Resuscitation in adults
Carola Felchner is a freelance writer in the medical department and a certified training and nutrition advisor. She worked for various specialist magazines and online portals before becoming a freelance journalist in 2015. Before starting her internship, she studied translation and interpreting in Kempten and Munich.
More about the experts All content is checked by medical journalists.Resuscitation is the resuscitation of a person after respiratory and circulatory arrest. To do this, chest compressions, ventilation and other measures to support the circulatory system are carried out. Doctors also speak of cardiopulmonary resuscitation (CPR) or cardiopulmonary resuscitation. Read here how to proceed and what you should pay attention to!

Brief overview
- What does resuscitation mean? Resuscitation measures in the event of respiratory and cardiovascular arrest.
- Procedure: Check whether the patient is reacting and breathing, making an emergency call, performing chest compressions and ventilation until the rescue service arrives or the patient is breathing again himself.
- In what cases? Resuscitation always takes place when vital organs are not adequately supplied with oxygen, e.g. B. in cardiac arrest or in the case of insufficient pumping capacity of the heart.
- Risks: Broken ribs and injury to internal organs (such as the spleen) during chest compressions, air and blood influx between the pleura and pleura, (low) risk of infection for the first aider (through mouth-to-mouth resuscitation of a patient with an infectious disease).
Caution!
- In an emergency, do not hesitate to start chest compressions (with enough pressure on the person's chest) - it can be life-saving!
- The affected person can choke on vomit or on their own tongue. Therefore, check whether the (upper) airways are free: stretch your head backwards, lift your chin and pull it forward, remove foreign objects from your mouth and throat if possible.
- The physical strain of resuscitation can injure you as a first aider. There is a certain risk of contagion with resuscitation if the patient is infected.
How does resuscitation work?
Resuscitation essentially consists of chest compressions and resuscitation. It is designed to ensure the oxygen supply to the brain and other organs when someone has suffered a respiratory / cardiovascular arrest. Speed is of the essence - a lack of oxygen in the brain can cause irreversible damage and death after just three minutes.
When it comes to resuscitation, experts differentiate between the basic measures of resuscitation and the extended measures:
Basic measures of resuscitation
The basic measures are summarized under the term “basic life support” (BLS for short). They can and should also be carried out by laypeople. It includes:
- Talk to the patient and check his or her response
- Check breathing
- Call the emergency
- Chest compressions
- Resuscitation
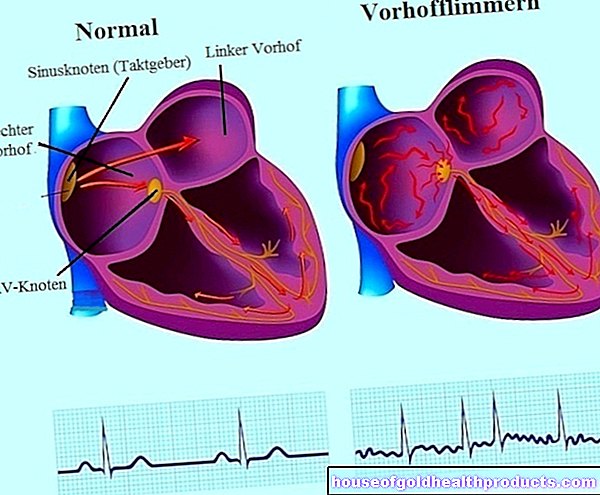
- if available: use an automated external defibrillator (AED) (defibrillation attempts to end life-threatening cardiac arrhythmias with the help of electrical impulses and restore a normal heart rhythm)
With the help of these measures, even as a layperson, you can ensure that the heart and brain of the person concerned are adequately supplied with blood until the emergency doctor arrives.
Advanced measures
The extended resuscitation measures ("advanced life support", or ALS for short) are carried out by medically trained personnel, such as paramedics. These try to animate the patient's heart to a normal beating rhythm again. This is done through defibrillation and medication.
In addition, the airways are secured and venous access is established. During this time, the basic resuscitation measures (cardiac pressure massage and ventilation) are carried out continuously.
Resuscitation: That's how it works
Anyone who finds a motionless person should, to the best of their knowledge, immediately provide first aid and resuscitation (as long as they do not endanger themselves).
