Breast cancer: blood test checks the effectiveness of therapy
All content is checked by medical journalists.Around 70,000 women in Germany develop breast cancer every year. In most of the patients, cancer growth is promoted by hormones and can be combated with anti-hormone therapy. This is why many women spend years swallowing tablets that suppress natural hormone production. In some of them, the tumor becomes resistant and the drugs lose their effectiveness. In the future, a simple blood test should show whether this is the case. It can prevent women from receiving therapies that can cause significant side effects but do not help.
Effectiveness test with "liquid biopsy"
The test was developed by scientists from the Institute of Cancer Research in London. He checks which patients benefit from aromatase inhibitors.
Currently, the only way to test the benefit of anti-hormonal therapy is through a biopsy. The new blood test should offer an alternative to this. "Liquid biopsy" is what the researchers from the Institute of Cancer Research called it. It is far less stressful than a normal biopsy, but should be just as meaningful.
The effect of mutations fizzled out
The test looks at the genetic properties of tiny DNA particles of the cancer in the blood. In their study, the scientists examined the blood of 171 women with hormone-positive breast cancer who had already developed metastases. They came across certain changes: The so-called estrogen receptor gene (ESR1) mutations indicate that the cancer has become resistant to anti-hormone therapies, especially to aromatase inhibitors.
“With the help of liquid biopsies, the course of a treatment can be observed. This allows doctors to know when to switch therapy, ”says Nicholas Turner, head of the research team. The treatment can thus be tailored very specifically to individual patients.
Start anti-hormone therapy early
Whether a patient becomes resistant to anti-hormone therapy appears to be related to when treatment is started. Women who were treated with aromatase inhibitors before their cancer had spread later had fewer ESR1 mutations (six percent) than women who only received aromatase inhibitors after the cancer had spread (36 percent). "More advanced tumors therefore become resistant more quickly," say the researchers. "This confirms once again how important it is to discover and treat tumors at an early stage."
Tumor cells with an ESR1 mutation are more aggressive and spread faster, the researchers write. The risk of rapid disease progression increases due to the change in the genetic code of the cancer cells: in women with mutations, the disease progressed three times faster than in women whose cancer cells had not changed.
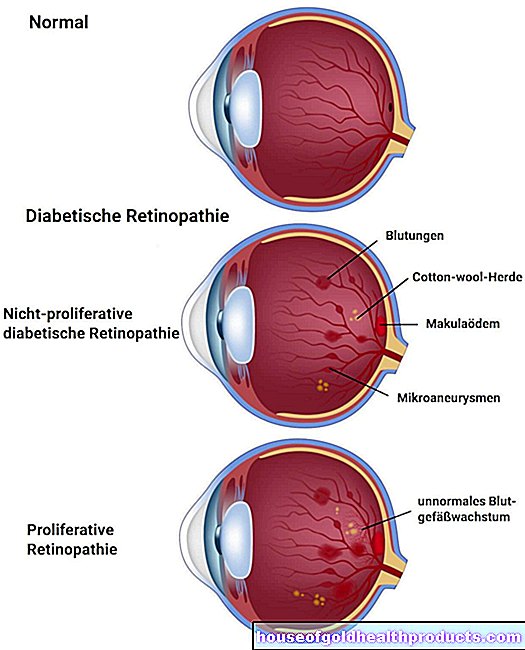
Blocked estrogen production
Estrogen promotes the growth of hormone-sensitive tumors. This can be prevented in two ways: First, by blocking the production of estrogen with the help of aromatase inhibitors. However, these only affect the production of estrogen in muscle and fat cells, but not that of the ovaries. Therefore, aromatase inhibitors are particularly useful for women who have already passed the menopause and whose ovaries no longer produce hormones. In younger women with active ovaries, active ingredients are therefore more likely to be used that block the effect of estrogen on the cancer cells themselves by occupying the docking sites of the hormones.
Breast cancer patients should take antihormonal drugs for at least five years, and according to more recent recommendations even up to ten years. But many stop the therapy early, mainly because they suffer from the side effects, including menopausal symptoms such as hot flashes but also muscle and bone pain. (vv)
Source: Schiavon. G. et al. Analysis of ESR1 mutation in circulating tumor DNA demonstrates evolution during therapy for metastatic breast cancer. Science Translational Medicine 11 Nov 2015: Vol. 7, Issue 313, pp. 313ra182. DOI: 10.1126 / scitranslmed.aac7551.
Tags: menopause anatomy therapies







.jpg)