amputation
All content is checked by medical journalists.An amputation is the separation of a part of the body. This can happen in the event of an accident or during an operation. For example, severe blood vessel diseases in which the tissue is no longer adequately supplied with blood often require amputation. Read all about the surgical procedure, when it is performed, and the risks involved.

What is an amputation?
In an amputation, a part of the body is cut off either surgically or through an accident. If there is still a connection between the severed body part, the so-called amputate, and the body through tissue such as skin or muscles, this is known as subtotal amputation. On the other hand, there is total amputation, i.e. complete severing.
When do you perform an amputation?
Surgical amputation always takes place when body tissue has been irreparably damaged or has already died. Because dead tissue on the living body - also known as necrosis or gangrene - carries a high risk of infections that can spread further in the body via the blood. To prevent this life-threatening complication, the affected tissue is removed.
If only a small area is affected by the necrosis, the doctor may be able to cut it out. If it is more advanced, however, usually only an amputation will help. You always cut off as little as possible. Other reasons for amputations are accidents and cancer.
Amputation in vascular diseases
In Germany, disorders of the arterial blood flow are the most common reason for amputations. If tissue is not supplied with enough blood, the cells do not receive enough oxygen and die. This can be caused by what is known as peripheral arterial occlusive disease (PAD), in which the arteries in the legs in particular “calcify”. PAD can occur alone or as a late sequela of diabetes (diabetes mellitus). It is true that doctors first try to improve blood flow through vascular surgery operations. But that often only delays an amputation.
Amputation for diabetes
In the long run, diabetes mellitus not only damages small and large blood vessels, but also the nerves. That is why people with diabetes often perceive sensory stimuli such as pain, temperature or pressure much weaker than healthy people.
For example, if a person with diabetes injures his foot, he does not feel any pain and therefore does not seek a doctor who could treat the wound. This can lead to necrosis and infections in the area of the injury, which in severe cases can only be contained by amputation.
Amputation in cancer
Malignant bone cancer also sometimes requires amputation. The thighs, lower legs and upper arms are particularly often affected here. The aim is to prevent malignant cancer cells from spreading to other parts of the body. The loss of function due to the amputation is accepted due to the better chances of survival.
Soft tissue tumors can also make amputation necessary. For example, a penile amputation is the last therapeutic option for certain types of cancer, even if this is associated with great psychological stress.
Amputation in the event of an accident
Extremities are often severely injured, especially in traffic accidents or accidents at work with agricultural or industrial machines. It may then no longer be possible to sew the severed vessels and nerves together. In such cases, the surgeon opts for an amputation. The lower legs and forearms are particularly often affected.
What do you do with an amputation?
In the run-up to the amputation, the doctors plan exactly at which point the body part is to be severed. Various imaging methods are available for this, for example computed tomography (CT). In addition, the blood flow to the tissue is checked with an ultrasound device. These examinations prevent dead tissue from developing again on the stump after the operation.
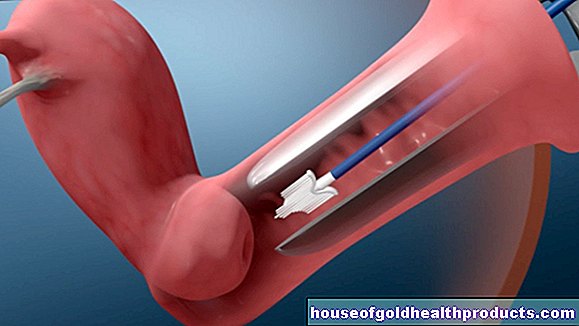
After the patient has been put under general anesthesia, the actual amputation begins. Leg, arm or other affected body parts are additionally anesthetized locally by the anesthetist. This makes pain management easier, especially after the operation, and phantom pain then occurs less often. During the operation, the doctor uses pressure cuffs to cut off the blood supply to the amputation area in order to keep blood loss as low as possible.
Amputation on the foot
With regard to the foot, a distinction is made:
- Minor amputation: "small amputation"; only parts of the forefoot (metatarsal bones and toes) will be removed.
- Major amputation: Any higher amputation.
In the case of amputations in the area of the foot, doctors try to remove as little bone as possible so that the patient can still stand and walk well after the operation.
The smallest possible amputation is one or more toes. Often, however, this is not enough because necrosis, for example, has already progressed too far. Then you have to amputate at a higher point, for example in the area of the metatarsal bones (transmetatarsal amputation).
Other options are the so-called Lisfranc and Chopart amputations, in which only the tarsus or heel bones remain. Here, the standing stability after the operation is already significantly limited.
Amputation on the leg
In the case of an amputation on the lower leg, the surgeon leaves a stump about ten centimeters long below the knee if possible. A prosthesis can be attached to this later. But that is not always possible. If the entire lower leg has to be removed below the knee, doctors speak of so-called disarticulation. Because the knee joint is then no longer functional, the patients are significantly more restricted in their movement.
