arthrosis
Ricarda Schwarz studied medicine in Würzburg, where she also completed her doctorate. After a wide range of tasks in practical medical training (PJ) in Flensburg, Hamburg and New Zealand, she is now working in neuroradiology and radiology at the Tübingen University Hospital.
More about the experts All content is checked by medical journalists.Osteoarthritis is a painful joint disease. It occurs when the joint cartilage is irreparably damaged. With conservative therapies or an operation, the symptoms of joint wear can be significantly reduced. Read more on the topic: What is osteoarthritis? What kind of complaints do you have? What can be done against osteoarthritis?
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. M15M16M19M47M23M17M12M24M96
Osteoarthritis: Brief overview
- Joints most commonly affected: knees, hips, shoulders, spine, finger and toe joints, ankles
- Most important signs: pain during exertion, start-up pain (pain at the beginning of physical activity), reduced mobility, joint thickening, with activated osteoarthritis: overheating, reddening, constant pain
- Diagnostics: physical examination, x-rays, computed tomography (CT) or magnetic resonance imaging (MRI)
- Treatment: exercise, warm or cold packs, pain relievers, possibly joint injections (hyaluronic acid, chondroitin sulfate), in advanced stages: joint replacement (surgery)
- Attention: Many arthroses do not have to be operated on for a long time, but improve sufficiently through exercise / physiotherapy and, if necessary, pain therapy
Osteoarthritis: treatment
What helps with osteoarthritis? For most patients, that is the central question. The clear answer: So far, there is no osteoarthritis treatment that can restore damaged cartilage. The osteoarthritis treatment can only alleviate the symptoms of the disease. In addition, it should prevent joint wear and tear from progressing further. Because over time, the disease also leaves its traces in the vicinity of the worn joint: Damage occurs in the joint capsule, on the bones and on the muscles.
In principle, osteoarthritis treatment includes conservative and surgical procedures. The attending physician will select the most suitable methods for each patient. Among other things, he takes into account which joint is affected, how pronounced the joint wear is and how severe the symptoms are.
Osteoarthritis: Conservative Treatment
Conservative osteoarthritis treatment is intended to relieve pain, combat inflammation and strengthen muscle strength and coordination. Stiff joints should be more flexible again and incorrect loads should be compensated for.
Move joints
Regular exercise keeps the joints flexible. Therefore, people with osteoarthritis should incorporate exercise into their everyday life, for example swimming. The crawl and backstroke are particularly suitable. You train your joints without putting too much strain on them. For the same reason, hiking on the plains and cycling are recommended for people with osteoarthritis.
Sports with abrupt, high joint loads, extreme movements or a high risk of injury are less suitable for osteoarthritis. These include, for example, tennis, ice skating, soccer, handball, karate and boxing.
Relieve joints
Bandages, elastic bandages, soft shoe soles and crutches relieve the joints. Orthoses also help in a similar way. These are special positioning rails for joints. They prevent painful movements. However, orthoses are not very mobile and should only be worn for a short time so that the joint does not stiffen.
If you are overweight, you should try to lose some weight. Your joints will have to carry less weight. Regular exercise and a healthy diet will help you lose weight.
Physical osteoarthritis therapy
Chronic osteoarthritis pain can be treated with heat from heating pads, mud packs, fango, baths or infrared light. Acute swellings and complaints, on the other hand, are relieved with cold ice packs or cool moor packs.
Physiotherapy is also helpful as a physical osteoarthritis treatment because it strengthens the muscles. Massages are also recommended: they relieve tension and improve blood circulation.
Medicines for pain and inflammation
Aching osteoarthritis joints can be rubbed in with pain relieving ointments, creams or gels from the pharmacy.
Paracetamol is often recommended as a pain reliever in osteoarthritis. Local anesthetics are also used to relieve pain: They are injected into or around the affected joint.
