite common. If the diverticula become inflamed (diverticulitis), they can start to bleed.
- Infections: From the common gastrointestinal flu to more serious illnesses such as typhoid or bacterial dysentery, various infections can cause blood in your stool. Usually diarrhea occurs at the same time.
- Pseudomembranous colitis: This is a form of colon inflammation caused by the overgrowth of certain intestinal bacteria (Clostridium difficile). The trigger is usually a longer antibiotic therapy. Typical symptoms of the disease are severe abdominal pain and diarrhea, often with blood in the stool.
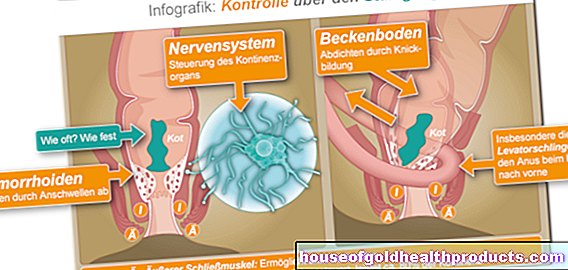
- Haemorrhoids: The spongy, well-perfused vascular cushion on the anus can be abnormally enlarged (haemorrhoidal disease) and thus tear open easily when defecating. Then you find fresh, mostly bright red blood on the stool.
- Mesenteric infarction: This is the acute occlusion of an intestinal vessel. Older people are mostly affected. Blood may appear in the stool as the disease progresses.
Blood in the stool: when do you need to see a doctor?
If you notice blood in your stool, it is important to see a doctor. Most of the time, the bleeding stops by itself and the causes are often harmless. Nevertheless, you should definitely clarify from which source the blood comes and whether there is possibly a more serious illness behind it. This is especially true if there are additional symptoms such as:
- Stomach or abdominal pain
- Painful bowel movements
- Nausea and vomiting (possibly with blood in the vomit)
- persistent fatigue and exhaustion
- significant weight loss in a short period of time
- Night sweats
Bleeding in the digestive tract can lead to anemia in the long term, which must be treated by a doctor in any case.
How to spot blood in stool
Blood in the stool indicates that blood is leaking somewhere in the digestive tract that has mixed with the stool. The color and texture of the blood can indicate the source of the bleeding. Blood in the stool is not necessarily light or dark red, it can also be black. Exactly what the blood looks like depends on how heavy the bleeding is in the digestive tract and whether or not the blood has come into contact with stomach acid or bacteria.
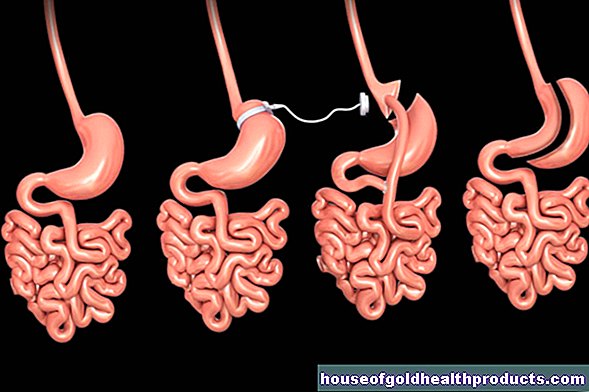
The gastrointestinal tract:

Red blood in the stool (hematochezia)
Light or dark red blood, either mixed with the stool or deposited in streaks, is relatively fresh. This type of blood in the stool is called hematochezia. The source of bleeding is usually in the middle or lower part of the gastrointestinal tract (gastrointestinal tract, GI tract), as the blood has not been broken down by stomach acid or bacteria and has been discolored as a result.
If the stool is evenly colored dark red, this may indicate increased bleeding in the colon. Weaker bleeding leaves more jelly-like marks in the stool.
Light red stripes can in turn indicate fresh bleeding in the rectum, as is typical for hemorrhoids.
Black blood in the stool (melena, tarry stool)
If the chair is black and shiny, it is called a tarry chair (Meläna). This usually indicates bleeding in the upper gastrointestinal tract, between the esophagus and the duodenum. This is because this is where the blood comes into contact with stomach acid, which breaks down the hemoglobin in the blood into hematin and thus turns the stool black. If those affected also suffer from vomiting, the vomit is also black like coffee grounds. Stomach ulcers are often responsible for bleeding in the upper digestive tract.
