Calf cramps
and Martina Feichter, medical editor and biologist and Carola Felchner, science journalistIngrid Müller is a chemist and medical journalist. She was editor-in-chief of for twelve years. Since March 2014 she has been working as a freelance journalist and author for, among others, Focus Gesundheit, the health portal ellviva.de, the publishing house living crossmedia and the health channel of rtv.de.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts
Carola Felchner is a freelance writer in the medical department and a certified training and nutrition advisor. She worked for various specialist magazines and online portals before becoming a freelance journalist in 2015. Before starting her internship, she studied translation and interpreting in Kempten and Munich.
More about the experts All content is checked by medical journalists.Calf cramps occur when muscles or muscle parts of the calf suddenly and painfully contract without any deliberate influence. This can happen during exercise, for example, but also during sleep. Occasional muscle cramps in the calf are usually harmless. However, if the cramps occur more frequently, they can be signs of illness. Read everything you need to know about leg cramps here!

Brief overview
- Description: Calf cramps are sudden, short, involuntary, and painful contractions of a part, whole or group of muscles in the calf.
- Causes: mostly unknown or harmless (e.g. strong muscle tension during sport, excessive water and salt loss through sweating, etc.). More rarely, leg cramps are signs of an illness (e.g. underactive thyroid, diabetes, kidney weakness, varicose veins) or side effects of medication.
- Treatment: depending on the cause and need, e.g. replacement of missing fluids or electrolytes, treatment of underlying diseases
- What helps against cramps in acute cases? Stretching, gentle massage, heat applications
- Prevention: e.g. regular exercise, gentle stretching (before exercising and going to bed), drinking enough, magnesium-rich diet, possibly taking magnesium supplements, avoiding nicotine, caffeine and stimulants such as ephedrine
Leg cramps: description
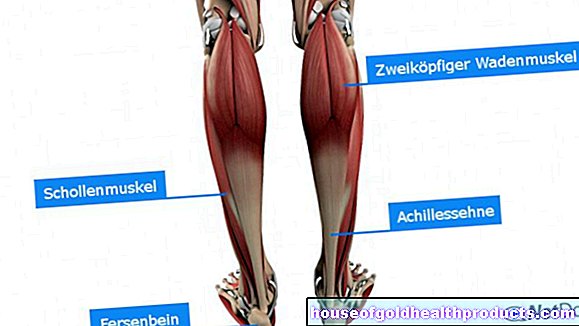
Calf cramps are cramps in the calf muscles. With such a muscle spasm, part of a muscle, an entire muscle or a muscle group suddenly, involuntarily and painfully contracts. The affected muscles are palpably hardened and unable to move. Muscle cramps only last for a short time (seconds to minutes) and then subside on their own.
Muscle spasms usually occur in the legs and here preferably in the calf. Leg cramps are therefore the most common and probably best-known form of muscle cramps.
Muscle spasms, i.e. painless cramps in the muscles, must be distinguished from muscle cramps. Fasciculations must also be distinguished - visible, irregular and involuntary twitching of muscle fiber bundles without any movement effect (e.g. twitching eyelid). They're not painful, but they are often uncomfortable.
Convulsions: frequency
Leg cramps and other muscle cramps occur especially at night and are not uncommon. Almost everyone has muscle cramps every now and then. Over 90 percent of young adults report isolated cramps. With age, muscle cramps become more common: 33 to 50 percent of people over 65 years of age have cramps regularly (at least once a week).
The increased susceptibility to muscle cramps in old age can be explained by generally shortened muscles. In addition, older people tend to drink too little - this can imbalance the water and mineral balance and thus promote cramps (e.g. in the legs).
Leg cramps: causes
Basically, calf cramps and other muscle cramps are divided into three categories by doctors, depending on how they develop:
- Paraphysiological cramps: Occasional cramps during pregnancy and after physical exertion, which are usually caused by a disruption in the electrolyte and water balance - for example as a result of profuse sweating.