In the case of amputations on the thigh, the bone can in principle be separated at any height. However, since a lot of muscles attach to the bone, one tries to make the cut as deep as possible, i.e. close to the knee. This provides the greatest possible mobility on the thigh stump.
As part of a hip disarticulation, doctors remove the entire leg and only the hip socket in the pelvis remains. If that is not enough due to the severity of an illness or injury, the bony pelvic areas on one side are also removed. Doctors call this type of amputation hemipelvectomy.
Amputation on the arm
In the case of amputations in the hand area, the main goal is to maintain the gripping function. For example, if the fingers need to be removed, there is an option to split the remaining metacarpal.This allows patients to continue to grip objects, even if this requires a lot of training.
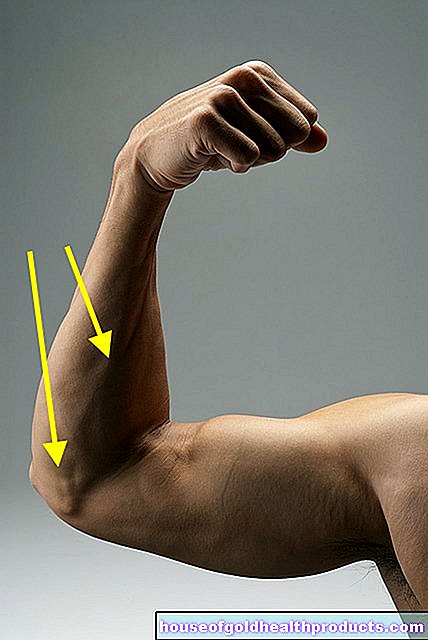
A similar operation is possible on the forearm. After this has been amputated, the surgeons separate the ulna and radius, which then lie next to each other like two fingers. This also enables the patient to grasp things.
If an amputation is required in the area of the elbow, upper arm or shoulder, it is important to preserve as much musculature as possible so that the patient can move the residual limb later. In addition, the surgeon creates a pear-shaped stump because a prosthesis holds better to it.
Sewing up the stump
After the doctor has removed the bone and associated soft tissue, he rounds off the bone stump. This prevents sharp edges from damaging the surrounding tissue. Finally, a flap of skin is placed over the stump and sewn to prevent germs from entering the wound.
What are the risks of an amputation?
As with any operation, amputation also carries general and specific risks:
- Infection of the wound
- Wound healing disorders
- Bleeding in the area of the stump
Later complications after an amputation include:
- Pressure sores in the area of the residual limb due to incorrect prosthesis settings
- Posture damage due to the changed stance and gait pattern of the patient
- Phantom pain
If the wound becomes infected and / or does not heal properly after the amputation, another operation may be necessary.
Phantom pain
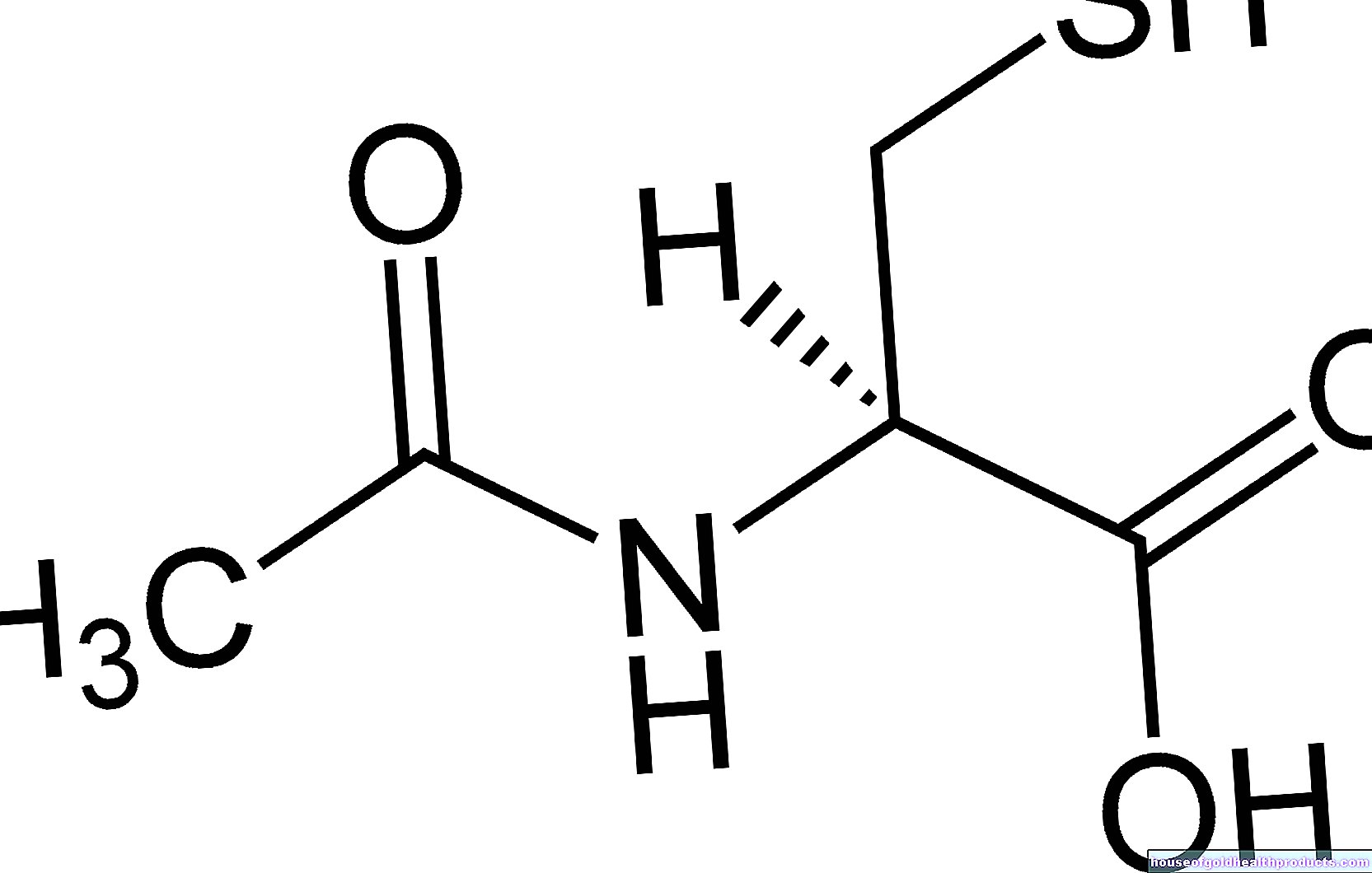