In addition to stomach acid, intestinal bacteria can also convert the hemoglobin in the blood into hematin upon prolonged contact. Therefore, if the intestinal passage is slowed, deeper bleeding can also lead to melena.
Under certain circumstances, bleeding in the upper gastrointestinal tract can also lead to red (instead of black) blood in the stool, i.e. hematochezia. This can be the case, for example, if little stomach acid is produced by medication or if a lot of blood leaks out, which quickly passes through the intestines.
Occult blood in the stool
If there is blood in the stool, but not visible to the naked eye, it is called occult blood in the stool. Usually this is discovered by chance during a basic examination or on suspicion in the case of known damage to the mucous membrane in the digestive tract.
Occult blood in the stool can be detected with an immunological stool test, which also reacts to the smallest amounts of blood. So far, the hemoccult test has been used for this.
Possible mix-up with blood in the stool
Some foods can discolor the stool, simulating blood in the stool. Red beets, for example, leave dark red marks in the stool, which can easily be mistaken for hematochezia. Blueberries and liquorice, on the other hand, color the stool black, similar to a tarry stool (melena).
Medicines such as charcoal and iron tablets can also cause black stools.
Blood in the stool: what does the doctor do?
For the doctor, it is first and foremost about determining the cause of the blood in the stool. Questions about the medical history (anamnesis) can provide important information about the source of the bleeding. For example, the doctor asks the patient whether he has had blood in his stool before and whether he has a previous illness (such as Crohn's disease, ulcerative colitis, hemorrhoids, stomach ulcer, etc.). The doctor can also inquire about the patient's alcohol consumption (alcoholism as a risk factor for gastrointestinal bleeding).
The interview will be followed by a physical exam. In addition, further examinations can help pinpoint the source of the bleeding. One of the most important is a gastrointestinal colonoscopy. Depending on your needs, other examinations can also be useful:
- Gastroscopy: In gastroscopy, a flexible tube with built-in optics (endoscope) is pushed over the mouth and into the stomach in order to examine the inside of the spies tube, stomach wall and the upper part of the first section of the small intestine (duodenum). In a colonoscopy, the endoscope is inserted through the anus into the rectum and further into the large intestine. This method can identify many possible sources of bleeding, such as esophageal varices, ulcers, chronic inflammation, diverticula, colon polyps, and other growths.
- Rectoscopy: If the doctor suspects hemorrhoids to be the cause of the blood in the stool, a reflection of the rectum is sufficient (rectoscopy).
- Double balloon enteroscopy (DBE): This type of endoscopy allows the doctor to examine the small intestine. To do this, he inserts an endoscope to which two small balloons are attached. The doctor alternately pumps these up so that the long endoscope can work its way into the small intestine. The examination is usually carried out in two steps: First, the doctor examines the upper part of the small intestine via the mouth, then the lower part via the anus.
- Video capsule endoscopy: For this special endoscopic examination, the patient swallows a mini camera. As it passes through the digestive tract, it takes pictures of the inside (especially of the small intestine) at short intervals. The method is completely painless, but time-consuming. In addition, the source of the bleeding cannot be clearly localized with it.
- Ultrasound examination: Using an ultrasound examination of the abdominal wall, the doctor can often identify a blockage of an intestinal vessel (mesenteric infarction) as the cause of the blood in the stool.
- Nuclear medicine procedures and selective arteriography: With these examination methods, vessels can be visualized more precisely with the aid of contrast media in order to detect active bleeding.
- Stool and blood samples: These can be used, for example, to identify infections as triggers for the blood in the stool.
This is how the doctor treats
For the first treatment, the patients are laid flat. They receive oxygen through a nasogastric tube. Blood substitutes replenish the missing volume in the bloodstream. If there is more blood loss, those affected receive blood transfusions.
Further treatment depends on the cause of the bleeding. The primary aim, of course, is to stop active bleeding. In addition, recurring bleeding should be prevented by tackling the cause.