Osteoarthritis is usually a non-inflammatory joint disease. However, an inflammatory process can "sit on top". Then one speaks of osteoarthritis arthritis or activated osteoarthritis. The doctor often prescribes non-steroidal anti-inflammatory drugs (NSAIDs) such as acetylsalicylic acid or ibuprofen for treatment. Sometimes glucocorticoids are injected into the joint against the inflammation, so called "cortisone".
Some patients get hyaluronic acid for osteoarthritis. This is a so-called glycosaminoglycan and a natural component of the synovial fluid. With hyaluronic acid injections directly into the affected joint, you want to make it more flexible again. However, the effectiveness has not been clearly proven. In addition, with such syringes there is a risk that germs can inadvertently be introduced into the joint. These can infect the joint. Osteoarthritis treatment with hyaluronic acid injections should therefore not be carried out lightly.
Another glycosaminoglycan is the so-called chondroitin sulfate. It is also occasionally given as an injection in the treatment of osteoarthritis. However, its effectiveness has not been proven either. The same applies to the glucosamine that is also used. It is a component of hyaluronic acid and chondroitin sulfate.
Surgical osteoarthritis treatment
An operation can correct malpositions in osteoarthritis patients and stabilize joints. It is also used to relieve pain and prevent inflammation. In some cases, the damaged cartilage can also be replaced as part of the operation. Overall, osteoarthritis patients should be able to move better and be more productive after the operation.
There are different surgical procedures for osteoarthritis. Which one is used in the individual case depends on several factors. For example, what kind of joint is involved and how much wear and tear on the joint is. The age, general condition of the patient and the treatment goal are also taken into account when selecting the surgical method.
Lavage and debridement
In the case of osteoarthritis, the affected joint is sometimes rinsed with a saline solution (lavage). This is done more often, for example, with the knee joint. The irrigation removes cartilage and tissue fibers and other particles floating in the synovial fluid. In addition, it should calm any inflammation that may exist in the joint.
Debridement is a type of articulated toilet. Rough cartilage surfaces in the osteoarthritis joint are smoothed with suitable instruments. Other parts are also removed that may hinder the mobility of the joint. This can be, for example, free joint bodies, cartilage or bone parts. In addition, the debridement should at least temporarily reduce acute pain.
Lavage and debridement are usually performed as part of an arthroscopy. The surgical instruments are inserted into the joint through only small incisions in the tissue.
Cartilage-improving osteoarthritis treatment
The remaining cartilage surface can also be drilled during an arthroscopy. This is supposed to stimulate the cartilage cells to form replacement tissue. However, this new cartilage tissue has a different structure than the original cartilage and does not meet the demands on the joint quite as well.
For some years now, it has also been possible in certain cases to transplant corpus cells from the outside into the damaged joint.
Corrective Osteotomy
In a corrective osteotomy (adjustment osteotomy), the joint-forming bones are positioned differently in order to distribute the load more evenly on the joint surfaces: Part of the load is shifted from the osteoarthritis zone to healthy areas of cartilage and bone. In this form of osteoarthritis treatment, the joint capsule and ligaments are usually operated on in order to improve the mobility of the joint.
A corrective osteotomy is not always used to treat existing osteoarthritis. In the case of misalignments, it can also be carried out preventively in order to prevent the development of joint wear. Misalignments can in fact promote osteoarthritis.
Endoprosthetic joint replacement
If no other osteoarthritis treatment can relieve the pain, an endoprosthetic joint replacement is an option. That means: The damaged joint is replaced by an artificial joint. This is mainly done with osteoarthritis in the knee or hip joint.
Strictly speaking, the worn joint bodies and joint surfaces are surgically removed and replaced with prostheses made of metal, plastic and ceramic (alloarthroplasty). There are prostheses that only replace the joint body and those for the entire joint. They can be anchored into the existing bone with either cement or screws. With this form of osteoarthritis treatment, the joint position can also be corrected if necessary.
Any prosthesis can loosen after a while. When this happens depends on a number of factors. These include age, gender, clinical picture, infections, type of joint and type of prosthesis. A loosened prosthesis often needs to be replaced. Any loosening can be detected in good time with the help of regular x-rays.
