Celiac disease
Ricarda Schwarz studied medicine in Würzburg, where she also completed her doctorate. After a wide range of tasks in practical medical training (PJ) in Flensburg, Hamburg and New Zealand, she is now working in neuroradiology and radiology at the Tübingen University Hospital.
More about the experts All content is checked by medical journalists.Celiac disease is an inflammatory bowel disease. It is triggered by a misdirected immune reaction to the adhesive protein gluten, which is found in many types of grain. Patients experience severe diarrhea and abdominal pain when they ingest foods containing gluten. So far, therapy has mainly been limited to a lifelong gluten-free diet, under which the symptoms no longer occur. Here you can read how celiac disease develops and which symptoms it triggers.
Once the diagnosis of celiac disease has been confirmed, a gluten-free diet should be followed for life.
Dr. med. Mira Seidel
Celiac Disease: Brief Overview
- Description: Overreaction of the immune system to the adhesive protein gluten and an endogenous enzyme that breaks it down; Inflammation of the lining of the small intestine; Deficiency symptoms due to poor nutrient absorption.
- Symptoms: occur after eating foods containing gluten: abdominal pain, flatulence, diarrhea, often atypical symptoms.
- Treatment: gluten-free diet, no wheat, barley, rye, green spelled, etc., compensation for deficiencies, so far no causal therapy.
- Diagnostics: Celiac disease test: detection of antibodies in the blood, biopsy of the small intestinal mucosa, self-tests only provide inadequate results.
- Prognosis: If left untreated, complications can develop, such as lactose intolerance or cancer of the gastrointestinal tract.
What is Celiac Disease?
In celiac disease, the small intestine becomes inflamed. The immune system is to blame. It classifies the actually harmless adhesive protein gluten as dangerous and overreacts as soon as patients ingest gluten in their food. This is found in many types of grain such as wheat, rye, barley, spelled or green spelled. The immune system of celiac disease patients is also triggered by an endogenous substance: the enzyme tissue transglutaminase. It splits the gluten in healthy people.
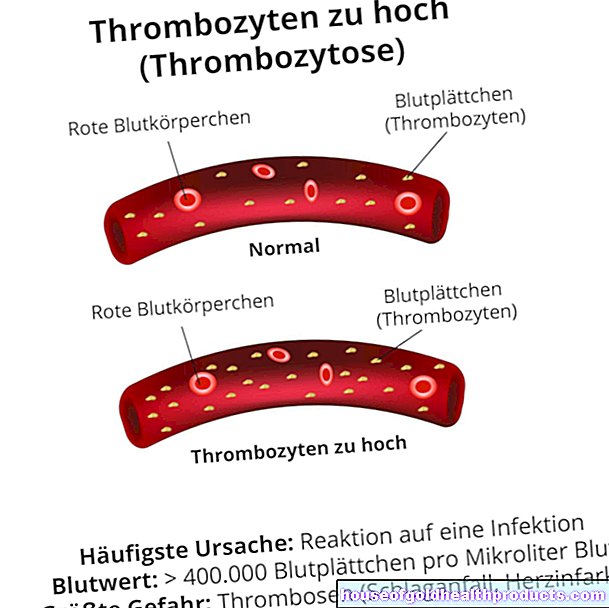
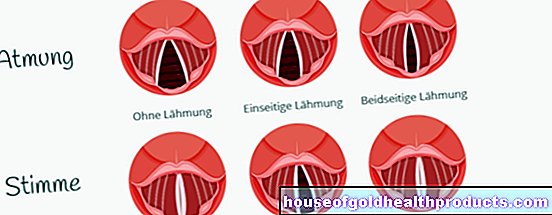
Because gluten and tissue transglutaminase are located on the intestinal mucosa, it becomes inflamed when the immune system attacks it. Over time, the mucous membrane is so badly damaged by the chronic inflammation that the food can no longer be absorbed normally through the intestine into the blood. The intestinal mucosa is usually wrinkled and forms so-called villi. This structure increases the surface area of the intestine. This has the advantage that the food components can pass from the intestine into the blood more quickly. In celiac disease, the auto-antibodies destroy these protuberances. The result: Serious deficiency symptoms can occur because less surface is available for nutrient absorption.
This is how the villi change in celiac disease
Allergy or Autoimmune Disease?
Experts also argue about whether celiac disease is an allergy or an autoimmune disease. The fact is, celiac disease has elements of both an allergy and an autoimmune disease.
An allergy is generally an excessive reaction of the immune system to actually harmless substances. This is the case with celiac disease, as the immune system reacts to the actually harmless gluten with an excessive immune response.
