Radiculopathy
and Carola Felchner, science journalistMarian Grosser studied human medicine in Munich. In addition, the doctor, who was interested in many things, dared to make some exciting detours: studying philosophy and art history, working on the radio and, finally, also for a Netdoctor.
More about the expertsCarola Felchner is a freelance writer in the medical department and a certified training and nutrition advisor. She worked for various specialist magazines and online portals before becoming a freelance journalist in 2015. Before starting her internship, she studied translation and interpreting in Kempten and Munich.
More about the experts All content is checked by medical journalists.Radiculopathy is damage to or irritation of a nerve root. This is the name given to the nerve cells in the back where they enter or leave the spinal cord. In addition to pain, radiculopathy can also cause loss of sensation and symptoms of paralysis. Disc herniations are often the trigger. Other possible causes include changes in the bony spine and inflammation. Read everything you need to know about radiculopathy, how to diagnose and treat it!

Brief overview
- Description: Damage or irritation of the nerve root with pain, symptoms of paralysis, loss of sensation
- Causes: mostly pressure on the nerve root or inflammation, among others. Herniated discs, bony spinal changes, osteoarthritis, slipping vertebrae, tumors, hemorrhages
- When to the doctor in the case of persistent back pain, especially if the pain is radiating, numbness and / or symptoms of paralysis
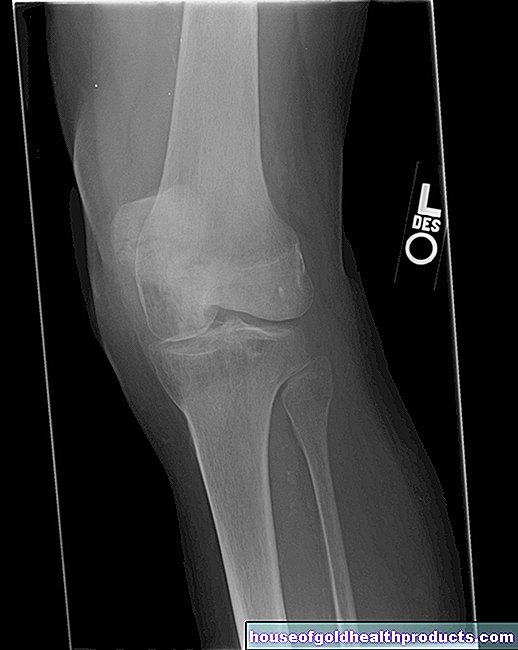
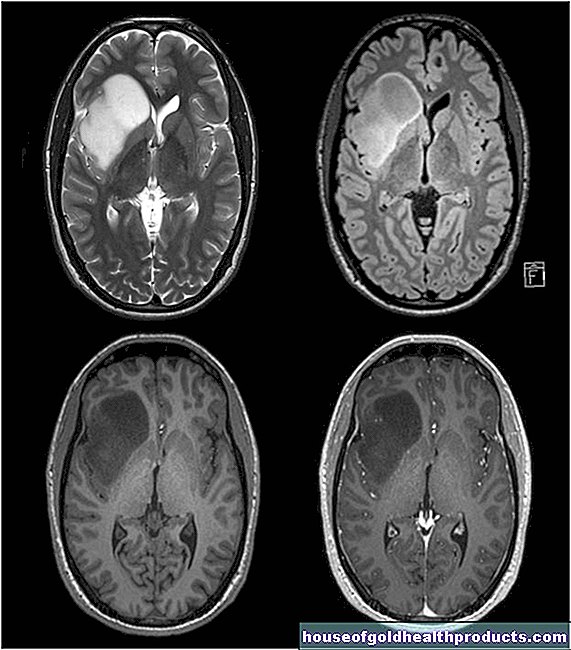
- Diagnostics: consultation with the patient, physical examination (e.g. test of strength, sensitivity and reflexes), possibly computer tomography, magnetic resonance tomography, x-rays, electromyography (EMG)
- Therapy: depending on the cause and severity of the symptoms, medication (e.g. pain relievers, muscle relaxants, possibly cortisone or antibiotics), physiotherapy, massages, physical heat treatment, rarely surgery
- Tips: Train your back muscles, pay attention to back-friendly behavior in everyday life (e.g. correct lifting, correct sitting posture, etc.)
Radiculopathy: description
In medicine, radiculopathy is the general term used to describe complaints that arise from damage to or irritation of a nerve root. If several nerve roots are affected, one speaks of a polyradiculopathy.