- Idiopathic convulsions: They happen for no apparent reason and no cause can be determined. Often there are nocturnal cramps in the legs.
- Symptomatic cramps: They are an accompanying symptom of diseases, such as disorders in the nervous system, muscles or metabolism. Medication can also cause muscle cramps (such as calf cramps) as a side effect.
Leg cramp mostly harmless
The occasional cramp in the calf is generally not a cause for concern - it is usually idiopathic or paraphysiological. The latter can be triggered, for example, by a lack of fluid intake, strenuous exercise or a common gastrointestinal flu with severe diarrhea. Strong muscle tension (such as when exercising) can also result in calf cramps.
More rarely, leg cramps are the symptom of a serious illness (e.g. hormonal or metabolic diseases, vascular diseases, kidney diseases) or a side effect of medication.
Below you will find more detailed information on possible causes of calf and other muscle cramps.
Disorders of the electrolyte and water balance
Dehydration
Often, calf cramps or muscle cramps are triggered by dehydration, i.e. dehydration of the body. The result is an imbalance in the mineral balance that can trigger muscle cramps.
For example, dehydration can result from severe diarrhea, violent vomiting, or profuse sweating and insufficient fluid intake. Sometimes, however, the cause is also a serious illness such as diabetes insipidus (a hormonal disorder with extremely high urine output) or inflammatory bowel disease, Crohn's disease. Diuretics (water medication) can also lead to a large loss of water from the body and thus trigger a muscle spasm (in the leg or elsewhere).
Magnesium deficiency
A magnesium deficiency (hypomagnesaemia) can also cause calf cramps or muscle cramps. An undersupply of the mineral can result from an unbalanced diet or diet, from diabetes mellitus, alcoholism or intestinal and kidney diseases. A deficiency often develops during pregnancy as well - there is then an increased need for magnesium.
Leg cramps and other muscle cramps in connection with other symptoms of magnesium deficiency (such as confusion, weakness, tiredness, headache and cold feet) are collectively referred to as magnesium deficiency syndrome.
Other electrolyte imbalances
Potassium deficiency (hypokalaemia) and calcium deficiency (hypocalcemia) are also possible causes of muscle cramps:
A deficiency in potassium can result, for example, from severe diarrhea, the use of certain medications, a magnesium deficiency or diseases of the adrenal glands (see below). An undersupply of calcium can be caused by a magnesium or vitamin D deficiency, disorders of the parathyroid gland or kidneys (see below) or certain medications.
Disorders of the hormonal balance and metabolism
Various hormonal and metabolic disorders can cause symptomatic muscle spasms if they disrupt the water and electrolyte balance. Examples:
- Underactive thyroid: Common signs of an underactive thyroid (hypothyroidism) include poor performance and concentration, easy fatigue and memory disorders. In addition, the muscles tend to cramp.
- Underactive parathyroid gland (hypoparathyroidism): It causes a calcium deficiency, which makes the muscles overexcitable. Among other things, this can trigger muscle cramps and, in severe cases, even tetany (rigid, persistent cramps) in the hands and feet.
- Diabetes mellitus: The first symptoms are increased urination and a strong feeling of thirst. Muscle cramps (such as calf cramps) can initially be caused by electrolyte imbalances, later they can be the result of diabetic nerve damage (polyneuropathy).
- Adrenal cortical disorders: The adrenal gland secretes hormones that are essential for regulating the water and mineral balance. Diseases of this organ can therefore make themselves felt, among other things, with muscle spasms.
- Kidney diseases: The kidneys play the central role in regulating the fluid balance. Kidney weakness or even kidney failure can therefore trigger cramps, among other things.
Musculoskeletal disorders
Every now and then, symptomatic muscle cramps are the result of muscle diseases (myopathies). These rare diseases can be congenital or acquired and are typically associated with muscle weakness. Sometimes cramp-like muscle pain also occurs.
Structural disorders are also possible triggers for muscle cramps. With flat feet, for example, the uneven strain on the foot muscles can lead to foot cramps. A genu recurvatum - an abnormally hyperextensible knee joint - sometimes causes muscle cramps in the leg.