On the other hand, in celiac disease, the immune system also forms antibodies against the body's own enzyme tissue transglutaminase. Since the immune system also attacks the body's own structures in celiac disease, the definition of an autoimmune disease is also met for gluten allergy. According to the current state of knowledge, celiac disease is most likely a hybrid of allergy and autoimmune disease. However, the term gluten allergy has not caught on in science and should therefore be avoided.
Celiac disease: symptoms
If people with celiac disease consume foods containing gluten, they experience typical symptoms. These primarily include abdominal pain, gas and greasy diarrhea. In addition to these short-term symptoms, there are also long-term impairments: In celiac disease, the mucous membrane of the intestine is damaged by the inflammation, so that all food components are more difficult to absorb into the body. This can lead to severe deficiencies, such as iron deficiency. This makes it harder for the body to hold water in the vessels. Instead, it accumulates in the tissue - edema forms. Celiac disease patients often lose weight over the long term due to gastrointestinal complaints.
Atypical symptoms
In some patients, gluten intolerance shows up with atypical symptoms, i.e. complaints that are not directly related to bowel function, for example skin problems. Celiac disease is then often recognized late. The most common atypical symptoms include:
- Liver disease with slightly elevated liver values in some cases
- Skin inflammation with itchy reddish raised blisters
- Anemia, burning tongue, lazy licking of the mouth (due to iron deficiency)
- Osteoporosis, muscle weakness, muscle cramps, bone pain (due to lack of calcium)
- Bleeding, for example in the skin (due to vitamin K deficiency)
- Night blindness (due to a vitamin A deficiency)
- Thyroid dysfunction
- Inflammation of the kidney corpuscles
- Joint discomfort
- Mood swings
- depression
- Epileptic seizures
- Movement coordination disorder
- Nerve disorders
Celiac Disease Symptoms in Children
Even in a toddler, gluten intolerance can cause indigestion symptoms. These can manifest themselves as a bloated stomach, voluminous, foul-smelling diarrhea or refusal to eat. Some children get noticed at pediatrician checkups because they are no longer growing properly or their puberty is delayed. Iron deficiency is also a typical symptom of gluten intolerance in children. Signs of celiac disease can also be changes in the nature or behavior of the child. The children are then noticeably tearful, grumpy or apathetic. Celiac disease symptoms in children often appear towards the end of the first year of life, i.e. around three to six months after the first gluten-containing cereal meal.
Subclinical Celiac Disease
In some people, the typical antibodies for celiac disease can be detected in the blood and the mucous membrane of the small intestine is also characteristically changed. Nevertheless, the patients have no complaints. Doctors then speak of subclinical celiac disease (formerly: "silent" celiac disease). This form is usually discovered during a screening examination, which is carried out, for example, if close relatives have celiac disease.
A gluten-free diet can also be useful for completely asymptomatic patients. It is true that the benefits have been less extensively researched than with "typical" celiac disease. Nevertheless, studies indicate that the risk of secondary diseases such as osteoporosis is increased even with a subclinical clinical picture.
If you have been diagnosed with celiac disease on the basis of laboratory values and a tissue sample, but you do not have any symptoms, then let your doctor explain the advantages and disadvantages of a gluten-free diet in detail.
People who have no obvious symptoms of celiac disease still suffer from unspecific, very weak, or elusive symptoms. They report, for example, a feeling of exhaustion and tiredness. So-called subclinical celiac disease can also be present here. The symptoms often improve with a gluten-free diet.
Children and adolescents with typical blood changes and abnormal intestinal mucosa should definitely eat a gluten-free diet - even if there are no symptoms. Otherwise, disturbances in bone metabolism and growth can occur at an early stage.
Potential Celiac Disease
Sometimes celiac disease antibodies can be detected even before the lining of the small intestine has changed. This can lead to celiac disease with symptoms - but that doesn't have to happen. Doctors refer to this form as potential celiac disease (formerly also known as "latent" celiac disease).
If such a constellation occurs, doctors test further parameters or repeat the diagnosis. The further recommendations are then based, for example, on existing deficiency symptoms and the symptoms of the person affected. It is often sufficient to monitor the potential celiac patient and regularly check the typical parameters.
Celiac Disease: Treatment
If a person suffers from celiac disease, the disease will be with them for the rest of their lives. So far there is no curative therapy. If an affected person wants to alleviate their symptoms and reduce the risk of secondary diseases, then they have to eat permanently gluten-free. If he follows this gluten-free diet consistently, the symptoms of celiac disease almost always recede completely. As part of the celiac disease treatment, any existing deficiencies are compensated for until the affected intestine has normalized.