1. Check awareness and breathing
As a first responder, you should first check whether the unconscious person responds to shaking or speaking loudly. Then check your breathing. To do this, stretch the patient's head back slightly and lift his chin. Look for foreign objects in the mouth and throat that could impede breathing. Remove them if possible.
Hold your ear close to the unconscious person's mouth and nose, facing towards the chest. Check to see if you can hear breath sounds, feel a breath of air, and see if the patient's chest rises and falls.
2. Alert the emergency doctor
Call the emergency doctor (phone: 112) or ask bystanders to do so.
3. Chest compressions
Then start immediately with chest compressions, the core of resuscitation. It ensures that, despite respiratory and cardiovascular arrest, the oxygen-saturated blood in the body is transported on to the cells (especially in the brain). How to perform chest compressions:
- Lay the motionless person flat on a hard surface and expose their upper body.
- Kneeling to the side, place the heel of your hand on the middle of the breastbone, place the second hand on the first and interlace your fingers.
- So that the chest is compressed sufficiently deeply, bend vertically over the chest (your shoulders should be perpendicular over your hands) and press firmly on the chest with your arms straight. The frequency should be at least 100 impacts per minute. You can also increase the chest compressions rhythm (up to a maximum of 120). Since “100” is a very abstract value, the following tip helps to find the right rhythm: Think of the song “Stayin’ Alive ”by the Bee Gees - its rhythm is ideal for chest compressions. The same goes for the song "Rock Your Body" by Justin Timberlake.
- After 30 compressions, there is twice a donation of breath, i.e. mouth-to-mouth or mouth-to-nose resuscitation.
- Continue this 30: 2 cycle until help arrives. If another first aider is present, it makes sense to change after every 30: 2 cycle (the chest compressions are exhausting!).
- If you do not trust yourself to ventilate (and no bystanders either), limit yourself to chest compressions and continue doing it continuously - until the emergency doctor arrives or the patient is breathing normally again.
- Use an automated external defibrillator (AED) if available. Such devices are now available at many central locations and in public buildings. Voice instructions help with correct application. Caution: The use of an automated external defibrillator must never delay or replace chest compressions!
As soon as the ambulance service arrives, they will try to restore the patient to a natural heart rhythm. The patient is intubated to secure the airway. That means: You push a thin tube (tube) through your mouth or nose and into your windpipe. In addition, a venous access is established, through which the patient is given fluids and medication. Often, for example, adrenaline (raises and supports blood pressure) and anti-arrhythmic drugs (antiarrhythmics) are given. In addition, an EKG is written to check cardiac activity.
Resuscitation in children
There are a few things to consider when resuscitating babies and toddlers in particular. You can find out more about this in the article Resuscitation in Children.
When do I do a resuscitation?
Cardiopulmonary resuscitation is always necessary if, in an acute emergency, vital organs or organ systems of an affected person are not adequately supplied with oxygen. The reason for this is usually cardiac arrest or insufficient pumping of the heart muscle, for example in the event of a heart attack, cardiac arrhythmia or pericardial tamponade (fluid accumulation in the pericardium that compresses the heart).
External influences such as suffocation, poisoning or drowning can also lead to cardiac arrest.
Typical symptoms of a lack of oxygen supply are unconsciousness, respiratory arrest or gasping (uncontrolled diaphragmatic twitching) and a missing or too fast heartbeat.
Risks of resuscitation
Resuscitation carries the following risks for the person concerned:
- Broken ribs
- Lung injuries
- Tears in the diaphragm, liver, or spleen
- Inhalation of stomach contents
- Entry of air into the pleural space (pneumothorax)
- Entry of blood into the pleural space (hemothorax)
- Entry of blood into the space between the heart and pericardium (hematopericardium)
There are also certain risks for first aiders: if they breath breath to a patient with an infection, there is a (low) risk of infection. In addition, chest compressions can be exhausting; the first aider may even injure himself.
Despite these potential risks for the patient and for you as the first aider, you should not shy away from resuscitation in an emergency - the life of the person concerned may depend on you!
Tags: baby toddler tcm skin care







.jpg)