Wound healing
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Wound healing is a very complex process. Their goal is to seal off damage in the body tissue in order to prevent infection, dehydration or other consequential damage. Read more about the wound healing phases and the difference between primary and secondary wound healing here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. T89T79T81
Why wound healing is important
Wound healing is a complicated process in which many different cells, messenger substances and other substances are involved. It aims to close a wound - i.e. a defective area in the tissue of the outer or inner surface of the body - as quickly as possible. This is to avoid infections, temperature fluctuations, dehydration and other mechanical irritation.
Phases of wound healing
There are roughly three phases of wound healing that can also overlap and run in parallel:
Exudation or cleansing phase
The exudation phase (also called the cleaning or inflammation phase) begins immediately after the wound has formed:
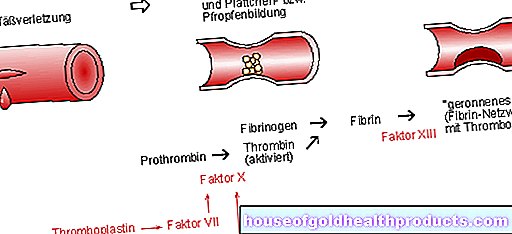
Any bleeding is stopped by vasoconstriction (constriction) and activation of the blood coagulation cascade (formation of fibrin = protein fibers). Damaged vessel walls are sealed. The release of messenger substances such as histamine triggers a local inflammatory reaction, as a result of which, among other things, the wall permeability of the finest blood vessels (capillaries) increases. As a result, increased blood plasma escapes in the wound area (exudation).
With this wound secretion (wound fluid) the body tries to clean the wound. It washes out cell debris, foreign bodies and bacteria. This process is supported by immigrated white blood cells of the macrophage type (phagocytes) and granulocytes:
Like macrophages, granulocytes eliminate germs. The phagocytes also break down cell debris.
The exudation phase usually lasts up to three days.
Granulation or proliferation phase
In this second phase of wound healing, the smallest blood vessels (capillaries) and connective tissue cells begin to grow into the wound bed from the wound edges and form a solid network. This vascular tissue is deep red, shiny and granular on the surface and is referred to as granulation tissue (Latin: granulum = grain).
The connective tissue cells produce collagen precursors. These stabilizing protein fibers cause the wound to shrink - the wound edges are drawn towards each other and the wound surface is reduced.
The granulation phase lasts about ten days.
Regeneration phase
In the last phase of wound healing, the proportion of tissue water and vessels in the granulation tissue decreases. The previously created collagen fibers network and stabilize. This is how the first scar tissue is formed. The epithelial cells that migrate from the wound margins finally cover the entire surface of the wound (epithelialization).
The regeneration phase can last for several weeks to months. Only after about three months has the scar reached its maximum resilience.
Primary and secondary wound healing
There are basically two ways in which wounds can heal: primary and secondary wound healing.
Primary wound healing
Doctors speak of primary wound healing when the wound edges grow together directly to form a narrow scar. This can happen on its own or with medical assistance (using sutures, staples or plasters). The initially light red, soft scar becomes whitish over time and becomes more firm.
Primary wound healing is found in uncomplicated occasional wounds (such as cuts and lacerations) with smooth wound edges and no major tissue loss. And then, if the wound is not older than four to six hours when it is closed. Wound healing after surgery also proceeds primarily if it is a non-infected (aseptic) surgical wound.
Secondary wound healing
Large and / or gaping wounds with greater tissue loss heal secondarily, i.e. the wound edges do not grow together directly, but the wound is filled from the bottom with granulation tissue. Such a secondary healing wound finally has a wider scar area, which is not very resistant to stress and can be cosmetically disruptive.
Any wound infected with bacteria should also heal secondarily to be on the safe side: if the wound is primarily closed by a skin suture, the germs in the wound can multiply and lead to a pus (abscess). In the case of an infected wound, open wound healing with granulation from the depths upwards is important so that wound exudate or pus can flow outwards unhindered.
Secondary wound healing also occurs in chronic wounds such as a diabetic foot ulcer or pressure ulcer (bedsores).
Tags: alcohol gpp teeth