Arthrodesis
What is known as arthrodesis can also be used to treat osteoarthritis pain. This is understood to mean surgical joint stiffening: the affected joint is more stable and usable after the procedure, but it is also less mobile. Arthrodesis is therefore usually only carried out on joints in which less mobility does not interfere with the patient's everyday life. These are, for example, finger end joints, other finger joints and small joints in the area of the wrist. Arthrodesis is also sometimes performed on the metatarsophalangeal joint of the big toe.
Resection arthroplasty
In this form of osteoarthritis treatment, the damaged joint bodies are removed and reshaped surgically without a prosthesis. Resection arthroplasty is rarely used today. It is particularly suitable for osteoarthritis of the thumb (rhizarthrosis) if conservative osteoarthritis treatment is unsuccessful. One of the affected metacarpal bones is removed and replaced with the body's own tendon tissue. The tendons of the long thumb muscle or the short hand flexor are often used. However, this form of rhizarthrosis therapy is not considered a standard method.
Resection arthroplasty is sometimes also performed in the case of osteoarthritis of the metatarsophalangeal joint of the big toe (Hallux rigidus) or osteoarthritis between the collarbone and the roof of the shoulder.
Alternative osteoarthritis treatment
What helps with osteoarthritis apart from conventional medical procedures? Many patients are interested in this question. You want to support the conventional medical arthrosis treatment with the help of alternative healing methods. Although the effectiveness of many alternative procedures has not been scientifically proven, they are a good help for some patients with osteoarthritis. Homeopathy, plant substances, magnetic field therapy and acupuncture are supposed to alleviate the symptoms of osteoarthritis. Schüßler salts are also often used for osteoarthritis.
Osteoarthritis treatment: Schüßler salts and homeopathy
Osteoarthritis patients often rely on these two alternative methods: Schüßler salts, like homeopathic globules, are said to be able to alleviate osteoarthritis symptoms. In addition, Schüßler salts should also prevent osteoarthritis. Proponents say that both healing methods have no side effects and are therefore suitable for self-treatment of osteoarthritis.
Suitable Schüßler salts for osteoarthritis are:
- No. 1 Calcium fluoratum
- No. 2 Calcium phosphoricum
- No. 8 sodium chloratum
- No. 9 sodium phosphoricum
- No. 11 Silicea
- No. 16 Lithium chloratum
Experts recommend using these minerals in combination as an ointment or cream gel.
If the osteoarthritis treatment is to be supported with homeopathy, various preparations are available. For example, if movement helps relieve osteoarthritis pain, Rhus toxicodendron D12 is recommended. Dulcamara D12 is used when the joint pain is made worse by cold weather. Patients should discuss with an experienced therapist which other homeopathic remedies are indicated for osteoarthritis.
Osteoarthritis treatment: plant substances
For centuries, osteoarthritis treatment has also been based on medicinal plants. These include, for example, African devil's claw, nettle, comfrey, willow, dandelion, cayenne pepper and rose hip. Osteoarthritis symptoms usually only improve if the medicinal plants are used over a long period of time. Your doctor or pharmacist will advise you on the exact application and dosage.
Osteoarthritis treatment: magnetic therapy
Osteoarthritis treatment using magnetic field therapy is intended to relieve pain, swell the joints and increase the patient's wellbeing. The magnetic field is generated either by a natural magnetic stone or by an electric coil.
Medical studies have shown that magnetic field therapy can be particularly helpful for osteoarthritis of the knee. But also patients with chronic complaints in several joints (polyarthritis) should benefit from it. Side effects were not observed with this alternative osteoarthritis treatment.
Osteoarthritis treatment: X-ray pain irradiation
X-ray osteoarthritis treatment is said to inhibit inflammatory processes and improve blood circulation. The irradiation must be repeated at certain time intervals in order to be effective. Only very low doses of radiation are used.
X-ray pain radiation is used, for example, in rhizarthrosis therapy and Heberden arthrosis therapy. Both are forms of joint wear in finger joints.
