Anal prolapse
Fabian Dupont is a freelance writer in the medical department. The human medicine specialist is already doing scientific work in Belgium, Spain, Rwanda, the USA, Great Britain, South Africa, New Zealand and Switzerland, among others. The focus of his doctoral thesis was tropical neurology, but his special interest is international public health and the comprehensible communication of medical facts.
More about the experts All content is checked by medical journalists.With anal prolapse, the anal canal falls out of the anus. Often, as part of anal prolapse, unwanted stool loss (incontinence) occurs. Older people, especially women, are particularly affected. If other parts of the intestine fall out, one speaks of a rectal prolapse (rectal prolapse). You can find out more about anal prolapse here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. K62

Anal prolapse: description
Anal prolapse usually takes place in stages. At first there is only one prolapse of the anal canal during heavy pressing on the toilet. After a bowel movement, the anal canal is withdrawn. In the further course, coughing or heavy lifting will lead to an incident at the anus.
If the anal prolapse is not treated, the anal canal will hang out continuously after a while. The disease can also progress further, so that not only the anal canal, but even parts of the rectum and rectum protrude from the anus. One then speaks of a so-called rectal prolapse or rectal prolapse.
From a medical point of view, this is a visual diagnosis: If only a few skin wrinkles have emerged from the anus, it is an anal prolapse. If, however, more can be seen and entire bulges of the mucous membrane have fallen, it is a prolapse of the rectum. In the latter case, as a rule, the anus is no longer able to close and defecation can no longer be controlled.
The earlier an anal prolapse is identified and treated, the better the chances of recovery and the lower the possible risks. Anal prolapse is rarely life-threatening, but it often severely restricts the quality of life.
While anal prolapse can occur at any age, it is more common in the elderly. Usually weak pelvic floor muscles are responsible. But anal prolapse can also be a sign of other diseases. In any case, anal prolapse must be treated by a doctor, as it does not heal on its own.
Anal prolapse symptoms
Anal prolapse differs in its symptoms from other diseases of the anus. As a rule, there is no pain, or only slight pain. In contrast, hemorrhoids or anal fissures are often reported to be much more painful. That is why the pain intensity is often an important characteristic in the patient consultation. Those affected are more likely to complain about the large mass on the anus and the incontinence and sometimes itching.
Incontinence varies in severity depending on the extent of the prolapse. In anal prolapse, it is usually not as pronounced as in rectal prolapse. In addition, the exposed intestinal mucosa is constantly producing fluid, so that, in addition to incontinence, patients have the feeling that they are constantly moist. Bleeding of the mucous membrane can also occur.
The longer the patient waits for definitive therapy, the more severe the symptoms become. When describing the symptoms, it is also important whether the anal prolapse withdraws spontaneously or whether it can be pushed back into the anus with the finger. This gives an indication of the severity of the anal prolapse and plays a role in the therapy decision.
Anal prolapse: causes and risk factors
The causes of anal prolapse are very diverse. Weak pelvic floor muscles play an important role. This is therefore an important starting point in therapy and aftercare.
Although anal prolapse can occur at any age, older people are more often affected. In adults, more than eight in ten patients are women. Anal prolapse is less common in children, but the risk is the same for boys and girls. If children are affected, anal prolapse usually occurs before the age of three, usually even in the child's first year. In children, there is often another disease as the cause, such as cystic fibrosis.
In adults, a general sagging of the pelvic floor is often the cause, so that other organs, such as the uterus or the bladder, can also protrude. For example, the birth process can damage the pelvic floor and thus increase the risk of anal prolapse in old age.
Certain factors increase the likelihood of anal prolapse. High defecation pressure and long-term constipation can cause a prolapse of the rectum. In most cases, the muscles of the pelvic floor are too weak to keep the bowel from falling out. The following factors also increase the risk:
- Neurological damage to the nerves in the pelvis
- Injuries to the sphincter muscle
- Gynecological interventions
- Congenital malformations
- Inflammation
- Tumor diseases
Other diseases can also lead to anal prolapse. Before each surgical procedure, the entire rectum must be carefully examined in order to rule out other diseases that may have caused the anal prolapse or that must be taken into account during an operation. Ulcers or tumors, as well as polyps, can play an important role in the development and surgical intervention.
Anal prolapse: examinations and diagnosis
For a clinically experienced doctor, anal prolapse is a visual diagnosis. An anal prolapse can be distinguished from a rectal prolapse just by looking at it and feeling it. Ultrasound examinations and reflections can confirm the suspicion and help to better assess the extent. The reflection of the lower section of the intestine is particularly used to clarify the treatment options.
If the incontinence and the degree of anal prolapse cannot be assessed, a so-called defecogram can be made. In this case, stool is excreted under x-ray fluoroscopy. This examination, which is very uncomfortable for the patient, is not the rule and is only used for special questions.
Further blood tests and examinations can provide information about the other health status of the patient and thus play a role in assessing the risk of surgery.
Anal prolapse: treatment
Treatment for anal prolapse is usually surgery. Surgery can only be dispensed with in rare exceptions. Surgery is usually not necessary for children. Consistent treatment of the underlying disease (such as cystic fibrosis) is usually the best therapy for anal prolapse.