To stop active bleeding in the digestive tract, various endoscopic procedures are primarily available. It is practical here that a source of bleeding discovered with the help of a gastroscopy or colonoscopy can be treated immediately during the examination. The doctor has various options for doing this:
- Hemoclip: The doctor can close the bleeding area with a kind of clamp that compresses the injured vessel.
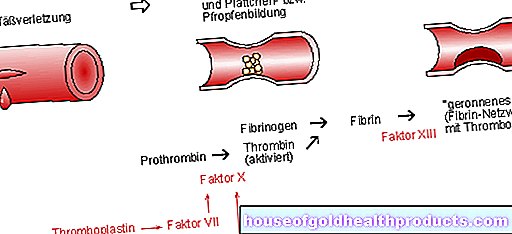
- Adrenaline solution or fibrin glue: Alternatively, the bleeding source can be injected with an adrenaline solution. This causes the vessels to contract at the appropriate point.So-called fibrin glue can also be injected. Fibrin is a protein that is important for blood clotting.
- Laser: Sometimes the doctor will obliterate the bleeding area with a laser.
- Piercing: In other cases, the source of the bleeding is pierced with minimal surgery. That is, sutures are placed around the injured vessels to stop the bleeding.
- Rubber band ligation: If esophageal varices or hemorrhoids have triggered the bleeding, medical professionals often use rubber band ligation. The affected vessels are tied off with a rubber band so that they die.
In the event of acute bleeding in the gastrointestinal tract with severe blood loss, the lost blood must be replaced as soon as possible. Otherwise life-threatening hypovolemic shock can result.
Once the bleeding has stopped, it is important to treat the cause to prevent it from re-bleeding. Some examples:
- Stomach ulcers: As they are often caused by an infection with the Helicobacter bacterium, patients are usually given antibiotics. In addition, gastric acid-inhibiting drugs such as proton pump inhibitors (PPIs) are often used to protect the gastric mucosa from further damage.
- Esophageal varices: They occur when the pressure in the portal vein (which brings blood from the abdominal organs to the liver) is increased (portal hypertension). Those affected are therefore treated with antihypertensive drugs, among other things.
- Chronic Inflammatory Bowel Disease: You are treated with anti-inflammatory drugs such as glucocorticoids ("cortisone").
- Diverticulitis: For inflamed intestinal protuberances, the doctor often prescribes antibiotics and anti-inflammatory drugs. In severe cases, an operation may be necessary: The diseased intestinal section is removed.
- Colon polyps: They are also usually removed surgically.
- Malignant diseases such as colon cancer: The main therapeutic options here are surgery, chemotherapy and radiation therapy.
Blood in the stool: you can do this yourself
If you notice blood in your stool, you should always consult a doctor to clarify the cause quickly. Treatment is also a matter for the doctor. Under certain circumstances, however, you can support the therapy. If you have an acute gastric ulcer, for example, you should avoid anything that further irritates the gastric mucosa. These include, for example, coffee, nicotine, alcohol, hot spices and stress. Ask your doctor how you can support conventional medical treatment.
In addition, a lot can be done to prevent (re) bleeding in the gastrointestinal tract - and thus blood in the stool. Diet has a major influence. By following these tips, you can reduce your personal risk of gastrointestinal bleeding:
- Lots of fruit and vegetables: Put apples, carrots, etc. on your diet regularly. In this way you counteract stomach and intestinal cancer as well as diverticula.
- Less meat: For the sake of your health, eat less meat and sausage products.
- Fiber-rich diet: Consume fiber regularly, such as that found in whole grain products. They promote digestion.
- Fatty foods: Avoid fatty foods as they often lead to excess stomach acid, which in turn can cause heartburn and ulcers.
- No alcohol and nicotine: These luxury foods also stimulate the release of gastric acid. Therefore you should do without them.
In addition to diet, psychological factors also play a role: Avoiding chronic stress can also prevent gastrointestinal bleeding and thus blood in the stool.
Additional information
Guidelines:
- Guideline "Guideline Gastrointestinal Bleeding" of the German Society for Gastroenterology, Digestive and Metabolic Diseases