Spinal anesthesia
All content is checked by medical journalists.Spinal anesthesia is a method of numbing the nerves of the spinal cord. In contrast to other anesthesia procedures close to the spinal cord, a drug is injected directly next to the nerves. In this way, large areas of the body can be numbed in a short time while the patient remains fully conscious. Read all about the benefits of spinal anesthesia and when to do it.

What is spinal anesthesia?
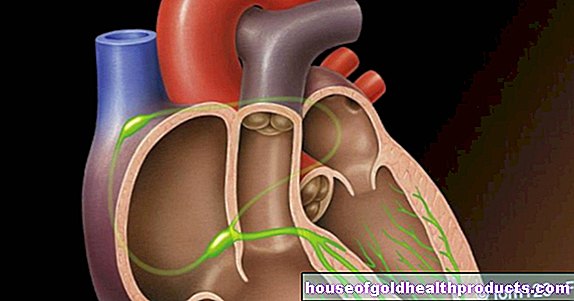
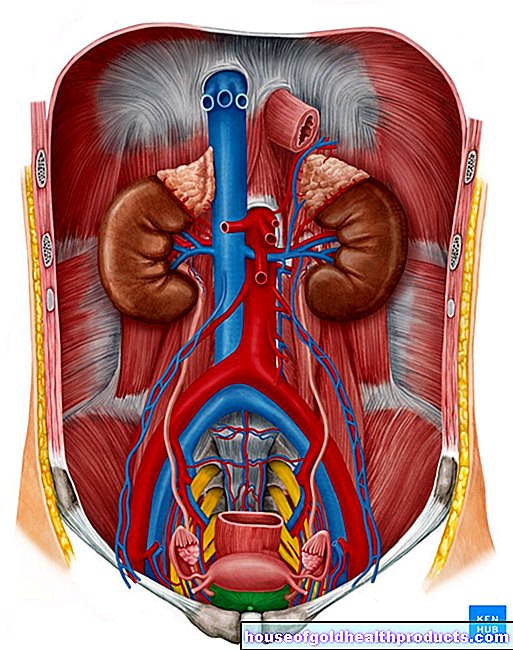
Spinal anesthesia interrupts the transmission of signals in the spinal cord nerves. To do this, the doctor injects certain narcotics (anesthetics) into the cerebrospinal fluid space (liquor space) that directly surrounds the spinal cord. In addition to the sensation of pain, pressure and temperature, the drug used also inhibits nerve fibers that control the muscles and parts of the involuntary nervous system.
Because the spinal cord transmits all nerve signals from the trunk and extremities to the brain, spinal anesthesia can numb large areas of the body from the legs to the chest. The point at which the sensation is switched off depends on the level of the spinal cord at which the anesthetic is effective.
When is spinal anesthesia performed?
Spinal anesthesia is used in many operations on the legs, pelvis or abdomen. This includes, for example, a number of orthopedic and urological interventions. Because spinal anesthesia puts less strain on the body than general anesthesia, it is often a gentler alternative. For example, it is preferred for patients with cardiovascular problems.
Spinal anesthesia can also be used in addition to general anesthesia. This reduces the consumption of painkillers during and after the operation and patients recover more quickly.
Finally, spinal anesthesia is often used in obstetrics. On the one hand for pain relief during natural births, on the other hand as an anesthetic procedure for caesarean sections. The spinal anesthesia works quickly so that even urgent operations can be carried out promptly and poses no danger to the unborn child.
What do you do with spinal anesthesia?
To create spinal anesthesia, the doctor pierces the lumbar spine with a thin needle. He pushes this forward between two vertebrae and penetrates through several ligaments in the spine. Finally, it pierces the hard skin of the spinal cord (dura mater) and reaches the space that surrounds the spinal cord and is filled with cerebrospinal fluid (liquor).
As soon as CSF flows into the syringe, the doctor knows that the needle is in the right position and can inject the drug. This usually happens once. But you can also insert a small plastic tube (catheter) into the liquor space, which makes it possible to give medication over a longer period of time.
The nature and dose of the medication and the patient's position determine the height of the spine at which the spinal anesthesia is effective. The anesthetic is always injected into the lumbar spine area. The patient is lying on the side or sitting. Inserting the needle is usually not painful, as the doctor initially anesthetizes the puncture site locally. However, some patients experience an uncomfortable feeling of pressure.
Just a few minutes after the anesthetic was injected into the liquor space, the patient usually first notices a feeling of warmth and tingling in the affected areas. After about 15 minutes, the spinal anesthesia has achieved its full effect and the patient can be positioned for the operation.
What are the risks of spinal anesthesia?
At the beginning of spinal anesthesia, an effect on the cardiovascular system is often noticeable. For example, in some patients, shortly after the anesthetic has been injected, their blood pressure and heart rate drop for a short time. These symptoms may also be associated with nausea and vomiting. However, the doctor can counteract this with special medication.
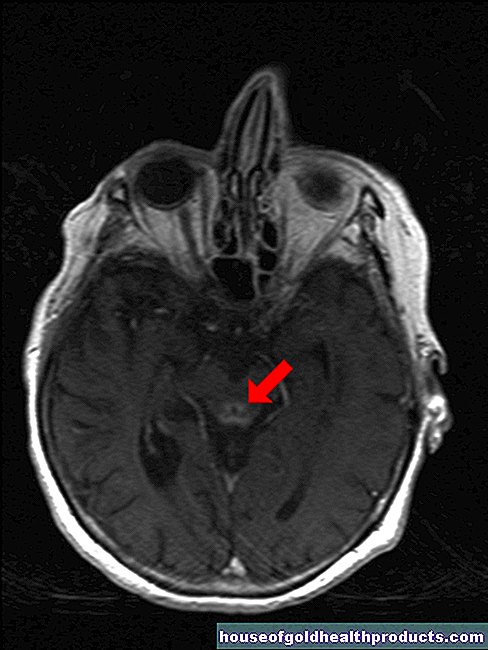
Serious complications can arise if the anesthetic is accidentally injected into a blood vessel or if excessive doses are used. The drug is then distributed throughout the bloodstream or rises too high in the liquor space. In the worst case, this can lead to cardiac arrest or respiratory paralysis.
With spinal anesthesia, some cerebral fluid always escapes from the liquor space, creating a slight negative pressure there. This can then cause headaches in the patient, which become worse, especially when the patient is in an upright posture. Such so-called post-spinal headaches can usually be treated well.
A bruise may form where the doctor inserted the needle, compressing the spinal cord. This, as well as direct injury to the nerve tissue by the needle, can lead to symptoms such as incontinence and paralysis. If the patient is taking blood thinners, they must discontinue them in good time prior to the procedure, as instructed by the doctor.
Many patients suffer from urinary retention after spinal anesthesia and therefore need a urinary catheter. In addition, even with careful disinfection, an encapsulated accumulation of pus (abscess) can form in the area of the puncture site, which constricts the spinal cord.
What do I have to consider after spinal anesthesia?
You are not allowed to drive for a day after spinal anesthesia. In addition, you should remain in bed with your upper body lifted for a while and then only get up under supervision to avoid falling. If you experience headache, back pain and nausea during this time, speak to your doctor about it so that he can treat the possible side effects of spinal anesthesia.
Tags: fitness alcohol toadstool poison plants