Shock position (shock position)
Carola Felchner is a freelance writer in the medical department and a certified training and nutrition advisor. She worked for various specialist magazines and online portals before becoming a freelance journalist in 2015. Before starting her internship, she studied translation and interpreting in Kempten and Munich.
More about the experts All content is checked by medical journalists.In shock positioning (shock position), the patient lies flat on their back while their legs are raised or positioned above head height. In this position, the blood flow back from the legs to the internal organs (especially the heart and brain) is supported. Read here in which cases shock positioning makes sense and when it should not be carried out under any circumstances.

Brief overview
- What does shock positioning mean? In the shock position, the first aider positions the legs of the person lying flat on their back higher than their head. This is to prevent him from becoming unconscious or from collapsing his cycle.
- This is how shock positioning works: Lay the person affected flat on their back on the floor, their legs about 20 to 30 degrees higher than the upper body / head on a solid object (e.g. stool) or hold up.
- In what cases? With different types of shock.
- Risks: None, provided that the shock position is not used in situations in which it is not recommended (see under "Caution!"), When the shock position is used in the wrong cases, e.g. in the case of a heart attack (the shock position puts additional strain on the heart), bleeding wounds Upper body (shock position increases blood flow to the wound area) or in the case of spinal injuries (moving the patient can worsen the injury).
Caution!
- No shock positioning in the event of a shock that originates in the heart (cardiogenic shock, e.g. in the case of a heart attack) - the shock position would put additional strain on the heart!
- No shock positioning in the case of severe hypothermia, shortness of breath, broken bones, chest and stomach injuries as well as injuries to the head and spine!
How does the shock positioning work?
The shock position (shock position) is used in first aid to stabilize the patient's circulation until the emergency services arrive. It is used when the person concerned is still conscious.
How to proceed with shock positioning:
- Lay the victim flat on the floor, supine.
- Position your legs about 20 to 30 degrees or about 30 centimeters higher than your torso / head. You can either hold them or place them on a box, step, etc. This improves the blood flow to the brain and other organs.
- Keep the victim warm, for example with a jacket or (rescue) blanket.
- Talk to the person lying down soothingly and avoid further agitation for him.
- Check the patient's breathing and pulse regularly until the emergency services arrive.
- Try to stop any bleeding (e.g. with a pressure bandage).
What is a shock?
"I'm shocked," is easy to say. However, this condition has little to do with shock in the medical sense. In the event of shock, the body switches to an emergency program. It pulls the blood volume together in the middle of the body in order to continue to supply the internal organs and the brain. However, this sensible reaction can set in motion a fatal spiral of shock, which can lead to the failure of several vital organs such as the kidneys, liver and lungs (multiple organ failure).
Medical professionals differentiate between different types of shock, including:
- Hypovolemic shock (triggered by a lack of volume, i.e. severe fluid / blood loss)
- Cardiogenic shock (triggered by insufficient heart pumping, e.g. in the event of a heart attack, myocarditis or pulmonary embolism)
- Anaphylactic shock (severe allergic reaction)
- Septic shock (in the context of blood poisoning = sepsis)
- Neurogenic shock (if the nerve-related blood pressure regulation fails, e.g. in the event of spinal cord injuries)
A shock can be recognized by symptoms such as pale skin, freezing, tremors, cold sweat as well as restlessness and fear.
When do I do a shock positioning?
A shock positioning is made when the person concerned is still conscious and breathing independently. It can generally be considered in the following cases:
- Volume-depleted shock (unless it was caused by severe bleeding from the upper body)
- anaphylactic (allergic) shock
- septic shock
- "Tipping over", i.e. brief loss of consciousness (fainting) due to a temporary lack of oxygen in the brain, for example when standing for a long time or when startled (vasovagal syncope)
When do I not do shock positioning?
Do not use shock positioning for:
- cardiogenic shock and heart disease in general
- Shortness of breath
- Head and spine injuries
- Chest and stomach injuries
- Broken bones
- severe hypothermia
Risks in shock positioning
There is not much you can do wrong with the shock position itself as a first aid provider - unless you use it in cases where the shock position is discouraged. For example, elevating the legs of a patient who is bleeding from the head, chest, or abdomen can increase the bleeding.
When putting a patient with a spinal injury into the shock position, moving may make the injury worse.
If someone is severely hypothermic, the well-intentioned shock positioning can lead to a lot of cold blood flowing back into the center of the body. This can increase hypothermia.
The shock position can also be very dangerous for patients with a shock emanating from the heart (cardiogenic shock) - the increased blood backflow caused by raising the legs puts additional strain on the pumping weak heart.
Tags: organ systems womenshealth sleep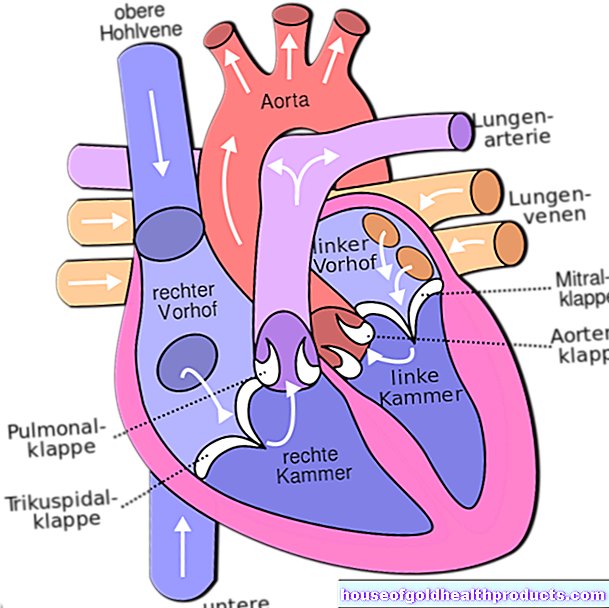











-warten-auf-den-piks-der-freiheit.jpg)