Angina pectoris
and Carola Felchner, science journalistDr. med. Mira Seidel is a freelance writer for the medical team.
More about the expertsCarola Felchner is a freelance writer in the medical department and a certified training and nutrition advisor. She worked for various specialist magazines and online portals before becoming a freelance journalist in 2015. Before starting her internship, she studied translation and interpreting in Kempten and Munich.
More about the experts All content is checked by medical journalists.Angina pectoris (medical stenocardia) means chest tightness. It manifests itself as a sudden pain in the heart area and a feeling of pressure in the chest. Angina pectoris is triggered by a lack of oxygen in the heart. There is danger to life, so you should call the emergency doctor immediately! Angina pectoris can usually be treated well with medication. Find out here, among other things, how symptoms differ between men and women and what you can do to avoid angina pectoris.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. I20I25

Brief overview
- What is angina? Sudden, painful chest tightness
- Symptoms: pain behind the sternum that may radiate, including also shortness of breath, nausea, tightness in the throat, numbness and anxiety, in women / elderly people: tiredness, shortness of breath
- Causes: insufficient supply of oxygen-rich blood to the heart (mostly due to coronary heart disease, CHD)
- Risk factors: smoking, high blood pressure, diabetes mellitus, old age
- Treatment: medication (especially nitro preparations); possibly surgery
- Prognosis: Angina pectoris can be severe up to and including fatal heart attack. Therefore, it is imperative to treat it. General measures such as exercise and a healthy diet are also important to reduce the risk of a seizure.
Angina: symptoms & warning signs
With angina pectoris (chest tightness, tightness of the heart, stenocardia) doctors describe an attack-like pain behind the breastbone. It is usually the main symptom of hardening of the arteries (arteriosclerosis) of the coronary arteries (coronary heart disease = CHD). Angina pectoris is actually a symptom and not a disease.
Depending on the course, doctors differentiate between stable and unstable angina pectoris.
General angina symptoms
Angina pectoris usually manifests itself with sudden pain and a feeling of tightness, burning, pressure or tightness behind the breastbone. The pain often radiates to other parts of the body, such as the neck, throat, lower jaw, teeth, arms or upper abdomen. In addition, there may be pain between the shoulder blades.
Those affected often describe a feeling of heaviness and numbness in the arm, shoulder, elbow or hand. This usually affects the left side of the body. In addition, symptoms such as sudden shortness of breath, nausea, vomiting, sweating and an oppressive, choking feeling in the throat can occur. These signs are often accompanied by feelings of fear up to fear of death and fear of suffocation.
Special features in women
In women, angina pectoris usually manifests itself with different symptoms than in men: Symptoms such as tiredness, shortness of breath and stomach problems are the typical signs here. The classic chest pain, on the other hand, only occurs in a few women.
Particularities in the elderly
Elderly patients (especially those over the age of 75) often show angina symptoms similar to women. When they have an attack, they often only complain of shortness of breath and a drop in performance.
Particularities in diabetes
Angina pectoris in diabetes (diabetes) has a special feature: patients with diabetes-related nerve damage (diabetic polyneuropathy) often feel no pain because pain stimuli can no longer be completely transmitted from the damaged nerves. Angina pectoris can therefore be almost painless (silent) in diabetics or be accompanied by only slight pain.
Stable angina: symptoms
In stable angina pectoris, the angina pectoris attacks are relatively similar each time. The signs of chest tightness are triggered by some form of stress. This can be physical or emotional stress, cold or a large meal. The pain can spread to the neck, lower jaw, teeth, shoulders and arms. The symptoms usually go away within 15 to 20 minutes at rest. If you use a nitro spray against the signs of angina pectoris, they subside after about five minutes.
According to the Canadian Cardiovascular Society, stable angina pectoris is divided into five stages:
|
stage |
complaints |
|
0 |
No symptoms. |
|
I. |
No complaints with everyday stress, but with sudden or prolonged stress. |
|
II |
Discomfort with increased exertion. Normal physical exertion is little restricted. |
|
III |
Discomfort with lighter physical exertion. |
|
IV |
Resting discomfort and discomfort with the slightest physical exertion.
|
Unstable angina: symptoms
Unstable angina pectoris is the term used to describe various forms of chest tightness with inconsistent symptoms. For example, the seizures can get stronger from time to time or last longer. Or they also occur at rest or even with low stress. Rest or previously effective medication (such as nitrospray) hardly help against the symptoms.
A special form of unstable angina pectoris is the rare Prinzmetal angina. This is where the heart vessels cramp (medical coronary vascular spasm). It occurs at rest, for example in sleep.
Unstable angina pectoris can develop from a stable chest tightness or come out of nowhere.
The unstable angina pectoris is divided into three degrees of severity:
|
Great |
Severity |
|
I. |
New onset of severe or worsening angina pectoris |
|
II |
Angina pectoris at rest within the last month but not within the last 48 hours |
|
III |
Angina at rest within the last 48 hours |
With unstable angina pectoris there is a high risk of a heart attack (20 percent). Therefore, in the event of an attack, the emergency doctor must be called immediately! Incidentally, Meiziner speak of acute coronary syndrome when unstable angina pectoris turns into a heart attack.