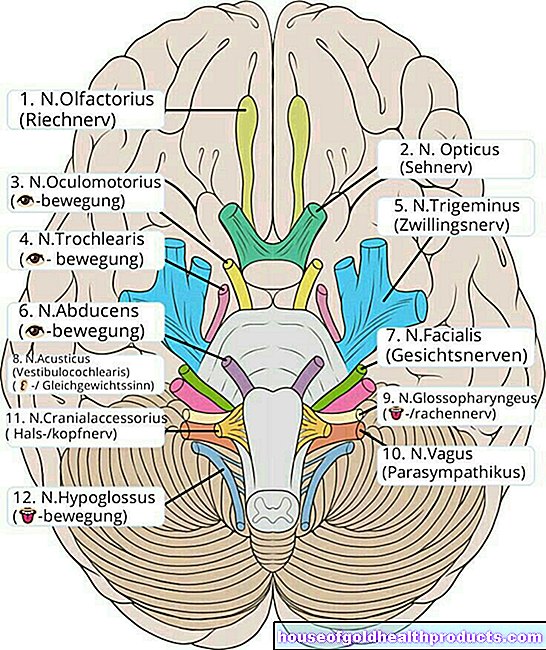
Many patients have so-called phantom pain after an amputation. They feel pain in the area of the body part that has been removed. For example, foot pain after a lower leg amputation. But other abnormal sensations such as warmth, cold or itching are also possible. That sounds paradoxical and can only be understood if you know how the brain processes the body's nerve signals.
There is a corresponding image in the brain for each area of the body. There the sensation of associated sensory stimuli are processed. For example, if you hit your right thumb with a hammer, the pain signal is first transmitted to the brain via nerves. There, the area reserved for the right thumb processes the signal and it becomes a conscious sensation, in this case pain.
After an amputation, the severed body part is no longer there, but the brain area that was responsible for processing its nerve signals is. If this brain area is now activated, the patient can experience sensations from the amputated part of the body.
How exactly such an activation occurs and why these sensations are often pain has not yet been clearly clarified. But because we have now better understood how phantom pain arises, it can be treated much better with the help of special techniques than a few years ago.
What do I have to consider after an amputation?
For many patients, the loss of a body part after an amputation is very stressful. If you are affected, you have the opportunity to talk to specialized psychologists about it after the operation.
In addition to doctors and psychologists, physiotherapists, occupational therapists and orthopedic technicians are also involved in further aftercare. These professionals will help you find your way in life again. For example, they will train you to use the new prosthesis in a rehabilitation clinic. Although this therapy is very strenuous, it is important that you continue to practice to get used to the prosthesis.
Also, pay attention to the wound on the stump after the operation. If you notice bleeding, swelling, redness or a too tight, painful wrap of the bandage, inform your surgeon immediately. Even if you have severe pain after the amputation, you must consult a doctor quickly so that he can treat possible complications.
Tags: nourishment diet pregnancy birth