Ulcerative colitis
and Carola Felchner, science journalistSophie Matzik is a freelance writer for the medical team.
More about the expertsCarola Felchner is a freelance writer in the medical department and a certified training and nutrition advisor. She worked for various specialist magazines and online portals before becoming a freelance journalist in 2015. Before starting her internship, she studied translation and interpreting in Kempten and Munich.
More about the experts All content is checked by medical journalists.Ulcerative colitis is a chronic inflammation of the large intestine. A typical sign is diarrhea with blood and mucus. There is also pain, often in the left upper abdomen. Ulcerative colitis usually progresses in relapsing form: normal everyday life is possible during the symptom-free period. On the other hand, hospitalization may be necessary during an episode. Read here how you can help yourself with ulcerative colitis, how diet influences the disease and how colon inflammation actually occurs.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. K50K51

Brief overview
- What is ulcerative colitis? A chronic inflammatory bowel disease that affects the rectum and often the colon.
- Symptoms: i.a. bloody slimy diarrhea, cramp-like pelvic pain, colic-like pain in the left lower abdomen, flatulence, loss of performance
- Risks: massive expansion of the intestine (megacolon) with the risk of intestinal perforation and inflammation of the peritoneum (peritonitis); heavy and possibly life-threatening bleeding; Stunted growth in children; increased risk of colon cancer (colon cancer, colon cancer).
- Causes: unknown; A genetic predisposition in combination with various risk factors is probably responsible for the development of the disease.
- Examinations: physical examination, blood tests, stool examination, colonoscopy, ultrasound of the abdomen, possibly other imaging procedures (x-rays, computed tomography, magnetic resonance imaging)
- Treatment: Medication to alleviate the symptoms (5-ASA such as mesalazine, cortisone, etc.), surgery if necessary
- Prognosis: With the right therapy, the symptoms of ulcerative colitis can usually be brought under control. So far, there has only been a chance of recovery if the colon and rectum are removed.
Ulcerative colitis: description
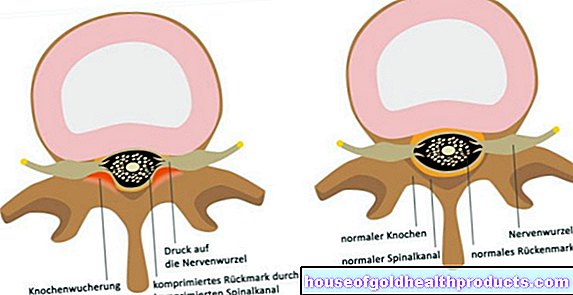
Like Crohn's disease, ulcerative colitis is a chronic inflammatory bowel disease (IBD). It is often difficult to tell the two diseases apart. One big difference, however, is that in ulcerative colitis only the rectum and possibly the large intestine are inflamed, while Crohn's disease can affect the entire digestive tract (from the mouth to the anus).
In addition, ulcerative colitis develops a widespread inflammation that is usually limited to the top layer of the intestinal wall (intestinal mucosa). In contrast, with Crohn's disease, spots of inflammation occur that can affect all layers of the intestinal wall.
Ulcerative colitis mostly occurs in young people between the ages of 16 and 35. In principle, however, the disease can occur at any age.
Inflammatory bowel disease: differences
Expansion of ulcerative colitis
Ulcerative colitis always starts from the rectum. From there it can spread to a greater or lesser extent to the colon:
In many patients, however, the inflammation is limited to the rectum. Then one speaks of a proctitis. If it also extends to the left-sided large intestine, left-sided colitis is present. In some patients, the inflammation extends further up the colon. Finally, if the entire colon (next to the rectum) is inflamed, it is called pancolitis.
As the colitis spreads, the severity of the symptoms also increases.
Ulcerative colitis: different courses
In more than 80 percent of those affected, ulcerative colitis is relapsing: phases with more or less severe symptoms (acute relapses) alternate with phases without inflammation and discomfort. Doctors speak of a chronic, recurrent course.
In around ten percent of patients, the disease takes a chronic, continuous course: the symptoms do not completely subside after a relapse.
In a few cases, ulcerative colitis shows a fulminant course: the disease begins all of a sudden with severe, bloody diarrhea, severe abdominal pain and a high fever. Patients can dehydrate quickly and develop symptoms of shock. About three out of ten people die over time.
