Esophageal varices
and Martina Feichter, medical editor and biologistMareike Müller is a freelance writer in the medical department and assistant doctor for neurosurgery in Düsseldorf.She studied human medicine in Magdeburg and gained a lot of practical medical experience during her stays abroad on four different continents.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Esophageal varices are varicose veins of the esophagus. The enlarged veins occur mainly in advanced liver cirrhosis. Other diseases can also be the cause, for example right heart failure. If esophageal varices rupture and bleed, there is a danger to life! Read everything you need to know about symptoms, treatment, and prevention of esophageal varices.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. I85
How esophageal varices arise
Varicose veins in the esophagus (esophageal varices) are often complications of advanced liver cirrhosis. In this chronic liver disease, functional liver tissue is increasingly converted into functionless connective tissue - it scars. The more pronounced the scarring, the more the blood circulation in the liver is impaired. This can lead to esophageal varices and other complications. To understand this, it is necessary to take a closer look at blood flow through the liver:
The blood supply to the liver occurs, among other things, via the portal vein. This large vessel transports the blood from the intestine (with the absorbed nutrients) and from other abdominal organs (stomach, spleen, etc.) to the liver. It functions as the central metabolic organ in which countless substances are constantly being built up, converted and broken down, and harmful substances are detoxified. After flowing through the liver, the blood flows through the hepatic veins into the inferior vena cava and on to the right heart.
In cirrhosis of the liver, however, the increasing scarring of the tissue means that the blood can no longer flow properly through the liver. It accumulates in the portal vein in front of the liver. This causes the pressure inside the vessel to rise abnormally: a portal vein hypertension (portal hypertension) develops.
The congested blood looks for another route to the inferior vena cava, that is, bypass circuits are formed. One of them runs from the portal vein via gastric veins into the lower esophageal veins and in this way reaches the inferior vena cava. Because the veins of the esophagus are very thin-walled, however, they cannot withstand the increased blood flow: They expand and “rip off” - varicose veins develop in the esophagus (esophageal varices).
Warning: There are other diseases that can cause portal hypertension and, as a consequence, esophageal varices. These include a right heart failure (right heart failure) and a blockage of the portal vein by a blood clot (portal vein thrombosis).
In addition to esophageal varices caused by other diseases, there are also primary esophageal varices: These are not based on another disease, but on a congenital malformation of the vessels. But they are very rare.
Bleeding from esophageal varices
Over time, the increased blood flow can thin the wall of the esophageal veins so much that they burst. Doctors then speak of bleeding from the esophageal varices. Such bleeding is life-threatening and can lead to death within a very short time!
Esophageal variceal bleeding occurs in 30 percent of all cirrhotic patients and is one of the leading causes of death in the disease. The further the cirrhosis has progressed, the more likely patients are to die from bleeding from the esophageal varices.
At the highest risk of bleeding esophageal varices are patients who:
- have already had bleeding from the esophageal varices
- continue to drink alcohol (main cause of cirrhosis of the liver)
- have very large esophageal varices
Esophageal varices: symptoms
Esophageal varices usually do not cause any symptoms as long as they are intact. So those affected do not even notice them.
Only when esophageal varices tear do they suddenly become noticeable: The patients then suddenly vomit a large amount of blood in a gush. Due to the loss of blood and fluid, symptoms of hypovolemic shock also set in quickly. These include, for example, cool and pale skin, a drop in blood pressure, a racing heart, shallow breathing and impaired consciousness.
Warning: bleeding esophageal varices must be treated by a doctor as soon as possible - there is a high risk of death!