Osteoarthritis treatment: acupuncture
The stimulation of certain points on the skin with acupuncture needles is supposed to normalize disturbed processes in the body again. Several sessions are usually necessary for this.
The use of acupuncture for osteoarthritis is not widely recognized. However, some patients report that acupuncture was actually able to relieve their osteoarthritis pain. Acupuncture can reduce chronic pain, especially if the knee is worn out.
-
Osteoarthritis - movement keeps the cartilage healthy
Three questions for
PD Dr. habil. Johannes Schauwecker,
Specialist in orthopedics and trauma surgery -
1
What Helps Cartilage Stay Healthy
PD Dr. habil. Johannes Schauwecker
The most important thing for joint cartilage health is exercise. Because there are no blood vessels in the cartilage tissue. Nutrients are therefore only absorbed from the synovial fluid, and exercise is necessary for this. But be careful: If you exercise too intensely, you can achieve exactly the opposite and damage the cartilage due to the high stress. Obesity can also have a negative impact.
-
2
What if the cartilage is already damaged?
PD Dr. habil. Johannes Schauwecker
Non-surgical measures are crucial in the treatment of osteoarthritis, especially in the early stages. Physiotherapy and independent training can improve posture, muscle strength and joint mobility. Bandages and custom-made shoe insoles relieve the joint. Anyone who is overweight should try to lose a few pounds. That can help too.
-
3
When does a joint replacement make sense?
PD Dr. habil. Johannes Schauwecker
Get a second doctor's opinion if your doctor recommends a joint replacement. This is because the patient's quality of life is decisive for an operation, not the degree of joint damage. A joint replacement is only advisable when the person concerned has exhausted all non-surgical treatment options and still complains of severe pain or restrictions in private and work life.
-
PD Dr. habil. Johannes Schauwecker,
Specialist in orthopedics and trauma surgeryAdditional qualification in manual medicine and chiropractic therapy, hip and knee specialist, certified main surgeon for endoprosthetics at the Orthopedic Center Munich East
Osteoarthritis and Diet
The connection between osteoarthritis and diet is often discussed: Can an unfavorable diet promote osteoarthritis? Is it therefore worth changing diet for osteoarthritis?
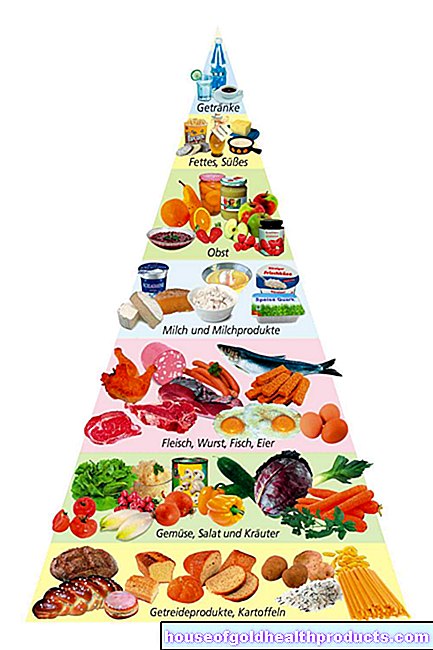
In general, it cannot be said that individual foods cause osteoarthritis. Overall, however, the type of diet can actually influence osteoarthritis: The decisive factor is how much we eat and how our meals are composed.
Less calories
If you gain weight, your joints have to bear more weight. As a result, they wear out faster. Overweight people therefore have a higher risk of osteoarthritis. If you already have osteoarthritis, being overweight promotes joint wear, especially in the knee joint ("osteoarthritis knee").
Diet for osteoarthritis should therefore be reduced in calories if you tend to be overweight or already bring excess kilos on the scales. A healthy body weight relieves the joints, can alleviate the symptoms of the disease and slow its progression.
Less animal foods
The right diet for osteoarthritis is poor in meat and other animal foods. The reason: Joints damaged by osteoarthritis can easily become inflamed. Certain metabolic products in the body mediate these inflammatory reactions. Some are made from the omega-6 fatty acid arachidonic acid. This is mainly found in animal foods.
