Poisoning of pregnancy
Mareike Müller is a freelance writer in the medical department and assistant doctor for neurosurgery in Düsseldorf. She studied human medicine in Magdeburg and gained a lot of practical medical experience during her stays abroad on four different continents.
More about the experts All content is checked by medical journalists.Pregnancy poisoning is a disorder of the body to adapt to the changes that occur during pregnancy. Any woman can be affected, but there are risk factors that make it more likely to occur. But what exactly is pregnancy poisoning? Why can it be dangerous for mother and child? And how is pregnancy poisoning treated? You can read answers to these and other questions here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. O16O12O11O14O15O10O13

Pregnancy poisoning: description
The term pregnancy poisoning is actually out of date, but is still often used in everyday language. He refers to an earlier theory that certain substances released in the body during pregnancy cause poisoning. According to the current state of science, this is not the case. Rather, pregnancy poisoning is a disorder of the body to adapt to the changes during pregnancy.
Diseases that are triggered by pregnancy are known as gestoses. A distinction is made between early gestosis, such as vomiting in the morning during the second to fourth month of pregnancy, and late gestosis, which includes pregnancy poisoning. They appear after the 20th week of pregnancy. The late gestoses are also referred to as hypertensive pregnancy diseases because they all have high blood pressure (hypertension). They include:
- High blood pressure of pregnancy (gestational hypertension)
- Preeclampsia (EPH gestosis)
- Eclampsia
- HELLP syndrome
- Graft gestosis
Pregnancy poisoning: occurrence
According to the guideline on high blood pressure diseases during pregnancy, six to eight percent of all pregnant women suffer from it. They are one of the most common reasons mothers die during pregnancy.
Preeclampsia develops from pregnancy high blood pressure in almost half of those affected, with ten percent of them developing severe preeclampsia. This can lead to a HELLP syndrome. In Europe, preeclampsia occurs in around two percent of all pregnant women each year. 70,000 women worldwide die of preeclampsia every year.
Women who had high blood pressure before the onset of pregnancy and who continue to suffer from it for more than twelve weeks after giving birth have chronic hypertension. During pregnancy, this can develop into graft clampsia in one in four women.
Pregnancy poisoning: symptoms
To find out what signs there are of pregnancy poisoning, see Pregnancy poisoning: symptoms.
Pregnancy poisoning: causes and risk factors
The exact mechanism by which pregnancy poisoning develops has not yet been conclusively researched. Doctors currently assume that it is a disorder of the body to adapt to the changes in pregnancy. Various factors play a role here. Among other things, one assumes a disorder in the placenta. This can lead to changes in the expectant mother's blood vessels and activate her immune system. As a result, fluid escapes from the vessels, water retention (edema) forms and blood clotting is activated.
Pregnancy poisoning: who does it affect?
In principle, every woman can get a gestosis. There are, however, some risk factors that favor the occurrence of pregnancy poisoning. These include:
- Occurrence of gestosis in a previous pregnancy
- Pregnancy with multiple births
- Age of pregnant women under 18 or over 40 years
- Autoimmune diseases
- Blood clotting disorders
- first pregnancy
- obesity
- Diabetes mellitus
- Occurrence of gestoses in close relatives
- Kidney disease
Pregnancy poisoning: examinations and diagnosis
To find out about pregnancy poisoning, see your gynecologist. First, he asks you in detail about your medical history (anamnesis). He will ask you the following questions, among others:
- Did you have high blood pressure before you became pregnant?
- Is there any known case of pregnancy poisoning in your family?
- Have you had a gestosis in a previous pregnancy?
- Do you have upper abdominal pain or visual disturbances?
There is no specific test for diagnosing gestosis. Women are therefore subjected to various examinations:
First, your blood pressure will be measured. It is often increased in pregnancy poisoning. In rare cases it can have normal values.
Your weight will also be checked. Rapid weight gain can speak for the retention of water and an EPH gestosis.
Your urine will also be checked for proteins. Normally there are no proteins in the urine of healthy people.
In addition, your blood will be drawn and examined in the laboratory. If the liver enzymes (transaminases) are increased, this can indicate damage to the liver in the context of pregnancy poisoning. The amount of blood platelets is also important: Decreased values can indicate a HELLP syndrome.
