transplantation
Updated on All content is checked by medical journalists.A transplant is the surgical grafting of tissues, organs or parts of the body. The transplants can come from other people as well as from the patient himself. A transplant is necessary in the event of irrevocable organ failure or serious injuries. Read everything you need to know about the procedure, when it will be done, and the risks involved.

What is a transplant?
In a transplant, the surgeon transplantes individual cells, tissues, organs or even entire parts of the body. According to the origin of these transplants, doctors differentiate between different types of transplantation:
- Autologous transplant: the donor is also the recipient. This can be the case with extensive burn injuries - the burn wounds are covered with a large piece of skin that is removed from another part of the body.
- Allogeneic transplant: the donor receives a transplant from another person. This has either already died (post-mortem organ donation) or is still alive (living donation).
- Xenogenic transplantation: Here the patient receives a transplant from an animal (for example the heart valve of a pig).
Organs and tissues that can be transplanted
The first transplant that was permanently successful was carried out by American surgeons in Boston in 1954. At that time, the recipient received a kidney from his twin brother. The following organs or tissues can basically be transplanted today:
- heart
- lung
- liver
- kidney
- Small intestine
- Pancreas or its cells
- Cornea of the eye
- Bone marrow cells
- Auditory ossicles
- Skin, tendons, bones and cartilage cells
- extremities
In the meantime, the first child was born after a uterine transplant. This gives some unwanted childless women a new way of fulfilling their desire to have children.
A hair transplant is used for burn injuries, for example.
When do you do a transplant?
A transplant is always necessary when the function of an organ has been irretrievably lost and there is no longer any other treatment option. This is the case, for example, with the following illnesses or injuries:
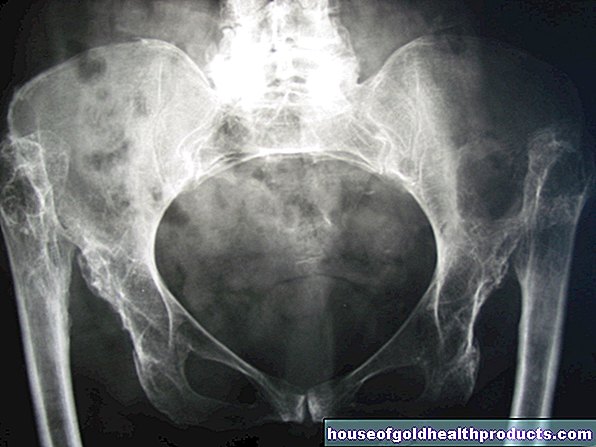
- complete loss of function of the kidneys
- Heart failure (heart failure)
- Cirrhosis of the liver
- Chronic obstructive pulmonary disease (COPD)
- severe burns or injuries to the skin and extremities
- severe forms of insulin-treated diabetes mellitus
- Blood cancer (leukemia)
- Recovery from skin cancers
What do you do with a transplant?
Post-mortem organ donation
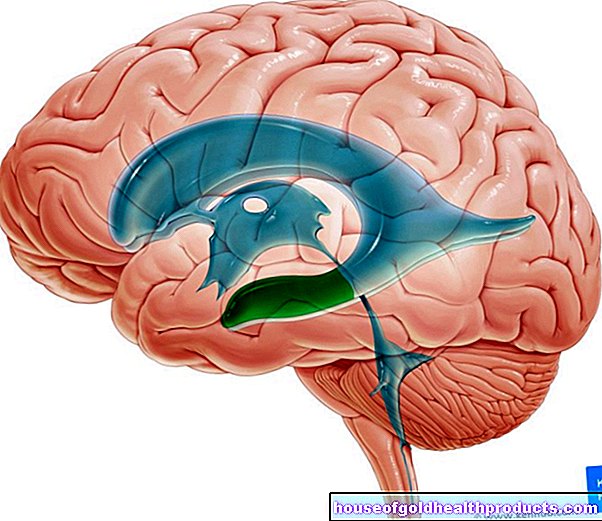
Many transplants are allogeneic - the patients receive another person's organs. This donor is very often a dead person - in other words, a person who has been found to be brain dead (post-mortem organ donation). Before the surgeons at one of the 49 German transplant centers can carry out such an organ transplant, their patient must be assigned a donor organ. Since the need for donor organs and tissues significantly exceeds availability, the distribution of transplants in Germany is regulated and strictly monitored in the Transplantation Act.