Ulcerative colitis: symptoms
Ulcerative colitis often begins insidiously and is only noticed late by those affected. The further the inflammation spreads in the intestines, the worse the symptoms become. An acute ulcerative colitis flare-up can cause such severe symptoms that those affected have to be treated in hospital.
Depending on the severity and course of the disease, symptoms of different strengths (during an episode) occur. This includes:
- bloody slimy diarrhea several times a day and also at night
- painful urge to stool (tenesmen)
- cramping pelvic pain, especially before bowel movements
- Colic abdominal pain, mostly in the left lower abdomen, possibly combined with a slight fever
- nocturnal urge to defecate
- Flatulence, which can lead to involuntary defecation (fecal incontinence)
- Weight loss, fatigue and loss of performance
- Anemia (from bloody diarrhea)
In addition, symptoms outside the intestine can occur (but less often than with Crohn's disease). The most common are inflammations of the joints (arthritis), the spine or the sacrum. Some people develop inflammation around the eyes or bone loss (osteoporosis). Small ulcers, suppurations, or reddish-purple nodules (especially on the front of the lower legs) can form on the skin. In some cases, there is inflammation of the biliary tract inside and outside the liver (primary sclerosing cholangitis).
Ulcerative colitis: complications
A dreaded complication of ulcerative colitis is the so-called toxic megacolon: If the inflammation spreads to the entire intestinal wall, the intestine can acutely expand. The stool can no longer be transported because the intestine is paralyzed (intestinal paralysis, paralytic ileus). It shows the picture of the acute abdomen (acute abdomen): The abdomen is distended, hard and painful. The patients have a high fever.
There is also the risk that the massively enlarged intestine will burst (intestinal rupture, perforation). Then the contents of the intestine (feces) are emptied into the abdominal cavity - an inflammation of the peritoneum (peritonitis) develops. In such cases there is a danger to life!
Another complication of ulcerative colitis can be profuse bleeding: The ulcers of the intestinal mucosa that form as a result of the inflammation can break open and bleed. In severe cases, the blood loss can be so severe that the patient may pass out. The bleeding can even be life-threatening!
Ulcerative colitis in children can cause stunted growth. These can be made worse by poor diet.
People with ulcerative colitis have an increased risk of developing colon cancer (colon cancer).
Ulcerative colitis: treatment
Since the exact causes of ulcerative colitis are not yet known, it has not yet been possible to treat the cause. But there is a lot that can be done to alleviate the symptoms and to lengthen the symptom-free time between the flare-ups. Various drugs are available for this. Additional medication may be necessary in the event of complications (e.g. antibiotics for additional bacterial infections).
Surgery is an option in severe or complicated ulcerative colitis cases. In addition, patients can also help to cope with their illness and alleviate the symptoms themselves. You can read more about the individual building blocks of ulcerative colitis treatment in the following sections.
Ulcerative colitis: drugs
In ulcerative colitis, drugs work best directly at the site of the inflammation in the intestine, for example as a suppository or enema. As a result of this targeted local application of the drugs, side effects are less common than with drugs that are used systemically (such as tablets).
The following drugs are available for ulcerative colitis treatment:
- 5-ASA (5-aminosalicylic acid): has an anti-inflammatory effect and is administered in the form of a precursor, usually as mesalazine. Possible forms of administration include suppositories, enemas, foams (introduced through the anus) and tablets.
- Corticoids ("cortisone"): also have an anti-inflammatory effect (e.g. prednisolone). In milder cases, they are applied locally (e.g. as a suppository or enema), in more severe cases in tablet form.
- Immunosuppressants: active substances that suppress the activity of the immune system (e.g. azathioprine, methotrexate, ciclosporin A, tacrolimus). This can have a positive effect on the course of the disease. They are used for severe or complicated ulcerative colitis (for example, when cortisone does not work or is not tolerated).
- TNF antibodies: active substances that inhibit the inflammatory messenger substance TNF (e.g. adalimumab, golimumab, infliximab). Can be used in more severe cases of ulcerative colitis when cortisone does not work or is not tolerated. TNF inhibitors are among the so-called biologics (biotechnologically manufactured drugs that specifically intervene in certain body processes).