The diet for osteoarthritis should therefore contain little arachidonic acid. That means: You should reduce the consumption of meat and meat products. Instead, one should increasingly resort to products that contain a lot of omega-3 fatty acids. Because these inhibit inflammatory reactions. Omega-3 fatty acids are found, for example, in rapeseed and linseed oil and in high-fat fish such as herring, mackerel and salmon.
In summary, the following tips apply to a suitable osteoarthritis diet:
- Reduce your consumption of meat and eggs.
- Eat fish (such as salmon, mackerel, herring) twice a week.
- Use vegetable oils such as canola oil, linseed oil, sunflower oil, or olive oil.
- Eat lots of fruits and vegetables.
- Prefer whole grains and legumes.
- Drink at least 1.5 liters of water or unsweetened tea every day.
- Calcium from low-fat dairy products strengthens your bones.
- Avoid caffeine, alcohol, and nicotine.
Such an osteoarthritis diet cannot replace other therapeutic measures, but it can complement them sensibly. This means that although it cannot cure osteoarthritis, it can have a beneficial effect on the disease. However, for an osteoarthritis diet to be successful, it must be permanent. Incidentally, it helps with all forms of osteoarthritis - from knee joint osteoarthritis to finger osteoarthritis (Heberden).
Osteoarthritis: symptoms
In the beginning, joint wear often does not cause any complaints. Over time, however, pain sets in when the affected joint is moved or stressed. In the late stages of osteoarthritis, joint pain can also occur at rest or permanently. Many patients also report noticeable or audible rubbing and cracking noises in the joint.
Arthrosis joints also often feel "stiff" and their mobility is restricted, for example the fingers in the case of arthrosis in the finger joint. In addition, the joint position can change pathologically over time.
Sometimes inflammation is added to the continuous wear and tear of the joint. This can happen in the case of acute overload, for example. Then one speaks of activated osteoarthritis: The affected joint swells and is overheated. The pain will increase and an effusion may form in the joint.
You can read more about the signs of joint wear and tear in the various stages of osteoarthritis in the article Osteoarthritis Symptoms.
Osteoarthritis: causes and risk factors
With osteoarthritis there is increasing wear and tear of articular cartilage. There can be different reasons. In all cases, however, the affected joint is stressed beyond its load-bearing capacity for a longer period of time. This causes cartilage damage. Since the cartilage cannot repair itself, it wears out.
With increasing age, joints wear out in everyone. Other possible causes are:
- Overload: for example, if you are overweight or have an unusually high load on your joints (for example in competitive sports or when working with a jackhammer)
- Incorrect loading: for example, due to joint misalignments such as bow legs or knock knees
- Metabolic diseases such as gout (uric acid crystals build up in joints, causing cartilage damage)
- Injuries: for example cartilage trauma (post-traumatic osteoarthritis) or broken bones that heal in a misalignment
With such clearly demonstrable causes, doctors speak of secondary osteoarthritis. In other cases, however, no cause for the joint wear can be identified. Then there is primary osteoarthritis.