Celiac Disease Treatment: Diet
Newly diagnosed celiac disease patients initially feel extremely restricted in their diet. In fact, from now on they have to remove a large number of foods from the menu. However, the more information about a gluten-free diet is available to those affected, the more opportunities they will find to eat gluten-free and yet varied.
The following information will help you as to which types of grain and foods you should avoid if you have gluten intolerance and which ones you can safely consume:
Strictly avoid: cereals containing gluten
If you have gluten intolerance, you should completely and permanently avoid the following types of grain and products that contain them:
- wheat
- rye
- barley
- Spelt
- Green kernels
- Triticale
- Einkorn
- Emmer Kamut
- sometimes oats (does not cause symptoms in all those affected)
Foods containing gluten
Gluten can also be found in many cereal products. In principle, manufacturers have been obliged since 2005 to label foods containing gluten in accordance with the allergen labeling requirement. Ingredients containing gluten, such as wheat, must appear on the list of ingredients (exceptions: syrup, spirits). However, there is no need to mention the term “gluten” itself. So it is necessary for people with celiac disease to know which ingredients contain gluten. A food is considered gluten-free if it contains a maximum of 20 ppm (2 mg per 100 g) of gluten. There is also a special symbol that identifies gluten-free foods: a crossed-out cereal ear.
The following foods almost always contain gluten. As a celiac patient, you should avoid these as well.
- Bread and other baked goods
- Pasta
- Pizza
- Muesli and other breakfast cereals
- Cookies
- breaded meat
- Malt coffee
- beer
- Soy sauce (gluten-free soy sauce is also available)
Gluten-free cereals
Fortunately, there are also some types of grain that do not contain gluten and are therefore safe for people with gluten intolerance. Gluten-free grains include:
- rice
- Corn
- millet
- Buckwheat
- Amaranth
- Quinoa
- Wild rice
- Teff (dwarf millet)
Gluten free foods
The following foods do not naturally contain gluten. They can therefore be eaten without hesitation (provided they do not contain any gluten-containing additives):
- All types of fruit and vegetables
- potatoes
- Meat, poultry, fish, seafood
- Legumes such as soy
- Eggs, milk, dairy products, butter, margarine
- Jams, honey
- Sugar, salt, herbs
- Nuts and oils
- Water and juices
- Wine and champagne
- coffee and tea
Celiac disease treatment: therapy for deficiency symptoms
In celiac disease, the intestines become inflamed due to attacks by the immune system. This can disrupt the normal absorption of nutrients into the blood. In particular, vital vitamins and trace elements are affected and must be supplied in the event of a deficiency caused by celiac disease. When it comes to vitamins, there is often a lack of vitamin A, vitamin B6 and B12, folic acid and vitamin K. But the trace elements iron, magnesium and calcium are often only insufficiently absorbed in celiac disease.
The various deficiencies can sometimes have serious consequences. For example, too little iron, folic acid or vitamin B12 triggers anemia. The lack of vitamin K can lead to severe bleeding. A typical consequence of calcium deficiency is muscle cramps.
If deficiency symptoms occur, the missing vitamins and trace elements must be supplied artificially. In lighter cases, this can be done in the form of tablets or capsules. Sometimes, however, an infusion into the vein or at least an injection into the muscle is necessary, as the inflamed intestine cannot absorb the missing substances sufficiently.
Celiac disease treatment in babies
If a pregnant woman has celiac disease or if there are relatives with this disease in her family, she should breastfeed her child for as long as possible. Breast milk has been shown to have a protective effect against celiac disease. Studies from the USA and Sweden also suggest that small amounts of foods containing gluten may also have a preventative effect in middle infancy. This had the greatest effect in the fifth to seventh month of life. This means that children who were fed gluten-containing foods at this age, later suffered from celiac disease less often. In contrast, children who come into contact with gluten earlier appear to be at greater risk of developing celiac disease.
If celiac disease is suspected in babies or children, it should be checked immediately whether gluten intolerance is responsible for the symptoms. Otherwise, undetected and therefore untreated celiac disease can lead to severe developmental disorders due to the lack of vitamins, trace elements and nutrients.
