Pleural effusion
and Sabine Schrör, medical journalistMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts
Sabine Schrör is a freelance writer for the medical team. She studied business administration and public relations in Cologne. As a freelance editor, she has been at home in a wide variety of industries for more than 15 years.Health is one of her favorite subjects.
More about the experts All content is checked by medical journalists.With a pleural effusion, more fluid collects in the pleural cavity, the gap-shaped space between the lungs and the chest. Moist pleurisy (pleurisy) is usually responsible for this. Depending on how pronounced the pleural effusion is, the symptoms vary in severity - from slight pain to shortness of breath. Read more about the signs, causes, diagnosis and treatment options of pleural effusions here.

Brief overview
- What is a pleural effusion? Excessive build-up of fluid in the pleural cavity in the chest. Differentiation between transudates (low-protein pleural effusions) and exudates (high-protein pleural effusions).
- Symptoms: With small pleural effusions usually no symptoms. For larger effusions z. B. Difficulty breathing, tightness in the chest, possibly breathing-dependent chest pain (chest pain), cough (when the lung is irritated), water retention (edema) in the legs, nocturnal urination (nocturia) with pronounced pleural effusion.
- Causes: heart weakness, liver weakness, kidney weakness with transudates. For exudates z. B. inflammations, tumors, pulmonary embolism, abdominal diseases such as inflammation of the pancreas (pancreatitis), accumulation of pus below the diaphragm (subphrenic abscess), injuries in the chest area such as broken ribs.
- Diagnosis: anamnesis, physical examinations (e.g. tapping the chest), imaging procedures such as ultrasound, x-rays, computed tomography (CT), pleural puncture, blood test.
- Therapy: Treatment of the underlying disease that caused it. In the case of severe pleural effusions with severe symptoms, additional treatment methods such as relief puncture (pleural puncture), chest drainage, pleurodesis (obliteration of the pleural space).
Pleural effusion: description
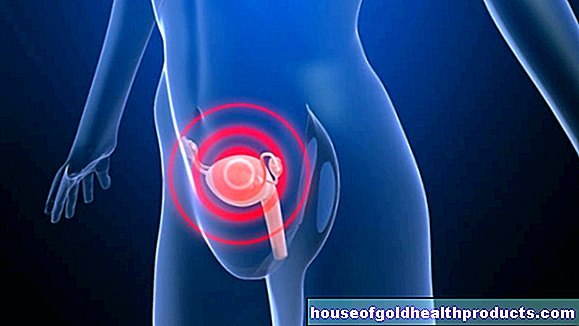
With a pleural effusion, fluid collects in the pleural cavity (pleural space). This is a gap-shaped space between the two pleural leaves, which together form the pleura (pleura) - a firm covering of connective tissue that surrounds the lungs and lines the inner chest cavity. The pleural cavity and pleural leaves are collectively called the pleura.
Usually the pleural cavity only contains some lubricating fluid. This so-called pleural fluid ensures that the pleural leaves slide smoothly past each other when you inhale and exhale.
In healthy people, the release (secretion) of new pleural fluid (via lymph and blood vessels) and its resorption (absorption) are in balance. But if this balance is disturbed, a pleural effusion develops: Either the lymph or blood vessels then release too much fluid into the pleural cavity or they take in too little from it. There are many reasons for this (see below).
Pleural effusion: types
Depending on how the pleural fluid is composed, a distinction is made:
- Transudates: low-protein pleural effusions. They occur, for example, with left heart failure (left heart failure) or as a result of liver cirrhosis.
- Exudates: Protein-rich pleural effusions. They can usually be traced back to inflammation or tumors. The exudates include the hemothorax (bloody pleural effusion) and the chylothorax (lymph-containing pleural effusion).
Pleural effusion: signs
A small pleural effusion does not cause any discomfort and usually goes unnoticed. Only when fluid increasingly collects in the pleural space do those affected feel symptoms. Because the more fluid the pleural cavity contains (in extreme cases several liters), the less space the lungs have to expand when inhaling.
Typical signs of a pleural effusion include:
- Shortness of breath
- Chest tightness
- possibly breath-dependent chest pain (chest pain)
- Cough (if the inner pleural leaf = pulmonary membrane is irritated)
- Water retention (edema) in the legs
- Urination at night (nocturia) with pronounced pleural effusion
Pleural effusion: causes
The most important causes of a transudate (low protein pleural effusion) are:
- Heart failure: Above all, heart failure of the left heart (left heart failure) can cause a protein-poor pleural effusion.
- Liver weakness: Liver insufficiency is also a possible cause of a transudate.
- Kidney diseases: Both kidney weakness (renal insufficiency) and a nephrotic syndrome (symptom complex consisting of protein in the urine, increased blood lipid levels and water retention in the arms and legs) can be the cause of a protein-poor pleural effusion.
The most important causes of an exudate (protein-rich pleural effusion) are:
- Inflammations: e.g. pneumonia, pleurisy (pleurisy) or tuberculosis (often leads to bloody exudate).
- Tumors: e.g. tumors in the pleura (pleural metastases, pleural mesothelioma), lymph gland cancer or lung cancer (often leads to a bloody pleural effusion).
- Pulmonary embolism: A blood clot that has washed up blocks a pulmonary vessel. The result can be a bloody pleural effusion.
- Diseases of the abdomen: e.g. inflammation of the pancreas (pancreatitis), accumulation of pus below the diaphragm (subphrenic abscess).