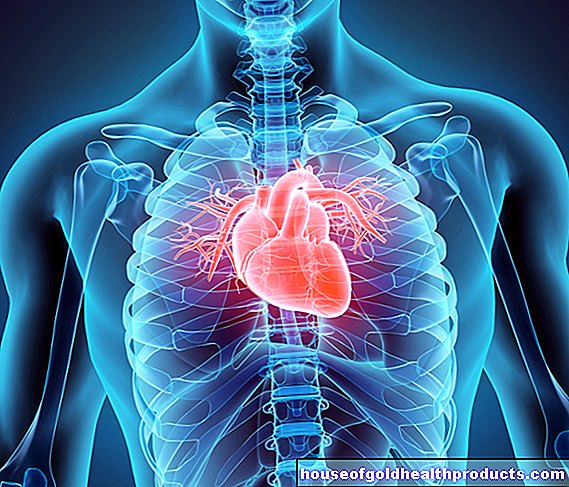
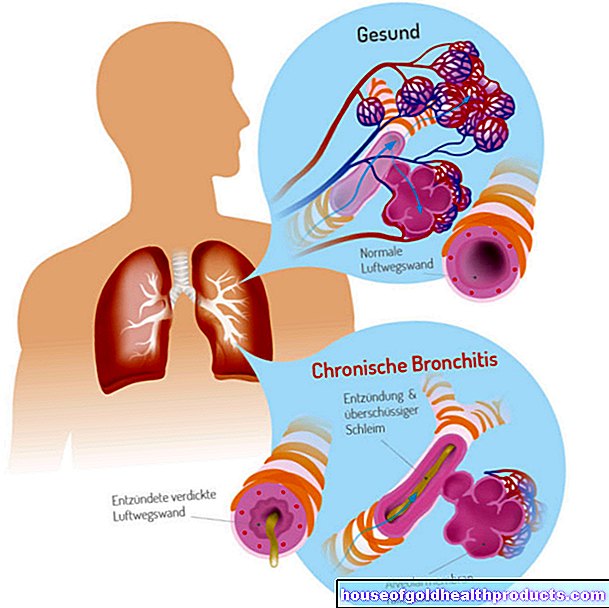
Osteoarthritis development
From cartilage damage to osteoarthritis
Destroyed cartilage usually affects normal joint function. Normally, the individual components of the cartilage are constantly being renewed. However, defective cartilage cells can no longer do this. In addition, the cartilage substance is broken down by attracted enzymes. The cartilage loses its strength and elasticity. The cartilage layer becomes thinner and can easily tear or form cracks under load.
If the joint continues to be stressed too much, other structures in the joint area change pathologically over time: the synovial membrane (synovial membrane), the bones and the ligaments. Only then does one speak of osteoarthritis.
In the most stressful zones, the cartilage layer finally disappears completely. The joint space narrows and the joint bones are exposed. Doctors speak of "bald bones". In order to withstand the unusual stress, the bone tissue thickens. This is called subchondral sclerotherapy.
In addition, bony extensions (osteophytes) form on the edge of the joint. This changes the entire anatomy of the joint (arthrosis deformans).
The damaged cartilage no longer provides a tight demarcation between the joint space and the bone tissue (cancellous bone). This allows synovial fluid to get into the bone structure and form a cavity in the bone (rubble cyst). Cell debris and metabolic products accumulate in the joint. As a result, the synovium becomes inflamed very easily. Joint effusion also often forms. In this way, joint wear and tear that may have been symptom-free up to that point turns into inflammatory (activated) osteoarthritis.
Osteoarthritis stages
Doctors differentiate between different stages of osteoarthritis, depending on the extent of wear and tear:
- Stage 1: The articular cartilage still looks smooth and is relatively healthy, but is thickened and structurally changed. The synovial membrane can be irritated.
- Stage 2: The cartilage surface is uneven and frayed.
- Stage 3: The cartilage layer is thinned, the joint space narrowed. The first changes in the neighboring bone can be seen.
- Stage 4: The cartilage layer is completely missing in places. The bone shows compression (subchondral sclerosis) and expansion (osteophytes).
Osteoarthritis in the knee
In principle, any joint in the body can be affected by osteoarthritis: ankle, elbow or thumb, for example. Even osteoarthritis of the temporomandibular joint and "osteoarthritis toes" are possible. However, joint wear and tear is most common in the lower extremities and spine. Here the joints have to bear a lot of the body weight and therefore wear out more easily.
Joint wear in the knee is the most common form of osteoarthritis. In some cases, such osteoarthritis of the knee has no specific cause (primary osteoarthritis of the knee). On the other hand, secondary osteoarthritis of the knee is caused, for example, by a misalignment of the axis, for example by knock knees or bow legs. Other possible causes include inflammation or previous damage from accidents (such as meniscus injuries).
