Brain death: new guideline aims to allay fears
Christiane Fux studied journalism and psychology in Hamburg. The experienced medical editor has been writing magazine articles, news and factual texts on all conceivable health topics since 2001. In addition to her work for, Christiane Fux is also active in prose.Her first crime novel was published in 2012, and she also writes, designs and publishes her own crime plays.
More posts by Christiane Fux All content is checked by medical journalists.The German Medical Association has presented a new guideline on brain death diagnostics. It was last revised in 1997. The authors pay greater attention to the qualifications of doctors who diagnose brain death. With the guideline, the experts also want to counter possible fears and uncertainties when dealing with the sensitive topic.
Which doctors are qualified to assess brain death has now been more clearly defined. Accordingly, in addition to several years of experience in the intensive treatment of patients with acute severe brain damage, they must have appropriate specialist certification. What is also new is that at least one of the two doctors who must be consulted for the assessment must be a neurologist or neurosurgeon.
In addition, modern studies such as duplex sonography and CT angiography, which can confirm the irreversible functional failure of the brain, have included brain death diagnostics in the guideline.
Controversial term of death
The authors avoid the term brain death. Instead, they use the term “irreversible brain function failure”. “The colloquial term brain death has led to misunderstandings in the past,” says Professor Frank Ulrich Montgomery, President of the German Medical Association, explaining this decision in the German Medical Journal.
The most recent statement by the German Ethics Council shows how difficult it is to deal with the term brain death. Even there one could not agree on a common statement. While most members follow the medical definition, according to which brain death is actually equated with human death, a minority takes a different position: They are of the opinion that brain death is not a criterion for death because the organism (albeit with intensive care support) still has diverse functions such as heart function. However, it is undisputed in the Ethics Council that an irreversible loss of brain function is a sufficient prerequisite for the removal of organs.
Fear-ridden topic
Discussions arise again and again about the subject of brain death. A case in the Bremen area last caused a stir in December 2014. Organ removal for transplant purposes had already started, although the brain death diagnosis was not yet fully completed. Cases like this stir up fears in people who shy away from agreeing to an organ donation because they fear that they will hear something about the removal or even be declared dead prematurely.
"Our goal is to further strengthen trust in the directive-compliant death determination," says Montgomery in the German medical journal. To this end, doctors would have to explain in an understandable and comprehensible way what the irreversible brain dysfunction means in order to counter possible uncertainties and fears in this sensitive area of intensive care medicine. "Anyone who understands irreversible brain dysfunction as a sure sign of death can then make an informed decision about organ or tissue donation."
Strictly regulated procedure
The basic procedure for brain death diagnostics remains unchanged in the revised guideline. As before, two qualified doctors have to determine the brain death of the organ donor independently of each other. In brain death, all functions of the cerebrum, the cerebellum and the brain stem are extinguished.
If an organ removal is to take place afterwards, the assessing doctors must neither be involved in the removal of the organs nor in their transplantation or be subject to the instructions of a doctor involved in the transplantation.
Multiple examination
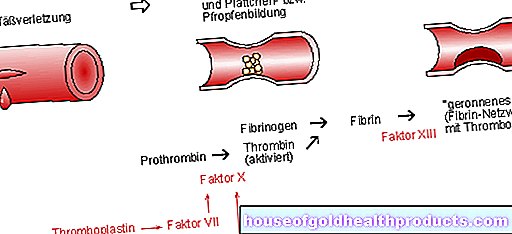
Before brain death can be diagnosed, doctors must rule out that the patient is not simply lying in a deep unconsciousness that has a remediable cause - for example, drugs or hypothermia. Brain death is determined when a number of specific reflexes, such as the pupil's lack of reaction to light, and when the respiratory reflex does not start when the ventilator is switched off. These examinations must be carried out again at certain intervals. Another option is tests that measure cerebral blood flow and activity. A clear sign of brain death is the complete lack of blood supply to the brain. (cf)