Angina pectoris: causes and risk factors
Angina pectoris occurs when the heart muscle is not supplied with enough blood in an attack. The cause is usually a narrowing of the vessels as a result of hardening of the arteries (arteriosclerosis) of the coronary arteries. More rarely, an angina pectoris attack is triggered by cramping of the vessels (vasospasms), such as Prinzmetal's angina.
In atherosclerosis - the main cause of angina pectoris - the blood vessels are narrowed by deposited fats, blood platelets, connective tissue and calcium. If the blood vessels supplying the heart (coronary arteries) are affected, the heart does not receive enough oxygen and nutrients. Doctors then speak of coronary heart disease (CHD) with the main symptom angina pectoris.
Risk factors such as smoking, high blood pressure, diabetes mellitus (diabetes) and old age favor the deposition of blood lipids on the arterial walls. Inflammatory processes transform the wall of the blood vessel - an arteriosclerotic (atherosclerotic) plaque is formed. Over many years the vessels harden and their diameter becomes smaller and smaller. If such plaque tears in the coronary arteries, blood clots form on site, which can completely block the artery.
If the heart muscle area supplied by this artery is no longer supplied with blood and dies, it is called a heart attack.
Angina pectoris in coronary heart disease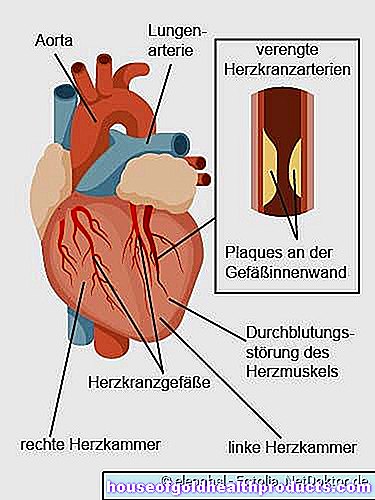
The following factors increase the risk of coronary artery hardening (CHD):
- Diet: High-fat and high-calorie foods lead to overweight and high cholesterol levels in the long run.
- Obesity
- Sedentary lifestyle
- Male sex: Men are at higher risk of arteriosclerosis than women before the menopause. The latter are protected by the female sex hormones (especially estrogen). After the menopause, when estrogen production stops, this protective effect is lost.
- Genetic predisposition: In some families, cardiovascular diseases such as CHD occur more frequently, so genes seem to play a role. The risk is increased if first-degree relatives are diagnosed with CAD before the age of 55 (women) or 65 (men).
- Smoking: Substances in tobacco smoke promote, among other things, the formation of unstable plaques in the blood vessels.
- High blood pressure: Increased blood pressure values directly damage the inner walls of the blood vessels.
- Elevated cholesterol: High LDL cholesterol and low HDL cholesterol encourage plaque buildup.
- Diabetes mellitus: If the diabetes is poorly controlled, the blood sugar is permanently too high, which damages the blood vessels.
- Increased inflammation values: e.g. an increased CRP value in the blood (makes the plaques unstable).
- older age: with increasing age, the risk of hardening of the arteries in the coronary arteries increases,
Angina pectoris: treatment
The primary goal of angina pectoris treatment is to prevent severe seizures and a heart attack. The risk of infarction exists especially with unstable angina pectoris. This can be recognized, for example, by the sudden pain and tightness in the chest or the usual angina pectoris symptoms are unusually severe.
If angina pectoris is unstable, call the emergency doctor immediately! The patient has to go to the hospital as soon as possible because there is a high risk of heart attack.
You should provide first aid until the emergency doctor arrives: Loosen any items of clothing that restrict the patient (e.g. collar, belt). Raise the upper body and try to calm the patient down. When the whole thing happens in a room, you can open the window and let in fresh air. Many of those affected find this beneficial.
Angina pectoris: medication
An acute attack of angina pectoris is usually treated with nitro preparations such as nitroglycerin as a spray or capsule to bite into. Nitro supplements expand the coronary arteries. This relieves the heart and reduces oxygen consumption. As the blood vessels widen in the rest of the body as well, the blood pressure drops.
Under no circumstances should nitro preparations be taken together with sexual enhancers (phosphodiesterase 5 inhibitors), as they also lower blood pressure. The blood pressure can then drop to a life-threatening level.
Other drugs that are used in angina pectoris therapy (also long-term) are, for example, active ingredients that keep the blood thin (platelet aggregation inhibitors such as acetylsalicylic acid or clopidogrel). So-called beta blockers are also often prescribed to patients. They lower the heart rate and blood pressure during exercise. This can prevent angina attacks. Regular use of vasodilators (vasodilators) such as various nitrates is also helpful. The doctor can prescribe statins for high cholesterol levels.
Angina pectoris: interventions on the heart
The narrowed section of the vessel that causes angina pectoris can be expanded using balloon dilatation: a small balloon is inserted into the narrowed point in the vessel through a thin plastic tube (catheter). The balloon is inflated on site so that it expands the constriction.
Another option for treating angina is bypass surgery. The surgeon bridges the narrowed piece of vessel with a piece of the body's own or artificial artery to restore the blood supply.