You can read more about the causes, consequences and treatment of osteoarthritis in the knee in the article Gonarthrosis.
Arthrosis in the hip joint
Wear and tear in the hip joint is called coxarthrosis and is another common form of osteoarthritis. In most cases, the cause is known: deformations or malformations of the hip joint are often the reason why premature wear occurs. Rheumatic diseases, bacterial inflammation of the hip joint and bone fractures in the joint area are also possible triggers of secondary hip joint osteoarthritis.
You can find more information about the causes, diagnosis and treatment of hip osteoarthritis in the article Coxarthrosis.
Osteoarthritis of the small vertebral joints
Wear and tear on the small vertebral joints in the spine is called spondylarthrosis. It occurs in almost everyone at an advanced age. In addition, there are some diseases that promote wear and tear on the vertebral joints. These include obesity and herniated discs. Certain sports and professions also promote wear and tear on the vertebral joints.
If you would like to know more about the causes, symptoms and treatment of this form of osteoarthritis, please read the article Spondylarthrosis.
Finger osteoarthritis
The hand consists of many small bones, each connected by a joint: the eight carpal bones, the five metacarpal bones, the two finger bones of the thumb and the three finger bones of the remaining fingers.
Osteoarthritis in the hand can affect several of these joints, including the various finger joints. The more common forms of finger arthrosis have their own name: Arthrosis in the thumb saddle joint is called rhizarthrosis. If arthrosis affects the finger joints, a distinction is made between Heberden's arthrosis in the end joints and Bouchard's arthrosis in the middle joints.
There is also wear and tear of the joints in the area of the small carpal bones. It occurs mainly between the scaphoid and polygonal bone (trapezium). In this case one speaks of scaphotrapezial or STT arthrosis.
Rhizarthrosis is a very common form of finger osteoarthritis. You can read more about its development and treatment in the article Rhizarthrosis.
Osteoarthritis in the shoulder joint
Wear and tear in the shoulder joint is called omarthrosis. It usually arises as a result of old injuries or illnesses (such as rheumatism). Primary shoulder arthrosis without a known cause is rare.
You can find out more about the causes, symptoms and treatment of osteoarthritis in the shoulder joint in the article Omarthrosis.
Other forms of osteoarthritis
Other common osteoarthritis are:
- Ankle arthrosis: Arthrosis in the ankle can affect the lower (USG arthrosis) or the upper ankle (ankle arthrosis).
- Arthrosis in the toe: Joint wear and tear in the metatarsophalangeal joint of the big toe (hallux rigidus) is often evident.
- Temporomandibular joint osteoarthritis: The temporomandibular joint is the most frequently used joint in the body and can therefore also be overloaded more easily.
- Sacroiliac joint arthrosis (SI joint arthrosis): Wear and tear in the joint between the ilium and sacrum
- Radiocarpal arthrosis: Arthrosis in the wrist
- Cubital arthrosis: osteoarthritis of the elbow
- Polyarthrosis: wear and tear in several joints at the same time
Osteoarthritis: examinations and diagnosis
In the vast majority of cases, an orthopedic specialist is the right contact for people with osteoarthritis. A dentist or orthodontist, on the other hand, can judge temporomandibular joint complaints well.
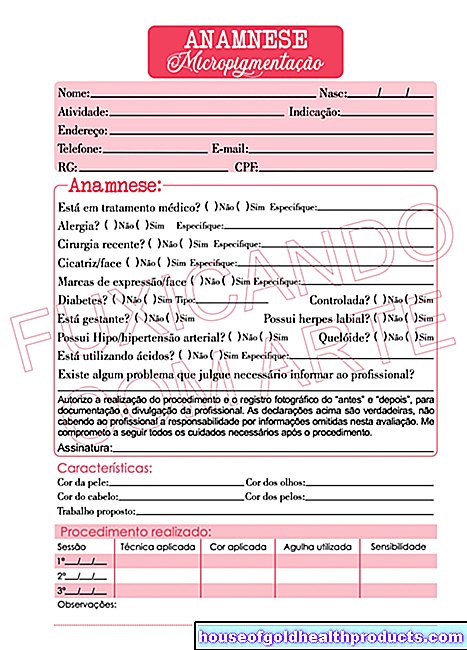
To collect the medical history (anamnesis), the doctor will first talk to the patient in detail. For example, he can ask the following questions:
- Is your joint pre-stressed from an injury or illness?