Untreatable Celiac Disease
The so-called refractory celiac disease is a very rare form that occurs in around 1.5 percent of celiac disease patients. In refractory celiac disease, the typical signs of gluten intolerance can be found in the blood and in a sample of the small intestine. However, the person affected cannot positively influence the disease with a strict gluten-free diet. Refractory celiac disease is when the symptoms do not subside during a twelve-month gluten-free diet or when typical or atypical celiac disease symptoms recur after improvement. In this case, the symptoms can only be relieved with medication. Research is being carried out into causal therapeutic approaches.
-
Gluten sensitive after gastrointestinal flu
Three questions for
Dr. med. Daniel Plecity,
Specialist in internal medicine, gastroenterology -
1
Is it generally healthier for people to avoid gluten?
Dr. med. Daniel Plecity
No, the opposite is often the case. Gluten-free bread from industrial production often contains less fiber and vital substances. However, many people feel that certain foods are not good for them. Research is constantly providing new insights, for example the so-called FODMAPs - a group of foods to which some react sensitively. If you have digestive problems, seek advice from your doctor.
-
2
Celiac disease or only sensitive to gluten - how do I tell the difference?
Dr. med. Daniel Plecity
Celiac disease can be clearly identified through a blood test and an endoscopy - after which it is necessary to avoid gluten for the rest of your life. Acquired gluten sensitivity can occur after a gastrointestinal flu, for example. But you can also get rid of them again, for example through an exclusion diet. After four to six weeks of gluten-free diet, you are slowly starting to gluten again. It's like desensitizing the intestines.
-
3
Do I really have to completely avoid gluten if I have celiac disease?
Dr. med. Daniel Plecity
Some patients eat gluten and have no real symptoms. However, this is not necessarily the same in the intestine. In principle, a persistent “irritation” from gluten increases the risk of local lymphoma. I always tell my patients that if there is no other option, then just eat gluten. However, you should not start to consume large amounts of gluten, but try to keep the recommendation to 90 to 95 percent.
-
Dr. med. Daniel Plecity,
Specialist in internal medicine, gastroenterologyDr. med. Plecity is the senior physician in charge of the internal medicine department at the Ebersberg district clinic.
Celiac Disease: Causes and Risk Factors
The mechanisms that take place in the body in celiac disease are already relatively well understood. However, it has not yet been clarified why celiac disease ultimately develops. Genetic factors, among other things, contribute to this. Since not all people with a corresponding predisposition actually get celiac disease, there must be other influencing factors. It is believed that diet and other environmental factors also play a role.
Hereditary factors
Hereditary factors are very likely to play a decisive role in celiac disease. About 90 percent of those affected have a certain surface protein on the immune cells. This protein binds fragments of gluten and is involved in the inflammatory immune response. Since it is inherited, family members of those affected have a ten to 15 times higher risk of developing celiac disease. Other autoimmune diseases such as a form of diabetes (type 1 diabetes mellitus) or autoimmune thyroid inflammation are also associated with this surface protein. However, around 30 to 40 percent of healthy people also have this surface protein. Therefore, environmental factors apparently also have an important influence on the development of the disease.
Nutrition and the environment
People who came into contact with gluten-rich foods as newborns are more likely to develop celiac disease. Baby food should - especially if the child has close relatives with gluten intolerance - consist of breast milk or gluten-free food. From the age of five months, small amounts of gluten can again have a preventive effect. Infections with intestinal viruses or a change in the bacterial intestinal flora are also discussed as possible risk factors. In addition, psychosocial factors should contribute to the development of celiac disease.
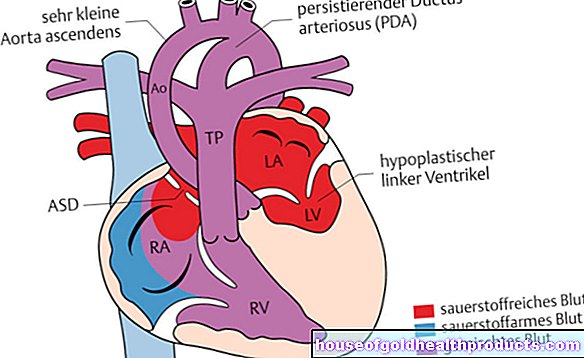
Connection with other diseases
Celiac disease occurs with other diseases. People with Turner syndrome, Down syndrome, IgA deficiency, type 1 diabetes and other autoimmune diseases such as autoimmune thyroid disease (thyroiditis) or liver inflammation (autoimmune hepatitis) are significantly more likely to develop gluten intolerance. It is still unclear why celiac disease occurs more frequently in these diseases.
Celiac Disease: Investigations and Diagnosis
The right person to contact if you suspect gluten intolerance is a specialist in internal medicine who specializes in diseases of the digestive tract (gastroenterologist).
