Organ donation
Updated on All content is checked by medical journalists.Organ donation is the transfer of an organ from an organ donor to a recipient. The donor can donate organs either after their death or during their lifetime (e.g. kidneys). Read everything you need to know about organ donation, how it is regulated and what you need to consider after receiving a donor organ.

What is organ donation?
Organ donation refers to the transfer of an organ or parts of an organ from an organ donor to a recipient. The aim is either to enable a sick person to survive or to improve their quality of life. If you want to become an organ donor, all you have to do is document your decision in writing, for example in an organ donor card. Discuss your wishes with your relatives as well.
Further information: Organ donation card
Why it makes sense to fill out an organ donation card and where you can get it from can be found in the article Organ donation card.
A distinction is made between post-mortem organ donation and living donation: Post-mortem organ donation refers to the donation of organs after death. The prerequisite is the clear determination of brain death in the donor. In addition, the consent of the deceased himself or his relatives must be available.
In the case of living donation, a living person donates an organ or part of it. Suitable organs are, for example, one of the two kidneys or part of the lungs, the liver, the small intestine or the pancreas. In Germany, however, only living donations of kidneys and parts of the liver are allowed. In order to prevent organ trafficking, a living donation may only be made if it is intended for one of the following groups of people:
- Spouse, fiancée, registered life partner
- First or second degree relatives
- other people close to the donor
In addition, a living donation must be voluntary and can only be offered by adults.
Which organs can be donated?
In principle, the following organs can be used as donor organs:
- heart
- lung
- liver
- kidney
- pancreas
- colon
Aside from organ donation, patients can also benefit from tissue donation. These include:
- Cornea of the eyes
- heart valves
- skin
- Blood vessels
- Bone, cartilage and soft tissue
Organ donation: age limit
In order to be allowed to donate organs, only the condition of the organs is decisive, not the biological age. Of course, the health of younger people is often better than that of the elderly, but the functioning organ of a 70-year-old can also be successfully transplanted. This is especially true if the organ goes to an older recipient.
There is no lower age limit for the donation, but the decision for children under 14 is up to the parents. From their 14th birthday onwards, children can object to organ donation on their own, and from their 16th birthday onwards they can also consent.
Organ donation: criticism
There is a rather skeptical attitude towards organ donation among the population. In recent years, criticism has been triggered primarily by organ donation scandals, in which patients were given preference in organ allocation by manipulating the waiting list. In the course of this, the Transplantation Act was revised in 1997 with the aim of increasing the transparency of organ allocation. In particular, the penalty for doctors who deliberately violate the guidelines has been increased: Such doctors can now be punished with a fine or imprisonment of up to two years.
Organ allocation via the Eurotransplant Foundation is based on the urgency and prospect of success of a transplant. The recipient's financial situation does not matter. The Transplantation Act also prohibits organ trafficking and makes both selling an organ and receiving a purchased organ a criminal offense.
Regarding the concerns about post-mortem organ donation: The argument that brain death in the organ donor cannot be unequivocally determined can be refuted - with the aid of the prescribed examinations, brain death can be determined medically without any doubt.
Organ removal always takes place with the same surgical care as an operation on a living patient. After the operation, the surgeon closes the body again and the body is handed over to the relatives without any disfiguring injuries.
Organ donation: ethics
The subject of organ donation raises many ethical aspects, in particular whether a person's brain death justifies the removal of their organs. In 2015 (last change in 2021), the German Ethics Council issued a statement in which it considers organ removal for transplantation purposes to be acceptable - provided that the donor or his relatives have given their consent.
Another ethical problem is the fair distribution of donated organs. It is based on the basic principle of the greatest possible medical benefit. This means that the patient who needs the organ most urgently and has the greatest chance of healing receives the organ available. There is broad consensus in society that financial aspects or the social position of a patient should not play a role in the distribution.
Organ donation: pros and cons
There are many motivations for deciding for or against organ donation. Frequent reasons for rejection are a lack of trust in the allocation system or - in the case of living donations - fears of distortion or health disadvantage. Spiritual or religious reasons usually do not play a role, as none of the larger religious communities in Germany has so far spoken out against organ donation.
For many relatives of dead organ donors, the knowledge that they have helped a sick person with donor organs helps them cope with the grief over the loss of a loved one.
The important thing is: The decision "Organ donation: yes or no?" everyone has to meet for themselves. It is helpful to deal with the topic and to document your will or to discuss it with the relatives. In Germany - in contrast to most other European countries - there is a decision-making system, a modification of the consent system:
Organs of a deceased person may only be removed if the person concerned has expressly allowed this himself during his lifetime or if the surviving dependents explicitly consent to the organ donation. In addition to Germany, this regulation also applies in Northern Ireland. There is an extended consent regime in Denmark, Ireland, Iceland, Lithuania, Romania, Switzerland and the United Kingdom, in which the next of kin or authorized representative decide if there is no documentation of the deceased person.
Many other countries (e.g. Spain, Italy, Austria, Hungary, England with Wales and Scotland) comply with the objection regulation: Here, every deceased person becomes an organ donor if he has not expressly decided against it during his lifetime and has also documented this in writing. The relatives have no say in this.
In Germany, if the patient's will is not documented, the relatives must decide to the best of their knowledge and belief.
When do I need an organ donation?