- Does your pain occur at the beginning of a movement or only after prolonged exertion?
- Does the pain improve with movement or at rest?
- Does the pain recur in certain situations?
Physical examination
The medical history is followed by a physical exam. The doctor assesses the position and function of the affected joint. To do this, he tells the patient how to move his joint. If there are problems with the legs or the spine, for example, he asks the patient to take a few steps. This is the best way for him to judge the sequence of movements.
In addition, the doctor will usually move the affected joint himself and examine the range of motion. It also tests specific pressure points over the joint space, muscles and at the insertion of tendons and ligaments. With pronounced joint wear, he can often feel a fine rubbing or even a coarse crunching of the joint with his hand (crepitation).
Imaging
Even in the early stages of osteoarthritis, one can see in the X-ray that the joint space of the affected joint is narrowing. A compacted bone structure under the articular cartilage (subchondral sclerotherapy) appears whiter on the X-ray. Bony attachments (osteophytes) are usually as bright as the bones themselves. Rubble cysts, on the other hand, leave a dark cavity in the light-colored bone in the X-ray image. In addition, misalignments and changes in the bone structure can be shown in the X-ray image.
Caution: Visible changes in the X-ray image do not allow any conclusions to be drawn as to whether and to what extent someone is suffering from symptoms. Sometimes you can see serious changes on the X-ray, but the patient has no symptoms whatsoever.
On the other hand, early stages can be overlooked in the X-ray image. In unclear cases, computed tomography (CT) or magnetic resonance imaging (MRI) is sometimes performed. These are imaging procedures that are much more accurate than an X-ray examination.
Exclusion of other causes
Joint pain can also have other causes than osteoarthritis. For example, arthritis is another common cause. This inflammatory disease affects the whole body. But it mainly manifests itself as a painful inflammation of the joints.
If osteoarthritis is suspected, the doctor must therefore clarify whether the joint pain is actually due to wear and tear or whether it has another cause (such as arthritis).
Osteoarthritis: disease course and prognosis
The most frequent question from those affected is: "Can osteoarthritis be cured?" The answer: Since the articular cartilage can only regenerate in children, osteoarthritis does not go away. So the disease is not curable. However, effective osteoarthritis treatment can alleviate the symptoms and slow the progression of the disease.
Prevent osteoarthritis
Regular exercise can prevent joint wear and tear. Sports in which the joints are evenly loaded are particularly suitable. This is the case, for example, with cycling and swimming. These sports are also recommended in the treatment of existing joint wear and tear.
In addition, osteoarthritis can be prevented by orthopedically correcting joint misalignments and avoiding over- or under-loading. An important overload arises from being overweight, for example. If you put too much weight on the scales, you should lose weight for the sake of your joints, among other things.
Avoiding unilateral joint loads is also an important preventive measure. This is because these promote joint wear. That is why you should, for example, regularly alternate between sitting and standing activities.
Footwear also has an impact on joint wear: In many women, osteoarthritis affects the metatarsophalangeal joint or other ankles because they very often wear unsuitable footwear. Above all, this includes high-heeled shoes.
Additional information
Book recommendations:
- Cure osteoarthritis yourself: The holistic anti-pain program, Martin Marianowicz, Willibald Walter, 2017, GRÄFE UND UNZER Verlag GmbH; Edition: 3
- Staying in motion despite osteoarthritis: Living without pain again, Peter Krapf, Frank Giarra, 2017, Kneipp Verlag in Verlagsgruppe Styria GmbH & Co. KG; Edition: 1
















.jpg)