There are many different procedures and techniques for operating theaters. In order to be able to choose the most suitable technique for the respective patient, one has to consider the affected person with all his illnesses and problems holistically. There are basically two different surgical methods: The doctor performs the procedure either through the abdominal cavity or from the anus:
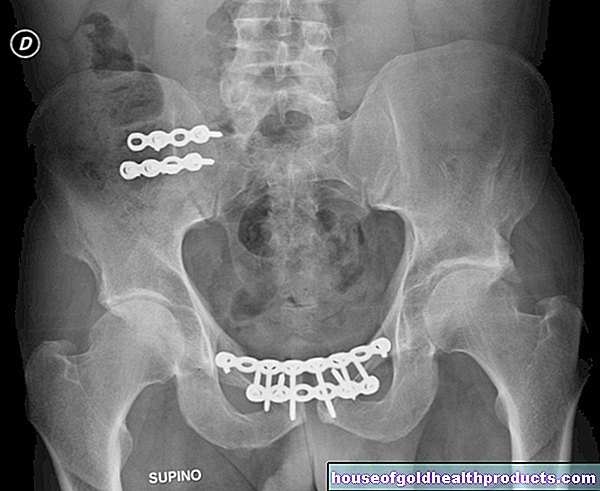
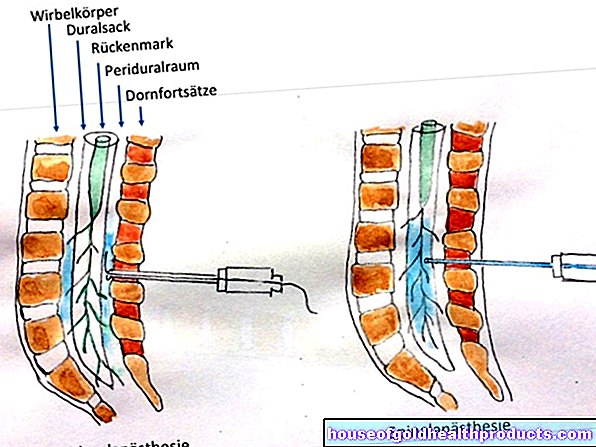
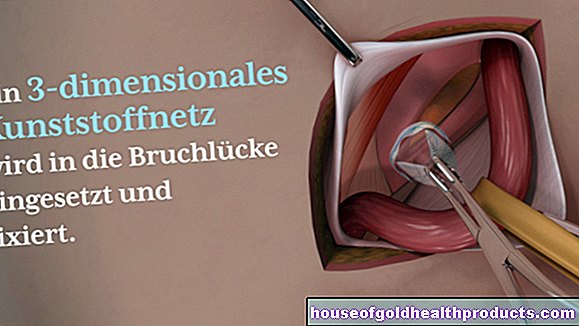
- Interventions in the abdominal cavity are carried out either via an abdominal incision (laparotomy) or a laparoscopy (laparoscopy). The doctor fixes the rectum in such a way that it can no longer sag down. He sutures the intestine at the level of the sacrum (rectopexy), with a plastic net in some cases holding the intestine in the desired position. Sometimes the surgeon needs to remove a specific section of the colon (sigmoid resection) to tighten it.
- In an operation from the anus, the doctor removes the bowel that has emerged. In doing so, he pushes back the two ends of the intestine and sutures them up again.
Overall, the risk of repeated anal prolapse is lower with an intervention via the abdominal cavity, but there is a higher risk of complications during or after the operation.
If the surgeon does not cut open the abdominal wall, but only operates on the anus, the risk of surgery for the patient is lower. However, the long-term chances of success are also lower. Depending on the patient's constitution, the advantages and disadvantages of the various interventions must be weighed up.
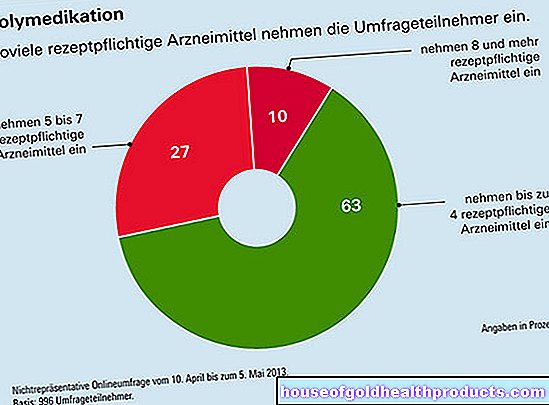
After the operation, the patient must take medication and certain nutrition plans to ensure that the stool remains soft and that there are no high pressures in the lower abdomen. It is often necessary to take antibiotics to prevent infections.
Course of the disease and prognosis
Anal prolapse is life-threatening only in rare cases. The intestine can usually be pushed back and there is no pinching. If this does happen, an emergency operation is necessary in rare cases to prevent the segment of the intestine that has fallen out from dying off.
In all other cases there is no emergency and the patient can present himself to the surgical clinic and, after having been thoroughly informed with the surgeon, choose the best procedure for him.
In younger patients in particular, the abdominal wall procedure is increasingly chosen, whereas the risk of such a large procedure is usually too high in older people. After a successful procedure, the anal prolapse is usually resolved. Patients should now pay attention to a balanced diet, prevent possible constipation at an early stage and strengthen the pelvic floor through exercise. Some clinics offer special courses to learn exercises to strengthen the pelvic floor muscles.
Tags: alcohol drugs teenager pregnancy