Trisomy 13
Updated onClemens Gödel is a freelancer for the medical team.
More about the experts All content is checked by medical journalists.Trisomy 13 (Pätau syndrome) is a mostly severe, genetic disease with malformations of several organ systems. The diagnosis is often made before birth. There is no curative treatment for trisomy 13, but there is an accompanying one. The majority of those affected die in the womb or in their first year of life. Find out more about the symptoms, diagnosis and treatment of trisomy 13 here!

Trisomy 13: description
Trisomy 13, also known as (Bartholin's) Patau syndrome, was first described by Erasmus Bartholin in 1657. In 1960, Klaus Pätau found out the cause by introducing new technical methods: In trisomy 13, chromosome 13 occurs three times instead of normally only twice. The excess chromosome causes malformations and severe developmental disorders in the unborn child at a very early stage of pregnancy.
What are chromosomes
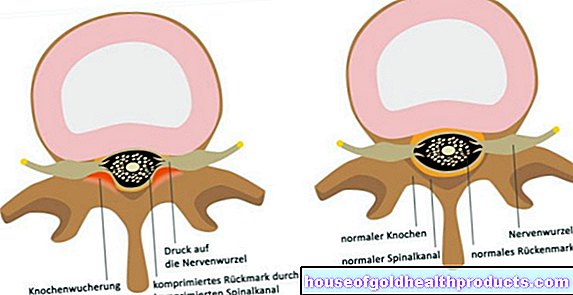
The human genome consists of chromosomes, which in turn are made up of DNA and proteins and are contained in the nuclei of almost all body cells. The chromosomes are the carriers of the genes and thus provide the blueprint of a living being.
A healthy person has 46 chromosomes, 44 of which are pairs of the same chromosomes (autosomal chromosomes) and two more define the genetic sex (gonosomal chromosomes). These two are known as either the X or Y chromosome.
In most cases, a deviation from this number of chromosomes (aneuploidy) is incompatible with life. The embryo cannot develop and the result is a miscarriage. However, there are a few forms of aneuploidy that affected children can survive with. In addition to trisomy 13, this also includes the much better known trisomy 21 (Down syndrome) with three chromosomes 21, or trisomy 18.
In all trisomies, the number of chromosomes is 47 instead of 46.
What types of trisomy 13 are there?
A distinction is made between different variants of a trisomy 13:
- Free trisomy 13: In 75 percent of the cases it is a so-called free trisomy. This means that there is an extra unbound chromosome 13 in all cells of the body.
- Mosaic trisomy 13: In this form of trisomy 13, the additional chromosome only occurs in a certain proportion of the cells. The other cells have a normal set of chromosomes. Depending on the type and number of cells affected, the symptoms of mosaic trisomy-13 can be significantly milder.
- Partial trisomy 13: In this form of trisomy 13, only a section of chromosome 13 is present in triplicate. Depending on the triple occurring section, more or fewer symptoms arise.
- Translocation trisomy 13: Strictly speaking, this is not a real trisomy, but the rearrangement of a section of chromosomes. Only a piece of chromosome 13 is attached to another chromosome (e.g. 14 or 21). Under certain circumstances, such a translocation does not lead to any symptoms. It is then referred to as a balanced translocation.
Occurrence
Trisomy 13 occurs in around 1 in 10,000 births. Presumably, the incidence of miscarriages is significantly higher. The frequency increases with the age of the mother. The Patau syndrome is thus the third most common viable aneuploidy - after trisomy 21 and 18.
Trisomy 13: symptoms
The list of possible trisomy 13 symptoms is long. Which complaints occur in the affected children depends on the individual case. The nature and severity of the symptoms of trisomy 13 can vary depending on the form of the disease. The more cells are affected, the more severe the consequences. In the case of mosaic and translocation trisomies, the severity of the symptoms may be so low that hardly any impairments are noticeable.
A free trisomy 13, on the other hand, is associated with severe malformations and disorders.
A classic symptom complex is the simultaneous appearance of the following signs:
- Small head (microcephaly) and small eyes (micropthalmia)
- Cleft lip and palate
- Extra fingers or toes (polydactyly)
These malformations are typical of trisomy 13, but do not have to be present in every case. Numerous other organ systems can also be affected.