Radiculitis is in itself the inflammation of a nerve root. However, the term is often used synonymously with radiculopathy. Other alternative names are root neuritis or root syndrome.
What is a nerve root?
Nerve roots are nerve fibers that enter or exit the spinal cord. A distinction is made between an anterior and a posterior root, which connect to form a spinal nerve while still in the spinal canal. The spinal nerves in turn emerge from the spinal canal in pairs on the right and left between the vertebral bodies. A person normally has 31 pairs of spinal nerves, i.e. 31 front and rear roots on each side of the body.
Depending on which area of the body and the brain a signal exchange takes place, this takes place at different heights of the spinal cord. For example, nerve roots in the cervical spine are responsible for the arms and nerve roots in the lower part of the spinal cord, which in adults ends at the level of the uppermost lumbar vertebrae, are responsible for the legs.
Each anterior root supplies certain muscles with nerve signals, each posterior root receives nerve stimuli from specific organ or skin sections. When a nerve root is damaged, typical symptoms corresponding to its height occur. Thus, based on the symptoms, it is usually quite easy to assess the level of the radiculopathy.
What types of radiculopathy are there?
Radiculopathies can be classified according to the level of the spinal cord at which they occur. If nerve roots in the area of the cervical spine are affected, one speaks of a cervical radiculopathy, in the case of complaints that can be assigned to the lower nerve roots, of a lumbar or sacral radiculopathy.
The lumbar and sacral areas are affected by radiculopathy much more frequently than the cervical area of the spinal cord. A root syndrome at the level of the thoracic spine (thoracic radiculopathy) is also possible, but relatively rare.
If you look at the duration of a radiculopathy, you can distinguish between acute and chronic forms. One speaks of chronic radiculopathy if the symptoms (above all the pain) persist for more than twelve weeks.
What are the symptoms of radiculopathy?
Radiculopathy very often leads to shooting pain and / or abnormal sensations such as tingling near the nerve root itself and in the area where it is supplied. Leg pain, for example, is typical for radiculopathy in the lumbar spine. In cervical radiculopathies, the symptoms often radiate to the shoulders and arms.
In addition to pain, numbness of the skin often accompanies radiculopathy. Symptoms of paralysis and decreased reflexes in the associated muscles can also occur.
Radiculopathy does not usually lead to complete paralysis, as each muscle receives impulses from several nerve roots.
At the level of the affected nerve root, the back muscles next to the spine are often hardened (hard tension). In addition, the pain increases when the patient presses, such as when coughing, sneezing or defecating. Tapping the spine at the appropriate point is also painful. With cervical radiculopathy, those affected sometimes also show an extended position of the neck.
Who Does Radiculopathy Affect?
Depending on the trigger, radiculopathy can occur at different ages. But since many of the possible triggers only develop with increasing age, young people are rarely affected by radiculopathy and children almost never.
The most common cause of root syndrome is a herniated disc in the lumbar spine. This occurs most often between the ages of 30 and 50. After that, the risk decreases again. Herniated discs in the cervical spine are much less common, but they occur mainly in younger people.
Radiculopathy: causes and possible diseases
Most of the causes of radiculopathy can be assigned to two broad groups: either there is some form of mechanical pressure on the nerve root, or it is inflammation that leads to the symptoms.
Mechanical causes are the most common. This includes:
- Herniated discs
- bony changes in the spine, e.g. B. a narrowing of the spinal canal (spinal stenosis) or the nerve exit points
- Arthrosis of the vertebral joints (spondylarthrosis, facet joint arthrosis)
- Vertebral gliding (spondylolisthesis)
- Masses such as tumors or hemorrhages
In the event of mechanical damage to the nerve root, inflammatory processes often set in after some time, which cause additional irritation.
The triggers of an inflammatory radiculopathy, on the other hand, are usually pathogens such as viruses or bacteria. These include, above all, the herpes zoster virus (pathogen causing chickenpox and shingles) and special Borrelia (triggering Lyme borreliosis).
Inflammation of the vertebral bodies and intervertebral discs (spondylodiscitis) can also spread to the nerve roots. It is often caused by the bacterium Staphylococcus aureus. One possible trigger for non-infectious inflammation of a nerve root is Guillain-Barré syndrome, an inflammatory disease of the nerves due to a misdirected immune system reaction.