Esophageal varices: diagnosis
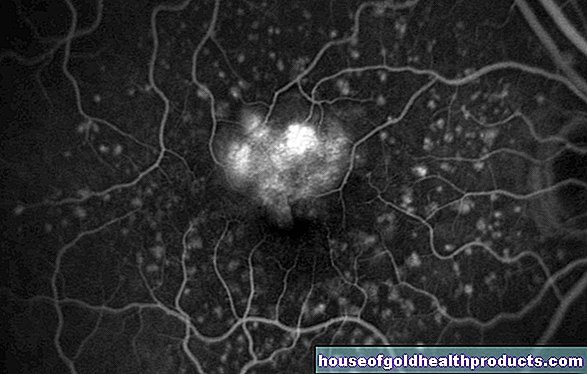
Esophageal varices can be detected with an endoscopy, more precisely with a reflection of the esophagus (oestrophagoscopy) or a gastroscopy (gastroscopy). A thin tube is inserted through the mouth into the esophagus (in a gastroscopy even further into the stomach). At the front end there is a light source and a small camera. This continuously takes pictures of the inside of the esophagus and transfers them to a monitor. Esophageal varices can usually be seen very quickly on the images.
If a patient vomits blood, bleeding from the esophageal varices is suspected. However, it can also be another source of bleeding in the upper digestive tract. These include, for example, stomach ulcers (ulcers) and inflammation of the gastric mucosa with damage to the mucous membrane (erosive gastritis).
Esophageal varices: therapy
If esophageal varices are discovered during an endoscopy, the doctor can obliterate them as a precautionary measure. Another method to reduce the risk of bleeding esophageal varices is the so-called rubber band ligation (variceal ligature): The dilated vein is tied off with a small rubber band or several rubber bands. As a result, it scars and can no longer bleed.
Both measures are possible within the scope of endoscopy: the doctor can insert the required fine instruments into the esophagus through the thin tube.
Esophageal variceal hemorrhage: therapy
If esophageal varices bleed, action must be taken quickly: the most important emergency measure is to stabilize the patient's circulation. A torn esophageal vein causes a lot of blood and fluid to be lost in a very short time. Therefore, the patient is given fluids directly into a vein and, if necessary, blood transfusions.
At the same time, one tries to stop the bleeding. Various methods are available for this:
First and foremost, endoscopic rubber band ligation (variceal ligature; as described above) is used for this. Additionally or alternatively, the doctor can administer drugs to stop bleeding such as somatostatin or terlipressin. They lower the blood pressure in the portal vein system.
Sometimes when the esophageal varices bleed, the affected vessel is also obliterated (as part of an endoscopy).
In the case of massive bleeding, a so-called balloon tamponade can also help: a small, empty balloon is inserted into the lower esophagus and then inflated. This compresses the blood vessels, which stops the bleeding. However, the method carries some risks. For example, inflating the balloon too much can tear the esophagus. The balloon can also slide towards the head and block the airway. Because of these risks, balloon tamponade is usually only performed if there is severe, uncontrollable bleeding from the esophageal varices.
As the disease progresses, patients are often given antibiotics as a precaution to prevent a possible bacterial infection.
Since esophageal variceal bleeding usually occurs with cirrhosis of the liver, the risk of hepatic coma must also be prevented. Normally, the blood that goes to the gastrointestinal tract after the bleeding is broken down with the help of the liver cells. Due to the cirrhosis of the liver, the liver is no longer able to do this sufficiently. Therefore, toxic metabolic products can accumulate. If they get to the head via the blood, they can damage the brain (hepatic encephalopathy). Therefore, the blood that is still in the esophagus has to be suctioned off. The patient is also given lactulose - a light laxative to cleanse the intestines.
Prevention of rebleeding
Within ten days of the first esophageal variceal bleeding, a varicose vein in the esophagus ruptures again in approximately 35 percent of patients. Within a year of the first bleeding, this even applies to 70 percent of patients.
The so-called secondary prophylaxis is therefore very important. It includes measures to prevent rebleeding of the esophageal varices. For example, many patients receive antihypertensive medication (such as propanolol) against portal blood pressure. Sometimes a variceal ligature is also performed as a precaution.
In certain cases it can also make sense to lay a so-called "shunt" (TIPS). This means that a connection is surgically established between the portal vein and hepatic veins, which bypasses the scarred tissue of the liver. This prevents the blood from taking a detour via the esophageal veins and causing new esophageal varices or enlarging existing ones.
Tags: anatomy Diagnosis desire to have children



.jpg)















.jpg)