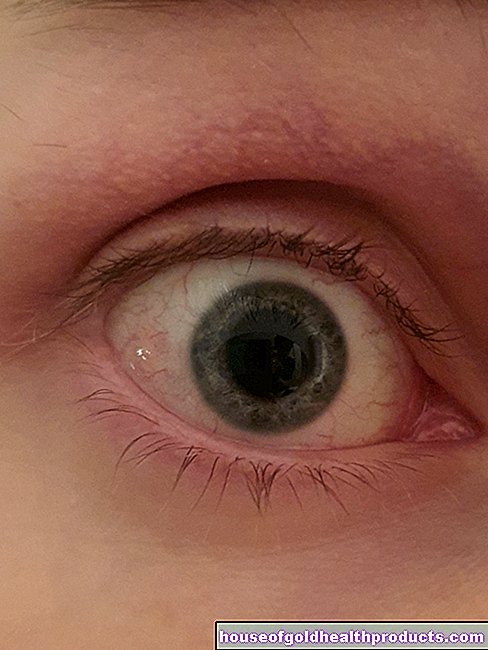
Face and head
In addition to microphthalmia, the eyes can be very close together (hypotelorism) and covered with skin folds. It is possible that the two eyes are fused into one (cyclopia), which is often associated with malformations of the nose (possibly missing nose). In a trisomy 13, the nose can also appear very flat and wide.
In addition, the ears, due to their relatively low position, and also the chin are often conspicuously shaped.
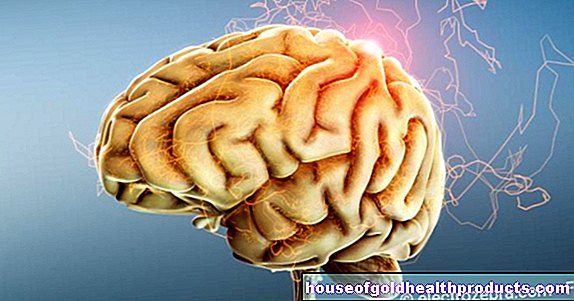
Central nervesystem
About 70 percent of trisomy 13 children have what is known as holoprosencephaly. The two halves of the brain are completely fused instead of - as in healthy people - only connected via a small part. As a result, the children are often very severely restricted intellectually, and they often suffer from epileptic seizures. Malformations of the cranial nerves, such as the auditory or olfactory nerves, can also result in corresponding functional failures.
The too small head and the lack of separation of the hemispheres can also lead to a water head (hydrocephalus). In addition, the neurological restrictions in the affected children often cause the muscles to become particularly slack (hypotension). All of this makes contact with the child difficult.
Internal organs
The internal organs in the chest and abdominal cavity are also affected by trisomy 13. A large number of different malformations (e.g. rotated arrangement of the organs in the abdominal cavity) can lead to a considerable restriction in daily life.
heart
80 percent of patients with trisomy 13 have heart defects. These are mainly defects in the dividing walls between the four heart spaces (septal defects). In addition, a so-called persistent ductus arteriosus is common. This is a kind of short circuit between the blood vessel (pulmonary artery) that extends from the heart into the lungs and the main artery (aorta).
This short circuit makes sense in the fetus because the unborn child does not breathe through the lungs, but receives oxygen-rich blood from the mother. After the birth, the ductus arteriosus usually closes with the first breaths. Failure to do this can seriously disrupt the newborn's bloodstream.
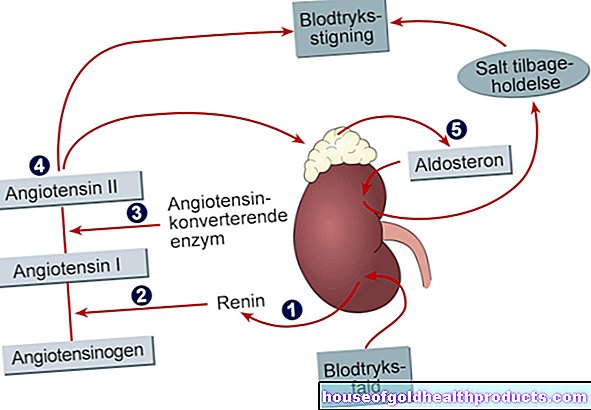
Kidney & urinary tract
Malformations of the kidneys and urinary tract are often present in trisomy 13. Among other things, cysts and horseshoe kidneys (merging of the kidneys in a horseshoe shape) occur. If the outflow of urine is obstructed, the urine often backs up into the kidneys. In the long run, this damages the kidneys (hydronephrosis).
Genital organs
In a newborn male, the testicles may not descend naturally from the abdomen into the scrotum. Usually this happens as part of natural development in the womb. If left untreated, developmental disorders of the sperm or even infertility are the result. The scrotum can also be abnormally changed. Newborn women may have underdeveloped ovaries and a malformed uterus (bicornuate uterus).