In order for a patient to be assigned an organ, the doctor treating them has to put them on a waiting list, which assigns them a certain rank based on urgency and the likelihood of success. In Europe, several organizations mediate post-mortem donations, such as Eurotransplant, which is also responsible for Germany.
A post-mortem organ donation is subject to conditions: there must be express consent to the organ donation - either the deceased has given his consent while he was still alive (e.g. through an organ donation card) or the relatives consented to an organ donation after the patient's death. In addition, two doctors (specially trained intensive care physicians) must independently determine the patient's brain death before organ removal.
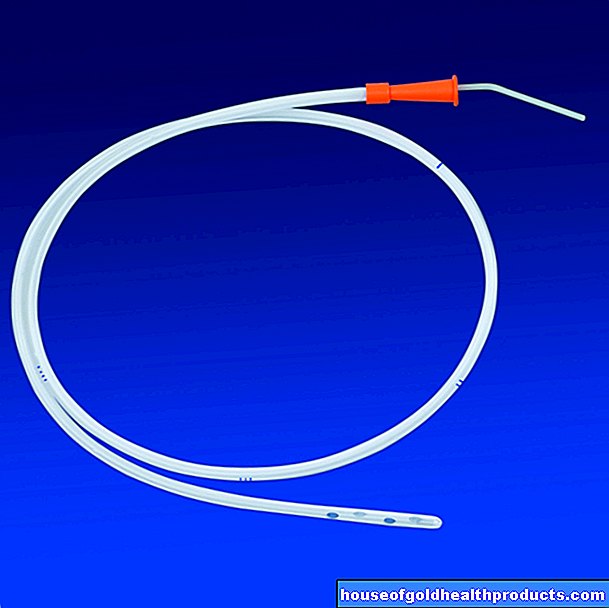
If these requirements are met, the doctors remove the donor organ (explantation). In order to prevent damage to the organ that is no longer supplied with blood, it is stored in a cool box and transported as quickly as possible to the transplant center, where the recipient is already prepared for the procedure.
Living donation
Living donations are only possible from close relatives (e.g. spouse, adult children / siblings or parents / grandparents) or other persons close to the donor. Organ transplants against payment are not permitted. Even the attempt to trade in organs is a criminal offense.
Further information: skin grafting
When to perform a skin transplant and what you have to consider in the article Skin transplantation.
Further information: heart transplant
When to perform a heart transplant and what you have to consider in the article Heart Transplant.
Further information: Corneal transplant
When to perform a corneal transplant and what you have to consider in the article Corneal Transplant.
Further information: liver transplant
When to carry out a liver transplant and what to consider when doing it, read the article on liver transplantation.
Further information: lung transplant
When to perform a lung transplant and what you have to pay attention to, read the article Lung Transplantation.
Further information: kidney transplant
When to perform a kidney transplant and what you have to consider in the article kidney transplant.
What are the risks of a transplant?
Depending on the type and extent of the operation, a transplant can involve considerable risks. For example, there is a high risk of bleeding or rebleeding, as the surgeons also separate large blood vessels during the transplant and sew them together again. The risk of infections is also increased.
The greatest danger is rejection of the donor organ. The recipient's immune system recognizes that the cells of the transplant do not come from their own body and therefore actively counteracts them. Such rejection is referred to as hyperacute (a few hours), acute (days to weeks) or chronic (months to years) depending on the time it takes for the reaction to begin. To prevent transplant rejection, the patient is given drugs that suppress the immune system from the start. These immunosuppressants can have severe side effects, but are necessary. However, they do not guarantee that the body will not reject the foreign organ after all. It must then be removed again.
Many patients also suffer from psychological problems after a transplant - such as feelings of guilt towards the dead donor or towards patients who continue to wait for an organ.
What do I have to consider after a transplant?
So that any complications after an organ transplant can be discovered quickly, you must attend regular follow-up appointments. The doctor will discuss with you how you should behave in everyday life after the operation, which medication you need and which side effects may occur after the transplant.
Tags: smoking alternative medicine travel medicine

















.jpg)