Organ donation is often the only life-saving therapy for chronic or sudden organ failure. Organ donation may be an option for the following clinical pictures:
- End stage cirrhosis of the liver
- Liver cancer
- severe organ damage due to iron storage disease (hemochromatosis) or copper storage disease (Wilson's disease)
- Current liver failure (fungal poisoning, diseases and malformations of the biliary tract)
- Diabetes mellitus (type I or type II) with kidney damage
- polycystic kidney disease
- chronic nephritic syndrome (a disease of the kidneys)
- congenital heart defects
- Valvular heart disease
- Coronary heart disease (CHD)
- Heart muscle disease (cardiomyopathy)
- Heart failure (heart failure)
- functional disorders of the intestines
- chronic obstructive pulmonary disease (COPD)
- Pulmonary fibrosis
- Cystic fibrosis
- Sarcoid
- "Pulmonary hypertension" (pulmonary hypertension)
What do you do with an organ donation?
The process of organ donation is stipulated by law and follows a precise scheme.
Process of post-mortem organ donation
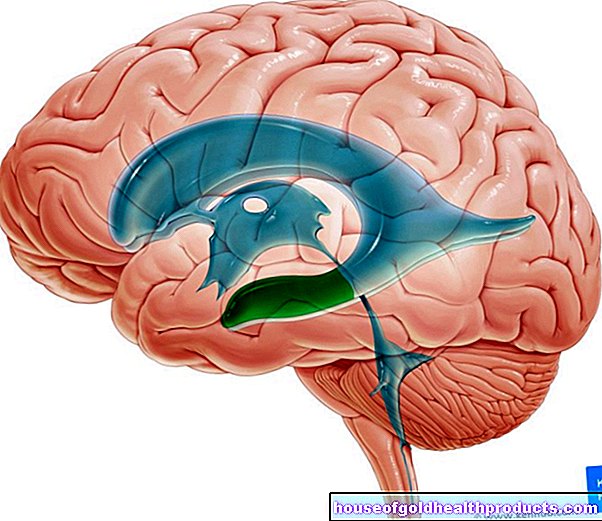
Before a patient can be considered a donor, he must be clearly diagnosed as having brain death. The doctor informs the German Organ Donation Foundation (DSO), which then arranges independent neurologists to determine brain death. According to the Transplantation Act, two doctors must independently determine whether the patient is brain dead. This is done according to a fixed three-stage scheme:
- Evidence of severe, incurable and irreversible damage to the brain
- Determination of unconsciousness, the ability to breathe independently and the failure of the reflexes controlled by the brain stem
- Verification of irreversible brain damage through examinations after prescribed waiting times
The doctors record the course of the examinations and their results in a protocol sheet, which can also be viewed by the relatives of the deceased.
If brain death is determined, the consent of the deceased to donate organs must be clarified. If there is no written documentation of his will (e.g. living will or organ donation card), the relatives must decide.
If the patient or their relatives have given their consent to organ donation, the DSO initiates various laboratory tests on the deceased. They are used to rule out contagious diseases that could be transmitted to a donor. Blood group, tissue characteristics and the functionality of the organ to be donated are also tested. In addition, the DSO informs Eurotransplant, which searches for a suitable recipient based on medical criteria such as the likelihood of success and urgency of the transplant.
Living donation process
Are you thinking about donating an organ to a loved one? Then you should first contact the doctor in charge of the transplant or dialysis center. In an initial discussion, it can be clarified whether a living donation is actually possible in the present case. The final instance in this examination is the living donation commission, which is usually affiliated with the state medical association.
If you meet all legal and health requirements for a living donation, the doctor will explain the risks of the procedure and the donation. Only then can you, as a potential donor, make an informed decision. If it turns out positive, you and the organ donor recipient will be admitted to the hospital and examined again. The transplant usually takes place the following day.
First of all, the surgeon begins to remove the donor organ. Shortly before the end of the procedure, the recipient's operation begins in parallel, so that the donor organ can be implanted directly with the least possible loss of time.
What are the risks of organ donation?
The removal of an organ or part of an organ harbors general risks for a living donor, such as can occur with any operation:
- Wound healing disorders
- Scarring with an unaesthetic result
- Bleeding
- Injury to nerves
- Wound infection
- Incidents of anesthesia
It has not yet been clarified whether kidney donation increases the risk of patients suffering from high blood pressure or increasing protein loss in the urine (proteinuria) in the future.
What do you have to consider after an organ donation?
The transplant center is a central point of contact for living donors and their relatives before and after organ donation.
After post-mortem organ donation
After a post-mortem organ donation, the body is handed over to the relatives for burial. If desired, the relatives can also be looked after by employees of the German Organ Transplantation Foundation (DSO). After a while you will be informed by the DSO about which organs have been transplanted and with what success this has happened. However, you will not receive any information about the recipient's name or illness.
After living donation
If there are no complications, you as a donor can go home after ten to 14 days. After a kidney or liver donation, you can expect about one to three months of incapacity for work - depending on the physical strain at work.
The organ recipient has to stay longer in the hospital so that it can be monitored and checked whether the new organ is back to work.
As a donor, you usually do not have to expect long-term health problems. Regular examinations ensure that any late effects of organ removal can be identified and treated in good time. Ask the transplant center for advice on how often you should go for follow-up care after an organ donation.
Tags: drugs gpp travel medicine

















.jpg)