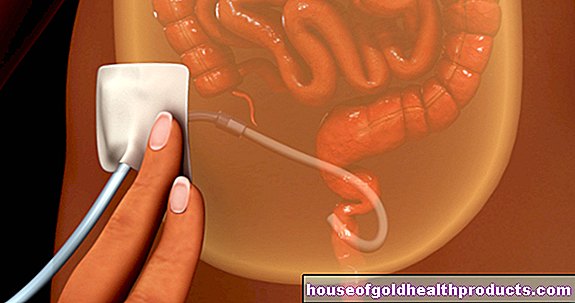
Cardiotocography (CTG) should be performed to assess the situation of the unborn child. With the help of the CTG, the child's heartbeat and contractions are monitored. An ultrasound examination (sonography) can also provide information about the baby's blood supply and growth.
Sonography can also be used to detect changes in the mother's liver. If the results are not clear, magnetic resonance imaging (MRI) can be performed.
Pregnancy poisoning: treatment
Treatment depends on the type of pregnancy poisoning and the symptoms. Water retention (edema), for example, can be treated with simple measures such as:
- Elevate the legs
- Wearing tight bandages or stockings
- 37 ° C warm baths
If you only have mild pregnancy high blood pressure without other symptoms, the therapy can be carried out on an outpatient basis. In doing so, you should definitely avoid or reduce stress.Your gynecologist may issue you with a certificate of incapacity for work or a work ban. In addition, you should have weekly check-ups with your gynecologist.
From a blood pressure of 150/100 mmHg, pregnant women should be treated as inpatients in the hospital.
Pregnancy poisoning: therapy in the hospital
In the clinic, you can be constantly monitored and given certain antihypertensive drugs. This is important because lowering blood pressure can prevent life-threatening complications such as cerebral haemorrhage. Various active ingredients can be used as antihypertensive agents. Most commonly, α-methyldopa, nifedipine, or metoprolol are used to lower blood pressure over the long term. In the acute situation, nifedipine, urapidil or dihydralazine are usually administered. The antihypertensive drugs should be slowly reduced in dose in the three months after the birth and finally discontinued completely.
Magnesium is given to prevent or treat eclampsia.
That being said, it is important to monitor the baby's health. This works best with the CTG.
The only way to treat preeclampsia causally is to give birth to the child. In patients who have already completed the 37th week of pregnancy, childbirth is usually initiated. The baby is then mature enough for life outside the womb. Childbirth is considered in women between the 35th and 37th week of pregnancy with severe preeclampsia. Between the 25th and 34th week of pregnancy, drug treatment is preferred and early delivery is postponed as long as possible. Before the completed 24th week of pregnancy, an individual decision is made as to whether the pregnancy is to be terminated. The focus here is on averting mortal danger for the mother.
If, in the case of pregnancy poisoning, premature delivery is necessary, although the baby's lung maturation has not yet been completed, this can first be accelerated with medication. To do this, the mother is injected with the glucocorticoid betamethasone once, between the 25th and 34th week of pregnancy, preferably at least 48 hours before the birth.
In the case of HELLP syndrome, childbirth is often initiated immediately, because otherwise the situation can be life-threatening for both the mother and the child.
Pregnancy poisoning: precaution
If women already had preeclampsia or a similar illness in an earlier pregnancy, they will be treated with acetylsalicylic acid (ASA) from the 16th week of pregnancy up to the 34th week of pregnancy at the latest. This lowers the risk of pregnancy poisoning occurring again up to the 37th week of pregnancy. A general intake of ASA during pregnancy is not recommended.
Regardless of possible risk factors, all pregnant women from the 20th week of pregnancy are tested for proteins in their urine. In addition, blood pressure should be checked at every preventive medical check-up. If it is too high, but no further symptoms exist, a long-term blood pressure measurement over 24 hours can first be carried out for more precise control. In addition, pregnant women can regularly check their blood pressure in the morning and in the evening in order to identify any possible increase in good time.
Pregnancy poisoning: the course of the disease and prognosis
Pregnancy poisoning can take many courses. Therefore, after the diagnosis, constant monitoring of mother and child is crucial. The different types of hypertensive pregnancy diseases can partially merge into one another. Gestational hypertension can initially develop into preeclampsia and then into eclampsia or HELLP syndrome. Eclampsia can develop suddenly even without any previous symptoms and become life-threatening for the pregnant woman within a few hours.
In general, the following applies: the various diseases are usually more serious for the expectant mother than for the child - there is a risk of cerebral hemorrhage, kidney failure and ruptured liver. In the unborn child, maternal high blood pressure can delay growth. A HELLP syndrome can also be life-threatening for the unborn child if the placenta is prematurely detached.
Women who have already had pregnancy poisoning are at increased risk of it happening again in the next pregnancy. Preeclampsia and HELLP syndrome are repeated in around 15 percent of those affected.
Tags: sports fitness skin care organ systems