Nerve disorders
Neurological disorders and diseases that can be associated with symptomatic muscle spasms include:
- Motor neuron diseases: These are diseases in which nerve cells that stimulate muscle movements are progressively destroyed. The most common form is amyotrophic lateral sclerosis. Its symptoms include muscle weakness, muscle wasting, and muscle cramps.
- Peripheral neuropathies: These are diseases in which peripheral nerves (such as leg nerves) are damaged, which can cause muscle spasms. The diseases can affect only one or a few nerves, but sometimes many. In the latter case one speaks of polyneuropathy. It is often caused by diabetes or alcoholism.
- Radiculopathies: These are diseases of the nerve roots (in the area of the spine), triggered for example by a herniated disc. For example, nerves that control the leg muscles can be affected, which can result in muscle cramps (such as calf cramps).
Vascular disease
Varicose veins (varices) are enlargements of superficial veins caused by weak veins. They often form on the legs and are visible here as blue, thick, knotty blood vessels. The legs feel heavy and tense. In addition, nocturnal calf cramps occur more frequently.
Drugs and stimulants
There are a number of drugs that can cause cramps in the muscles. These include:
- certain high blood pressure medicines: angiotensin II receptor blockers (AT1 antagonists) and some beta blockers
- bronchodilators used to treat asthma, e.g. salbutamol
- Cisplatin and vincristine (cancer drugs)
- Clofibrate and lovastatin (medicines for high blood lipid levels)
- Diuretics (water tablets)
- Donepezil (anti-Alzheimer's)
- Tolcapone (anti-Parkinson's)
- Contraceptive pill ("contraceptive pill")
- Pyrazinamide (anti-tuberculosis drug)
- Raloxifene (used to prevent and treat osteoporosis)
- Teriparatide (used to treat osteoporosis)
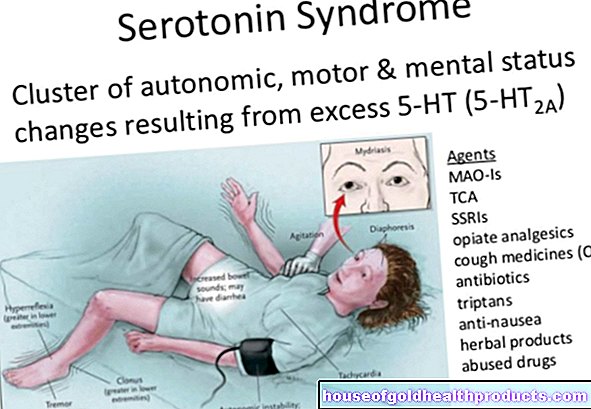
Various stimulants (such as amphetamines, cocaine, caffeine, nicotine, ephedrine, and pseudoephedrine) can also cause muscle spasms.
Leg cramps: treatment and first aid
Treatment for calf cramps (and other muscle spasms) depends on the cause. Some examples:
Disturbances in the electrolyte and water balance can often be compensated for if the person concerned drinks more and has a balanced diet. This is especially true if the disorder is not caused by the illness, but is caused by profuse sweating during exercise. If there is a strong imbalance in the water-salt balance (e.g. as a result of severe vomiting and diarrhea), special electrolyte solutions can be useful. They contain the most important mineral salts in an optimal composition and can quickly and effectively compensate for the loss of water and salt.
If an illness causes cramps in the calves or other muscles (via disturbances in the water-salt balance or in some other way), it is important to treat them appropriately. For example, if the thyroid is underactive, the doctor will prescribe a hormone preparation to replace the missing thyroid hormones. If the parathyroid gland is underactive (hypoparathyroidism), those affected receive vitamin D and calcium. This compensates for the calcium deficiency and can help against muscle cramps.
If cramps are a drug side effect, the doctor will prescribe an alternative drug if possible.