Hernias
A hernia is the displacement of the abdominal viscera through a natural or artificial gap in the abdominal wall. In trisomy 13, hernias occur primarily around the umbilical area, in the groin and at the attachment point of the navel (omphalocele).
skeleton
The skeleton is also not exempt from the consequences of trisomy 13. Numerous malformations of the bones are possible. In addition to an often additionally trained sixth finger (or toe), the hands and fingernails are often severely deformed. This sometimes results in the outer fingers pointing towards the center and resting on the inner fingers, so to speak. The foot can also be deformed in the form of a clubfoot.
Blood vessels
Finally, in a trisomy 13 (congenital) growths of small blood vessels (capillary hemangiomas) occur more frequently.They are primarily found in the skin, especially the face, and on internal organs such as the kidneys and liver.
Trisomy 13: causes and risk factors
The majority of trisomy 13 cases are the result of an error in the formation of the sex cells, i.e. the sperm and egg cells. These two cell types usually only have a single (half) chromosome set with 23 chromosomes. During fertilization, a sperm fuses with an egg cell, so that the resulting cell contains twice the chromosome set of 46 chromosomes.
So that the sex cells only have a single set of chromosomes before fertilization, their progenitor cells must divide into two sex cells, separating each pair of chromosomes. Errors can occur in this complicated process, for example a pair of chromosomes does not separate (non-disjunction) or a part of one chromosome is transferred to another (translocation).
After a non-disjunction, one of the resulting sex cells contains two chromosomes of a certain number, in this case number 13. In the other cell there is no chromosome 13 at all. One has 24 and the other only 22 chromosomes.
In many cases such an error is discovered by the body's own controls in cell development and the affected cell is “sorted out”. This may also only happen after fertilization and a spontaneous termination of pregnancy (abortion) occurs. If these control mechanisms do not work, however, the cells (with the defect) can continue to develop and even develop into a viable child - depending on the type and severity of the trisomy with more or less severe malformations.
In a mosaic trisomy 13, the error does not occur during the division of the sex progenitor cells, but rather at some point in the further development of the embryo. There are then already many different cells, one of which suddenly does not divide properly. Only this cell and its daughter cells have the wrong number of chromosomes, the other cells are healthy.
There is no clear answer to why some cells do not divide properly. Risk factors are the older mother's age during fertilization or pregnancy and certain substances that can disrupt cell division (aneugenics).
Is trisomy-13 hereditary?
A free trisomy 13 is theoretically hereditary, but the affected persons usually die before they reach sexual maturity. A translocation trisomy 13, on the other hand, can be symptom-free. A carrier of such a balanced translocation does not notice anything of the genetic defect, but with a certain probability passes it on to his offspring. There is then an increased risk of a pronounced trisomy 13 for them. A special genetic test can be used to test whether a translocation trisomy 13 is present.
If a healthy pair of parents already has a child with trisomy 13, the risk of further offspring of being born with a trisomy (also 18 and 21) increases. It is then around one percent.
Trisomy 13: examinations and diagnosis
Trisomy 13 specialists are specialized paediatricians, gynecologists and also human geneticists. Trisomy 13 is often diagnosed during pregnancy as part of preventive examinations. At the latest at birth, external changes and malfunctions of the cardiovascular system are usually noticeable. However, a mosaic trisomy 13 can also be relatively inconspicuous.
Prenatal examinations
In many cases there is already a suspicion of a trisomy 13 as part of the preventive examinations. The thickness of the neck fold of the fetus is routinely measured during ultrasound examinations of pregnant women. If this is thicker than usual, this already indicates an illness. Various blood values may provide further information and finally certain pathological organ changes confirm the suspicion of a trisomy 13.
Genetic tests
If there is any evidence of trisomy 13, prenatal genetic counseling including a prenatal examination is advisable. For this purpose, cells of the fetus are removed using special techniques from the amniotic fluid (amniotic fluid examination) or placenta (chorionic villus sampling) and subjected to a DNA analysis. Such invasive prenatal examinations give very reliable results, but can trigger a miscarriage.
For some time now, non-invasive prenatal blood tests have also been available, with which trisomy 13 (as well as other chromosome abnormalities) can be reliably detected in the unborn child - without the risk of miscarriage. All that is needed is a maternal blood sample: it contains traces of children's DNA that can be examined for anomalies.
Examples of such blood tests are the Harmony test, PrenaTest and Panorama test. If there is a justified suspicion of trisomy 13 and after a medical consultation, the costs incurred for such a prenatal test can be covered by the statutory health insurance.