Celiac Disease: Medical History and Physical Examination
First, the doctor asks about your current symptoms and any previous illnesses (anamnesis). If you suspect celiac disease or after a positive celiac disease self-test, he or she could ask you the following questions, for example:
- Have you suffered a lot from diarrhea or stomach pain lately?
- Have you accidentally lost weight in the past few weeks or months?
- In children and adolescents: Are there growth disorders? Is puberty delayed?
- Have you noticed any abnormalities on the skin?
- Does a family member have gluten intolerance?
- Have you ever had a celiac disease test or have you performed a self-test?
The anamnesis is followed by a physical examination. The doctor looks for celiac disease-specific abnormalities on the skin and tongue. He uses the stethoscope to listen to the abdomen to check for intestinal noises. He also taps and feels the patient, whereby he can detect increased air in the abdomen, fluid but also intestinal thickening. Since the intestine can only be assessed to a limited extent from the outside, further examinations are usually necessary for a celiac disease diagnosis.
Celiac Disease Test
A celiac disease test determines antibodies in the blood serum that are typical for gluten intolerance. In the case of pronounced celiac disease, a test using the air you breathe is also possible. There is also a self-test to detect gluten intolerance. However, this does not work particularly reliably. Under no circumstances should you rely on the result of the self-test, but always consult a doctor.
When to take the celiac disease test and how it works, read the article Celiac disease test.
In addition to the celiac disease test, a tissue sample can be taken from the small intestine. If this shows the typical changes in celiac disease, there is a gluten intolerance. The tissue sample can be dispensed with if symptoms typical of celiac disease occur, very high antibody levels are present and a typical genetic disposition for celiac disease is present.
If the diagnosis is uncertain despite the tests carried out, you should first follow a gluten-free diet for eight weeks. Following this, after a targeted gluten exposure, both the tissue sample and the celiac disease test can be repeated in the blood.
A diagnosis of celiac disease is not always easy because not all patients suffer from the typical symptoms. Up to 90 percent of those affected complain of atypical symptoms that are often not correctly interpreted for many years. It takes an average of four years for the diagnosis to be made.
Celiac disease: disease course and prognosis
Celiac disease is a disease that will last a lifetime. However, on a gluten-free diet, the symptoms usually go away completely. However, a gluten-free diet initially poses major problems for many people, as it means a massive cut in previous eating habits. However, if the person concerned deals in detail with the possibilities of a gluten-free diet, a varied diet is possible.
Celiac disease patients who have had the disease for a long time are at increased risk of certain cancers of the gastrointestinal tract (intestinal T-cell lymphoma, adenocarcinoma). In addition, the inflammation in the intestine can lead to serious deficiencies in vitamins, trace elements and other nutrients and other digestive disorders such as lactose intolerance. The intestinal inflammation leads to a deficiency of the lactase-breaking enzyme, which normally fulfills its function in the area of the intestinal lining of the small intestine. As a result, the milk sugar can no longer be digested, and lactose intolerance often occurs, at least temporarily. All of these consequences of illness are mostly irrelevant for people who know about their illness and can protect themselves with a gluten-free diet.
However, there are a large number of people who have not yet been diagnosed with celiac disease. Thanks to new examination options, the disease can now be diagnosed very easily. People with typical symptoms, associated comorbidities and relatives with celiac disease should be tested.
Celiac Disease: Frequency
Celiac disease is a common condition. It is estimated that around 1 percent of people worldwide suffer from gluten intolerance (as of 2018). However, the majority of those affected do not have a full picture of the disease. This means that many people have been shown to have celiac disease, but the symptoms are minor or moderate.
Overall, women are more often affected than men. Celiac disease in children occurs more frequently between the ages of one and eight and in adults between the ages of 20 and 50. In principle, however, the disease can develop at any age.
According to studies, the number of celiac diseases has increased steadily in recent years. On the one hand, this is probably due to the fact that the disease is now better known and can also be better diagnosed. Other reasons for this point to environmental factors such as gastrointestinal infections, changed eating habits and psychosocial factors. However, there is no clear explanation for the increase in the number of cases.
Additional information
Guidelines:
- S-3 Guideline of the German Society for Gastroenterology, Digestive and Metabolic Diseases: Celiac Disease, Wheat Allergy and Wheat Sensitivity
Self-help groups:
- German Celiac Society: www.dzg-online.de
- Austrian Working Group on Celiac Disease: www.zoeliakie.or.at
-
IG Celiac Disease of German Switzerland: www.zoeliakie.ch