Angina pectoris: healthy lifestyle
Successful angina pectoris treatment also includes the cooperation of the patient: those affected should adopt a lifestyle that avoids or at least reduces the risk factors of chest tightness. This can be achieved, for example, with a healthy diet, regular exercise and avoiding nicotine. Overweight patients should also try to lose weight. The attending physician can advise and support patients in changing their lifestyle.
Angina pectoris: examinations and diagnosis
If anging a pectoris is suspected, the doctor has various “tools” at his disposal to make and confirm a diagnosis.
Conversation and physical examination
First, the doctor will collect the patient's medical history (anamnesis) in conversation with the patient. He asks, for example, how long have the symptoms of a heart constriction existed, how exactly they express themselves, or whether they are triggered by anything (such as physical exertion). In addition, the doctor asks whether the symptoms can be relieved with a nitro spray.
The information from the anamnesis interview helps the doctor assess whether the chest pain is caused by coronary artery disease (CHD), another disease. For example, the symptoms can also originate from the stomach. In addition, a pulmonary embolism (i.e. the closure of a lung vessel by a blood clot that has washed up) can trigger symptoms similar to angina pectoris.
The next step is a physical exam. Among other things, the doctor will listen to the heart and tap the chest. A blood pressure measurement is also part of this examination. The doctor uses this to check whether the patient has high blood pressure (hypertension).
Imaging procedures
Various imaging methods help, among other things, to check the heart function and the blood supply to the heart muscle:
Ultrasound of the heart: With heart ultrasound (echocardiography), the doctor uses ultrasound to examine whether the heart muscle has changed. In this way, he can assess the ventricles and heart valves and their function.
Resting and long-term ECG: An electrocardiogram (ECG) shows the electrical activities of all heart muscle fibers as a sum in a cardiac tension curve. The ECG is changed in over half of patients with angina pectoris. If the doctor suspects cardiac arrhythmia, a long-term ECG is performed.
Exercise tests for the heart: Usually an exercise ECG with bicycle ergometry is also done in the clinic or practice. The patient rides a stationary bicycle while the load is gradually increased. At the same time, the ECG and blood pressure values are measured. The aim of an exercise ECG is to achieve insufficient blood flow to the heart muscle. If angina pectoris occurs as a result and the ECG changes, one speaks of positive ergometry.
Stress magnetic resonance imaging: Another examination option is stress magnetic resonance imaging (stress MRI). The heart is artificially stressed by drugs such as dobutamine and adenosine (these drugs make the heart beat faster and stronger). The doctor provokes an oxygen deficiency in the heart and examines this or its consequences in an MRI.
Heart scintigraphy: The heart or myocardial scintigraphy can show the blood flow to the heart muscle. To do this, the patient is first injected with a weakly radioactive substance. It is distributed in the heart muscle according to the blood flow and is absorbed by the cells. The radioactive rays emitted by the substance are captured by a so-called gamma camera and displayed as an image. The picture shows which areas of the heart muscle are being supplied with less blood. The recordings with the gamma camera are taken once at rest and once under stress. Myocardial scintigraphy is used when the ECG and echocardiography are insufficient to make a diagnosis of angina pectoris.
Angina pectoris: course and prognosis
The chest tightness is usually a sign of arteriosclerotic constriction of the coronary arteries (coronary heart disease, CHD) and therefore a warning signal. A hardening of the arteries develops slowly over the years.Above a certain level, it can trigger angina pectoris even with low stress. This can limit the quality of life and performance of the person concerned. The stronger and more frequent the angina attacks, the higher the risk of a heart attack.
It is therefore important to treat angina pectoris as early as possible. This not only includes the doctor prescribing the right medication or performing a surgical procedure (balloon dilatation, bypass surgery). Each patient can positively influence the course of angina pectoris, for example by giving up smoking, eating a healthy diet and regular physical activity.
Angina pectoris: prevention
If you want to prevent angina pectoris, the same tips apply as for people who already suffer from chest tightness: A healthy lifestyle can make a significant contribution to keeping the heart and blood vessels healthy. This includes eating healthy, exercising regularly and losing weight if you are overweight. This lowers the risk of coronary heart disease (CHD), the most common cause of angina pectoris. It is also very important not to use nicotine if you want to reduce your personal risk of angina pectoris. Smoking narrows the blood vessels and thus impairs the blood flow to the heart muscle (and other parts of the body).
Also, go to regular checkups. In this way, diseases such as diabetes, high blood pressure or high blood cholesterol levels, which damage the blood vessels, can be detected and treated in good time. If the doctor prescribes appropriate medication for you, you should take them regularly - even if you are feeling well at the moment.
Another tip: Avoid stress and allow yourself regular relaxation in everyday life. This also helps to prevent angina pectoris.
Additional information
Guidelines:
- Guideline "Coronary Heart Disease / Angina pectoris" of the German Society for Cardiology - Heart and Circulatory Research
Self help:
- German Heart Foundation: https://www.herzstiftung.de/Angina-pectoris.html





.jpg)

-der-giraffentrick.jpg)