Postnatal examinations
After giving birth, it is first important to identify life-threatening malformations and developmental disorders that require immediate treatment. Therefore, a thorough examination of the newborn's organ systems is carried out. The prenatal examinations also help to assess the severity of trisomy 13. After the birth, the affected child usually needs intensive medical monitoring and treatment.
If a trisomy 13 has not already been determined during the preventive medical check-ups, the genetic test is carried out after the birth. All that is needed is a blood sample from the newborn, which can be obtained from an umbilical vessel, for example.
heart
The heart must be examined thoroughly as soon as possible after birth. With the help of a heart ultrasound (echocardiography) one can assess the malformations in the heart. Especially the partitions in the heart should be carefully considered. Serious heart diseases often manifest themselves as dangerous circulatory disorders that require intensive medical treatment.
Gastrointestinal tract
An ultrasound or X-ray examination of the abdomen may reveal a rotation of the internal organs, leading to their abnormal arrangement.
Nervous system
The nervous system should also be examined using magnetic resonance imaging (MRI) or computer tomography (CT). A conspicuous brain structure, such as that found in holoprosencephaly, can usually be recognized.
Skeletal system
Malformations on the skeleton are often only examined in more detail last, since in most cases they do not pose an acute threat to life. Bones can be shown well on X-rays.
Trisomy 13: treatment
There is currently no curative treatment for trisomy 13. The aim of all efforts is the best possible quality of life for the affected baby. Any treatment for trisomy-13 should be performed by an experienced, multidisciplinary team. This team includes gynecologists, paediatricians, surgeons and neurologists. In addition, palliative care professionals can make a very important contribution to the well-being and comfort of the child.
While malformations of the organs in the chest and abdomen are often treatable and operable, malformations of the central nervous system (especially in the brain) pose a major challenge. They are usually not treatable.
In general, the therapeutic measures depend on the severity of the various malformations. Treatment should always be planned individually. The various problems are discussed in detailed discussions and evaluated according to their urgency. The type and intensity of therapy are controversial in the literature.
Since the mortality from the disease is very high, treatment limits are often agreed with the parents. Ideally, however, this should be done gradually. For example, one discusses whether and which operation (e.g. on the heart) is currently being carried out for treatment or which one should be avoided in the interests of the child.
Accompanying the parents
It is also very important to accompany the parents. They should be offered help and support in a responsible and honest manner, for example from social workers or in the form of psychological support. If the parents initially feel overwhelmed and helpless, the crisis intervention officer can provide hope and orientation.
Trisomy 13: disease course and prognosis
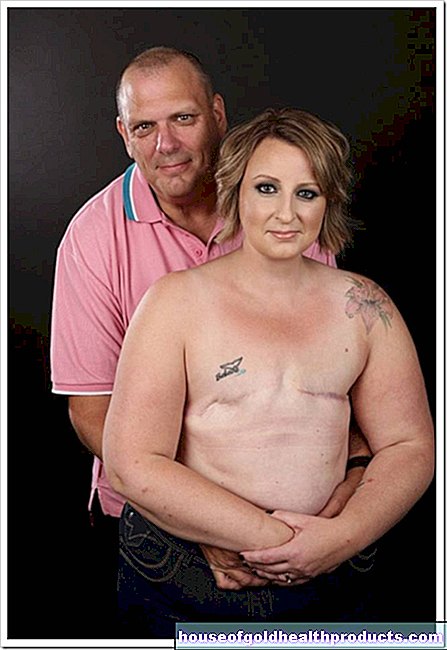
The Patau syndrome cannot be cured. Many of the trisomy 13 cases diagnosed prenatally die before birth, and many more in the first month of life. Only five percent of babies live to be older than 6 months. More than 90 percent of those affected die in the first year of life. However, it is difficult to predict how long a trisomy 13 baby will survive.
On average, the trisomy 13 life expectancy of a live born baby is 90 days after birth. This is mainly due to the fact that serious complications from the malformations usually occur immediately after birth. The most common life-threatening complications of trisomy 13 include breathing difficulties, heart defects, seizures, kidney failure, and feeding problems. Intensive therapy can possibly extend survival.
Longer survival is possible, especially if there are no major brain malformations. But even trisomy 13 children who survive the first year of life often show a large intellectual deficit, so that they usually cannot lead an independent life.
Even if there is still no cure, a large number of studies are being carried out to research healing options with the aim of finding a therapy for trisomy 13 one day.
Tags: gpp healthy feet tcm