Which drugs are used in individual cases for ulcerative colitis therapy depends on several factors. In addition to the extent of the symptoms, the severity and extent of the inflammation in the intestine play a role. When planning therapy, the doctor also takes into account how well the patient has responded to ulcerative colitis medication and how high his risk of colon cancer is.
Last but not least, a distinction is made between relapse therapy (treatment of a current relapse) and maintenance therapy (to extend symptom-free intervals between relapses; also called maintenance of remission).
Thrust Therapy
In the case of an acute flare-up of ulcerative colitis, the treatment is gradually increased, depending on the severity of the disease.
In mild to moderately severe ulcerative colitis, 5-ASA (more precisely: mesalazine) is usually used. In the case of pure rectal inflammation (proctitis), a mesalazine suppository (or mesalazine rectal foam or enema) is usually sufficient once a day. If that is not enough, patients also receive mesalazine in oral form (tablets, granules) or a locally applicable cortisone (e.g. Budenoside rectal foam).
If the inflammation extends to the large intestine, mesalazine is given both locally (as a foam or enema) and systemically (as a tablet). The dosage depends on the extent of the inflammation in the intestines. If mesalazine does not work well enough or is not tolerated, the doctor prescribes cortisone tablets.
Severe ulcerative colitis is treated with cortisone from the outset (in the hospital as an inpatient). The drug is given in tablet form or through a vein (as an infusion / injection). If the cortisone does not work well enough, the patient is given immunosuppressants or TNF antibodies.
Severe ulcerative colitis is when several criteria are met. These include about six or more severe bloody diarrhea per day, fever, rapid heartbeat (tachycardia) and anemia.
Maintenance therapy
As soon as a disease flare-up is over, patients should continue to use 5-ASA (preferably mesalazine) daily for at least two years. This can prevent another flare-up and reduce the risk of colon cancer. Depending on the extent of the inflammation, local application (foam, suppository) or systemic application (tablets) can be useful. Sometimes it is also necessary to administer mesalazine both locally and systemically.
In addition to mesalazine, sulfasalazine is also a 5-ASA preparation. Both substances are equally effective. However, sulfasalazine carries a higher risk of side effects. Therefore mesalazine should be preferred for maintenance therapy.
If, despite the daily 5-ASA application, there is another surge, the future maintenance therapy will be "expanded" (therapy escalation): The doctor can, for example, increase the 5-ASA dosage or instead prescribe immunosuppressants or TNF antibodies. The optimal duration of use of the last two groups of active ingredients is not yet known.
Cortisone is not suitable for maintenance therapy in ulcerative colitis: It is not effective for this purpose and can cause serious side effects (osteoporosis, cataracts, etc.) if used over a long period of time.
If mesalazine is not tolerated, ulcerative colitis patients are sometimes given preparations containing Escherichia coli Nissle. These are non-pathogenic intestinal bacteria that are supposed to extend the symptom-free intervals. So far, however, there are only a few studies on the use of E. coli Nissle as maintenance therapy for ulcerative colitis. This is why there is still no final assessment by experts.
Ulcerative colitis: surgery
Sometimes, ulcerative colitis can no longer be controlled with medication. Then an operation is inevitable. The same applies if colon cancer or a precursor to it has been detected. In the case of a toxic megacolon and severe bleeding that cannot be stopped, an operation must be performed as soon as possible!
During the procedure, the surgeon removes the entire colon with the rectum (proctocolectomy). He forms a sac from part of the small intestine, which he connects to the anus. Once everything has healed, this sac acts as a new rectum. Until then, the stool can be emptied through an artificial anus that the surgeon temporarily creates.
After the operation, patients no longer need ulcerative colitis medication. However, stool behavior can change: some patients have more bowel movements after the procedure than before. In addition, the stool can be thinner and greasy.
Ulcerative colitis: you can do it yourself
See a doctor at the first sign of blood in your stool. If the flare-up therapy is started early, it can shorten and soften the flare-up. You should remain in bed during a severe, acute flare-up.
Get psychological help! A psychologist or psychotherapist can help you cope better with your illness. Better handling, on the other hand, can alleviate the symptoms - do not underestimate the influence of the psyche!