- Injuries in the chest area: e.g. broken ribs. Such injuries usually lead to a bloody pleural effusion. If the body's largest lymph vessel (thoracic duct) ruptures, a lymph-containing pleural effusion (chylothorax) develops.
Pleural effusion: when should you see a doctor?
Basically, every pleural effusion should be clarified by a doctor. If you suffer from breathlessness, pain and / or tightness in the chest area, you should definitely consult a doctor.
Pleural effusion: what does the doctor do?
First, the doctor will take the medical history (anamnesis). For example, he asks what ailments you are suffering from and how long they have existed. You should also inform the doctor about basic and previous illnesses as well as possible accidents and injuries.
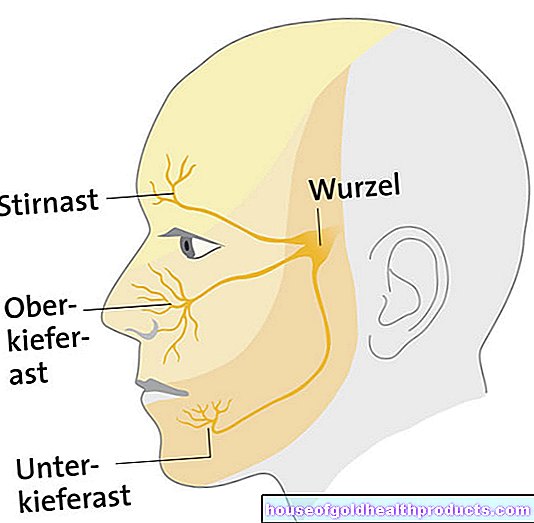
This is followed by a physical examination. The doctor will tap your chest, among other things, because a muffled tapping sound is typical for a pleural effusion. In addition, the doctor can determine whether the breathing sound is clearly audible. If not, this could also indicate a pleural effusion.
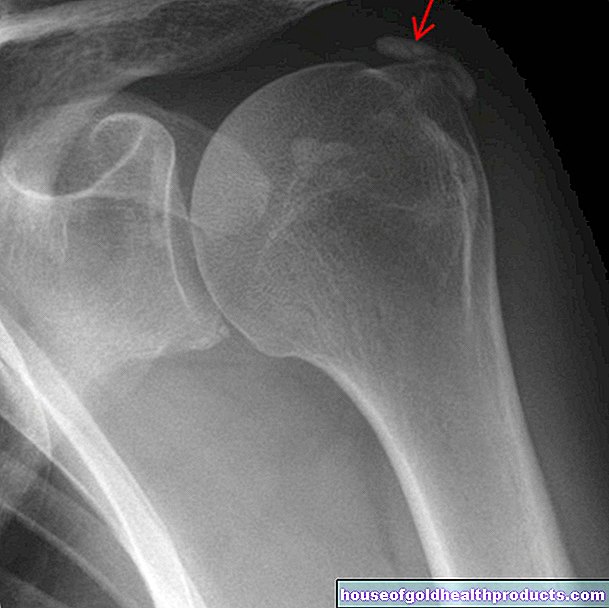
The suspicion of a pleural effusion can be confirmed by means of imaging procedures: pleural effusions can be detected on ultrasound from a fluid volume of ten to 20 milliliters, on the X-ray from around 300 milliliters. Sometimes computed tomography of the chest (thoracic CT) is also done: It can detect pleural effusions from around 70 milliliters. The imaging tests also often tell the doctor the cause of a pleural effusion, such as a heart or lung disease.
If the reason for the accumulation of fluid in the pleural space cannot be determined with imaging procedures, the doctor performs a pleural puncture: under local anesthesia and ultrasound control, he pushes a hollow needle into the effusion and removes some fluid. This is examined in the laboratory for pathogens, blood components and cancer cells. In addition, the composition and color of the pleural fluid are determined - aspects that provide valuable information about the possible cause of the pleural effusion.
The basic diagnosis also includes a blood test (blood count, blood sugar, etc.).
This is how the doctor treats a pleural effusion
The starting point is the therapy of the underlying disease (pneumonia, tuberculosis, heart failure, etc.). Smaller pleural effusions often recede on their own.
A larger pleural effusion, on the other hand, requires a rapid discharge puncture (pleural puncture): The doctor sticks a hollow needle into the effusion and sucks off a large amount of fluid. A single puncture is often sufficient.
However, if a new pleural effusion is to be expected quickly afterwards, or if it is a concomitant effusion from longer-lasting diseases (such as cancer), a chest drain is sometimes placed: the doctor inserts a drainage tube into the pleural space to remove the excess Liquid drains away. The tube can stay in place for a longer period of time, which saves a repeated puncture.
In the case of a malignant pleural effusion (i.e. a pleural effusion as a result of a tumor disease), the pleural space is usually obliterated (pleurodesis): To do this, the doctor first sucks off the pleural fluid. He then injects a special substance into the pleural space. The active ingredient triggers inflammation of the two pleural leaves, which then stick together. So new liquid can no longer flow into the gap.
In the case of a chylothorax (lymph-containing pleural effusion) caused by a tear in the central lymphatic vessel (thoracic duct), an attempt is made to surgically close the injured vessel. If this is not possible, there are two options: Either the patient receives a chest tube and special nutritional guidelines (special fat-modified diet) or a pleurodesis is performed.
Pleural effusion: you can do this yourself
Behind the symptoms of a pleural effusion, especially painful breathing, there can always be an initial illness. Therefore, consult a doctor at an early stage.
Tags: unfulfilled wish to have children travel medicine magazine