Finally, there are also certain diseases that directly destroy the tissue of the nerve roots without causing inflammation. An example of this is radiculopathy in diabetes mellitus (diabetic radiculopathy).
Pseudoradicular Syndromes
The symptoms of some diseases can be very similar to radiculopathy, although no nerve roots are affected. In most cases, these are orthopedic diseases such as hip arthrosis or vertebral fractures as a result of osteoporosis (bone loss). If symptoms similar to those of an actual radiculopathy occur, we speak of pseudoradicular syndromes.
Radiculopathy: when do you need to see a doctor?
Back pain is a very common phenomenon, especially with increasing age, and is often the result of wear and tear on the spine. However, if your back pain persists, you should always consult a doctor to clarify the cause.
Especially if the pain radiates and there may also be abnormal sensations, numbness or signs of paralysis, there can also be an acute process behind it that requires immediate treatment.
You must act in a hurry if certain warning symptoms occur. These so-called "red flags" include:
- new or increasing symptoms of paralysis
- decreasing pain with simultaneous symptoms of paralysis
- Pain intensification at night
- a previous trauma, such as a fall or accident. In older people, even harmless falls can cause vertebral fractures.
Such symptoms indicate a medical emergency that needs to be treated immediately! Call the ambulance!
Radiculopathy: What Does the Doctor Do?
First of all, the doctor collects the patient's medical history (anamnesis) in conversation with the patient. For this purpose, the type, location and intensity of the pain and other complaints can be described in detail. He also asks about any previous or underlying illnesses (shingles, herniated discs, diabetes, etc.) and previous injuries / accidents.
This is followed by a physical exam. This includes, in particular, strength tests and tests of sensitivity and reflexes. If necessary, this is followed by further examination methods:
For example, the doctor can request x-rays of the spine. Sometimes computed tomography (CT) or magnetic resonance imaging (MRI) is also performed - but usually only if the above-mentioned red flag symptoms occur. Another method that is used to more closely examine nerve damage is so-called electromyography (EMG), in which the natural electrical muscle activity is measured using needle or adhesive electrodes.
Radiculopathy: Therapy
When treating a radiculopathy, the first priority is to relieve the pain. There are various medications for this, whereby the doctor begins with the administration of weaker painkillers such as paracetamol or ibuprofen (non-opiodal or non-steroidal analgesics). If these active ingredients are insufficient, weak opioid pain relievers such as tramadol or tilidine can also be given. So-called muscle relaxants relieve any muscle tension that is often associated with radiculopathy. In certain cases, additional medication is necessary, such as cortisone preparations or antibiotics (in bacterial infections that cause radiculopathy).
In addition to drug-based radiculopathy therapy, there are also some special treatment methods that can be used either in addition or as an alternative. With the help of physiotherapeutic exercises, the patient can, for example, prevent misalignments and create more mobility. Massage can help loosen muscle tightness, as can physical heat treatments.
Contrary to the imagination of many patients, one should avoid bed rest whenever possible. In fact, it is usually beneficial for the healing process if the patient moves early and regularly. Bed rest should therefore be avoided at least four days after the symptoms appear. This requires early pain relief (painkillers, massage, etc.).
In many cases, apart from alleviating the symptoms, no further treatment is initially required. The symptoms often go away on their own after a few days to weeks.
If a mechanical cause is the cause of a radiculopathy and the patient experiences one or more of the red flag symptoms, it is usually necessary to operate quickly to prevent permanent neurological damage. Otherwise, people tend to be cautious about surgical interventions today.
It is also important to prevent the patient from developing chronic radiculopathy (chronification of the symptoms). Since psychological factors such as the patient's expectations also play a role in this regard, it is important that you, the patient, understand your illness and the treatment options well. Ignorance often creates fear and negative expectations increase the risk of the symptoms becoming chronic.
Radiculopathy: What Can You Do By Yourself?
In order to prevent radiculopathy or to prevent further symptoms of this kind, you should train your back muscles regularly (initially under the guidance of a physiotherapist or specially trained fitness trainer and later independently). A strong muscle corset gives the back stability and reduces signs of wear and tear on the spine.
You should also try to be gentle on your back in everyday life by, for example, not lifting "off your back", but rather stepping out of your legs, and making sure you are sitting correctly. These measures will reduce the risk of radiculopathy and other back problems.
Tags: interview menshealth parasites





















.jpg)