Join a support group for people with ulcerative colitis (or inflammatory bowel disease in general). Exchanging ideas with other sufferers can help to cope with the disease.
Alternative healing methods for ulcerative colitis such as TCM (including acupuncture) or herbal medicine are sometimes used to support conventional medical treatment. To improve the quality of life and wellbeing, you can try relaxation techniques, yoga, meditation or regular exercise (such as jogging), for example.
Ulcerative colitis: diet
In general, there are no special requirements for nutrition in ulcerative colitis. Affected people should pay attention to a balanced, varied menu.
In ulcerative colitis, deficiency symptoms can easily occur. These include, for example, deficiencies in iron, zinc, vitamin B12 or folic acid and anemia. Decreased bone density (osteopenia) or bone loss (osteoporosis) and malnutrition can also be the consequences of ulcerative colitis. In such cases, an individually adapted diet is very useful, for example lots of calcium-rich foods for weak bones. Sufferers should ask their doctor or nutritionist for advice.
In the case of severe deficiency symptoms, additional preparations containing the missing vitamins or minerals should be taken in consultation with the attending physician.
Some ulcerative colitis patients do not tolerate certain food components generally or during a flare-up. The diet should take this into account. For example, if you have an intolerance to milk sugar (lactose intolerance), you should avoid or at least limit the consumption of milk and dairy products such as cheese or yoghurt.
In acute attacks, experts advise eating little fiber (for example whole grain bread or legumes). Because the insoluble fibers make the stool swell and stimulate bowel movements - very unfavorable if you already have diarrhea. Coffee and hot spices should also be avoided because they can additionally irritate the intestinal mucosa.
Ulcerative colitis: causes and risk factors
As for most chronic inflammatory bowel diseases, the same applies to ulcerative colitis: The causes and risk factors are so far hardly known.
Obviously, a genetic predisposition plays an important role here. Because ulcerative colitis sometimes occurs more often in families. For example, siblings of patients have a 10 to 50 times higher risk of developing ulcerative colitis than the normal population.
Genetic predisposition alone does not lead to the onset of ulcerative colitis. Diet, infections and a disturbed immune system could also be involved in the development of the disease. The psyche may also have an influence, such as separation fears.
In the case of existing ulcerative colitis, psychological stress can also trigger or intensify a disease flare-up.
There is evidence that people who have had their appendix removed are less likely to develop ulcerative colitis. The reason for this is not known.
Ulcerative colitis: examinations and diagnosis
The clarification of (suspected) ulcerative colitis consists of several components. First, the doctor will have a detailed conversation with the patient in order to collect his or her medical history (anamnesis): Among other things, he will have the symptoms described in detail and ask about any previous illnesses as well as any known ulcerative colitis diseases in the family. Other important information for the doctor is, for example, whether the patient smokes or has smoked and is taking any medication regularly.
Physical examination
The anamnesis will be followed by a physical examination. This also includes the doctor feeling the patient's anus with one finger (digital rectal examination). In ulcerative colitis, a complication can be a tumor in the rectum, which can often be felt in this way.
Blood tests
The next important step is a blood test: Various parameters are measured in the patient's blood, for example the inflammation values CRP (C-reactive protein) and blood sedimentation (erythrocyte sedimentation rate, ESR). The electrolytes sodium and potassium are also determined. Because of the frequent diarrhea, a corresponding deficiency may have developed.
The amount of blood protein albumin provides information on the nutritional status of the patient. Elevated levels of the liver enzymes gamma-GT and alkaline phosphatase (AP) may indicate whether inflammation of the biliary tract has developed inside and outside the liver (primary sclerosing cholangitis) - a complication of ulcerative colitis. Other blood parameters are also determined, for example white blood cells (leukocytes), iron values and kidney values.
Stool examination
With ulcerative colitis, certain germs (bacteria, viruses, parasites) can easily spread in the intestine - especially during an acute attack. A stool test will be done to rule out such an infection.
Colonoscopy
A reliable way to detect ulcerative colitis and determine its extent is a colonoscopy. A thin, flexible, tubular instrument (endoscope) is inserted through the anus and advanced into the large intestine. At the top of the endoscope is a tiny camera and a light source. This allows the doctor to examine the intestine from the inside.In this way, changes in the mucous membrane and inflammation, such as those that occur in ulcerative colitis, can be recognized. The doctor can also use the endoscope to take a tissue sample so that it can be analyzed in the laboratory.