Quinine used to be used to treat muscle cramps (such as calf cramps). However, due to the side effects (such as vomiting, visual disturbances, ringing in the ears, headache), it is not recommended today. Mexiletine (a remedy for cardiac arrhythmias) would also be effective against cramps. But it also has many side effects (nausea, vomiting, tremors = tremor and seizures).
First aid for acute muscle spasms
>> stretching
In acute cases (e.g. muscle cramps during exercise or nocturnal calf cramps) it usually helps to stretch the painful, cramping muscles - this can often end the cramp.
For example, if you have a leg cramp while standing, pull the toes of the affected leg towards your nose (possibly with the help of your hand) while simultaneously pressing your heel into the ground. The whole thing also works when lying down - pull your toes towards your shin and push your heel away at the same time. This stretching of the calf muscles also stretches the back of the thigh - so this exercise also helps if you have a cramp in your back thigh.
If, on the other hand, you have a cramp in your thigh at the front, stretching works as follows: Stand upright, grasp the foot of the leg in question and pull it towards your buttocks - until you feel the stretch on the front of the thigh. If this one-legged stand is too shaky for you, you can hold on to the wall or a chair with your other hand.
>> Gentle massage
In addition to stretching, gentle massaging can also help with muscle cramps, ideally with a warm, damp towel. This loosens the cramped muscles and increases the local blood flow. This allows the muscle to relax better.
>> warmth
Warm wraps and hot baths also have a relaxing effect on cramped muscles - or you can put a hot water bottle on the aching muscles.
By the way: conventional pain relievers such as acetylsalicylic acid (ASA) or paracetamol do not help against muscle cramps.
Leg cramps: when to see a doctor?
Leg cramps and other muscle cramps that only occur occasionally are usually harmless. But be sure to see a doctor if the painful cramps
- occur more often
- Disturb the night's rest or daily routine,
- does not go away by itself or by stretching and gentle massage and / or
- are accompanied by other symptoms such as nausea, numbness, tingling or restricted mobility.
Your first point of contact in such cases is your family doctor. If necessary, he can refer you to a specialist.
Leg cramps: examinations & diagnosis
In order to uncover the cause of calf cramps (or muscle cramps in general), a detailed discussion between you and the doctor is first necessary to collect the medical history (anamnesis). Frequently asked questions are, for example:
- Where do the cramps occur?
- When and how often do you have the cramps?
- Approximately how long does a single cramp last?
- Are there certain situations or events that may trigger your cramps?
- Do you have any other symptoms (e.g. muscle weakness, numbness, diarrhea, sensitivity to cold, weight gain, etc.)?
- How about your alcohol consumption?
- Are you using any medication? If yes, which?
- Do you have any previous illnesses?
Physical and neurological examination
A physical exam will give the doctor clues about your general health. He can feel under muscles and joints and test the muscle reflexes. He also pays attention to abnormalities that may indicate the cause of the muscle spasms (e.g. dry skin and mucous membranes as well as standing skin folds in the case of dehydration or a swollen face, dull hair and hair loss in the case of hypothyroidism).
If necessary, a neurological examination is also useful. The examination methods often used to clarify muscle spasms include, for example:
- Measurement of electrical muscle activity (electromyography): This is how you can check whether a muscle disease or nerve disorder is present.
- Measurement of nerve conductivity (electroneurography): This allows the doctor to test the functionality of peripheral nerves and identify possible nerve damage.
Further investigations
For example, blood tests may show a lack or excess of electrolytes such as magnesium, calcium, or sodium. The kidney values provide information about possible diseases of the organ. An impaired thyroid function that causes muscle spasms can be recognized by the corresponding hormonal changes in the blood.
Sometimes imaging tests are also needed to get to the bottom of cramps and their possible causes. Ultrasound can be used to assess the condition of the kidneys and thyroid, for example. Doppler sonography (a special form of ultrasound) is used to clarify varicose veins more precisely. If nerve root damage (radiculopathy) is suspected, e.g. due to a herniated disc, computed tomography (CT) or magnetic resonance imaging (magnetic resonance imaging, MRI) can provide clarity.