After the diagnosis of ulcerative colitis, regular colonoscopies are done to check it.
It is often not easy to differentiate between the two chronic inflammatory bowel diseases, ulcerative colitis and Crohn's disease. In cases of doubt, the remaining digestive tract must therefore also be examined endoscopically. In Crohn's disease, inflammation and changes in the mucous membrane can also be found there. Using what is known as esophagogastroduodenoscopy, the esophagus, stomach and duodenum (uppermost section of the small intestine) are examined using an endoscope. The doctor can also take tissue samples.
The entire small intestine can be viewed more precisely from the inside using capsule endoscopy. The tiny endoscope the size of a vitamin capsule is swallowed and films the inside of the digestive tract on its way to the anus. The images are sent via the built-in transmitter to a data recorder that the patient carries with him. The method is very gentle. However, no tissue samples can be taken.
Imaging procedures
The abdomen is examined by ultrasound (sonography) both for diagnosis and repeatedly in the further course of the disease. For example, the doctor can identify inflamed sections of the intestine. A highly dilated intestine (megacolon) as a dangerous complication can also be detected on ultrasound. In this case, the doctor will also have an X-ray of the bowel done.
In certain cases, other imaging techniques are needed. For example, if there is a narrowing in the large intestine (colon stenosis), the doctor will order a computed tomography or magnetic resonance tomography (MRI) scan and take a tissue sample from the abnormal area. Colon cancer is suspected here!
Patients with ulcerative colitis are at increased risk of developing colorectal cancer. Therefore, you should go to your doctor for regular check-ups.
Ulcerative colitis: disease course and prognosis
As with the onset, the course of the disease in ulcerative colitis cannot be predicted. Most of the time the disease is relapsing. Physical and psychological stress can trigger a flare-up. The time between two consecutive attacks can vary. The symptoms during an episode are not equally severe in every episode and in every patient.
Depending on the extent of the inflammation, the prognosis for ulcerative colitis also varies. The symptoms and the course of the disease can be kept under control by means of medicinal treatment. If ulcerative colitis is limited to the rectum, this is usually sufficient for the affected person to be able to lead a reasonably normal life with a normal life expectancy. The more extensive the inflammation in the intestine, however, the more difficult the treatment and prognosis of ulcerative colitis are often. The only way to cure the disease at the moment is to remove the entire large intestine.
Pouchitis
One possible consequence of the removal of the large and rectum is what is known as pouchitis: the pouch is the name given to the sac-like reservoir of the small intestine, which is formed into an artificial rectum in the course of the operation. This becomes infected in about half of the patients in the years after the operation. The signs of pouchitis include diarrhea, bleeding from the intestines, and a fever. Cortisone enemas or antibiotics can help reduce the inflammation.
Pouchitis can also become chronic.
Increased cancer risk
Ulcerative colitis increases the risk of colon cancer - especially if the inflammation of the bowel is very widespread. The duration of the illness also plays a role: after 15 to 20 years of ulcerative colitis, around eight percent of patients develop colon cancer. If it is not recognized and treated in good time, this can significantly reduce the life expectancy of those affected. Therefore, regular check-ups (colonoscopy with sampling) are recommended in ulcerative colitis. Ulcerative colitis patients can find out from their doctor at which intervals the examinations make sense.
Additional information
Books:
- Chronic inflammatory bowel disease: Crohn's disease / ulcerative colitis from the German Crohn's disease / ulcerative colitis Association - DCCV e.V., HIRZEL, 2006
- The great patient guide for Crohn's disease and ulcerative colitis by Julia Seiderer-Nack, Zuckschwerdt, 2013
Guidelines:
- Guideline "Ulcerative Colitis" of the German Society for Gastroenterology, Digestive and Metabolic Diseases
Self help:
- DCCV e.V. - German Crohn's Disease / Ulcerative Colitis Association: https://www.dccv.de/








.jpg)



-mit-mickymaus-am-tannenbaum.jpg)