In some cases, a muscle biopsy is also needed to confirm or rule out a (suspected) cause of muscle spasms. This is necessary for amyotrophic lateral sclerosis, for example.
Delineation of other disorders
What the doctor must consider during his examinations: A distinction must be made between systemic muscle spasms and painful muscle contractions of a different origin as well as symptoms that are similar to muscle spasms. These include, for example:
- Dystonias: These are involuntary muscle contractions that generally last longer than normal muscle spasms and often affect other muscles - such as the muscles of the vocal cords (spasmodic dysphonia), the eyelids (blepharospasm), the muscles of the neck (torticollis) or the muscles of the hands ("writer's cramp") . Sometimes dystonia occurs as part of conditions like Parkinson's or Huntington's disease.
- Tetany: The term refers to the uninterrupted or periodic cramping of muscles throughout the body. So these cramps are much more extensive and last longer than normal muscle cramps. They are also often accompanied by repeated brief muscle twitches. Tetany triggers include rickets, chronic kidney disease, pancreatitis, traumatic brain injury and vomiting. Sometimes the cause of a tetany remains unknown (idiopathic tetany).
- Tetanus: This is an infectious disease with certain bacteria, the toxins of which trigger strong, persistent muscle cramps, for example in the face (blocked mouth, "devil's grin") and back. If left untreated, tetanus is fatal.
- Stiff-Man-Syndrome (Stiff-Person-Syndrome): This is a rare neurological disorder that is associated with slowly increasing muscle stiffness in the trunk and limbs and painful spasms.
- Strychnine poisoning: The highly toxic substance was previously used as a stimulant (analeptic) and rat poison. Typical symptoms of poisoning are extension cramps, i.e. long-lasting, rigid (tonic) cramps, especially of the extensor muscles. Death usually occurs through respiratory paralysis.
- Muscular ischemia: Patients with a "smoker's leg" (peripheral arterial occlusive disease, PAOD) can experience calf pain during physical exertion because the calf muscles are not supplied with enough blood (reduced blood flow = ischemia). This can feel like a calf cramp, but it's not (no muscle contraction!).
- Illusory muscle spasm: This is what doctors speak of when someone has the feeling of a muscle spasm, but neither muscle contraction nor muscular ischemia is present.
Leg cramps: prevention
The following tips can usually prevent occasional calf cramps (and other muscle cramps), such as those caused by exercise or a lack of fluids and electrolytes:
- Regular exercise: Regular exercise in connection with stretching exercises (see below) helps to keep the muscles well supplied with blood and healthy. This can prevent cramps. However, make sure that you exercise appropriately - if you overdo it, you will experience cramps in the calves and other cramps in the skeletal muscles.
- Gentle stretching: Gently stretching before exercise and before going to bed makes muscles and tendons more flexible. This reduces the likelihood that they will involuntarily contract (during or after training or while sleeping).
- Do not exercise after eating: You should not exercise immediately after eating.
- Drink enough: Those who drink enough (alcohol-free!) prevent disturbances of the water-salt balance and thus muscle cramps. This is particularly important if you sweat heavily, for example during sports. You can compensate for the water and salt loss with isotonic drinks (e.g. an apple juice spritzer with a pinch of salt or a non-alcoholic beer). Passionate athletes also like to use special sports drinks.
- Avoid caffeine and nicotine
- Avoiding stimulants: If possible, you should also avoid stimulants such as ephedrine and pseudoephedrine (contained in cold decongestants, for example).
- Magnesium: So far, there is no scientific evidence that taking a magnesium preparation can prevent calf cramps (or muscle cramps). In the right dosage, however, at least there is no harm in taking it. In any case, you should pay attention to a diet rich in magnesium (e.g. bananas, nuts, whole grain products).
- Correct footwear: Sometimes incorrect footwear (e.g. high-heeled pumps) or a misaligned foot such as splayfoot or flat foot is the reason for muscle cramps (e.g. foot cramps or calf cramps). Then the right shoes and, if necessary, insoles help.