Antiphospholipid Syndrome (APS)
Astrid Leitner studied veterinary medicine in Vienna. After ten years in veterinary practice and the birth of her daughter, she switched - more by chance - to medical journalism. It quickly became clear that her interest in medical topics and her love of writing were the perfect combination for her. Astrid Leitner lives with daughter, dog and cat in Vienna and Upper Austria.
More about the experts All content is checked by medical journalists.Antiphospholipid syndrome (APS) is an autoimmune disease that can lead to severe to life-threatening blood clots and vascular occlusions as well as pregnancy complications. The causes of APS are so far unclear. Read here about the symptoms of APS and how it is treated.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. D68

Brief overview
- What is APS? APS is an autoimmune disease in which the immune system produces defensive substances (antibodies) against the body's own cells. Blood clots develop, which can cause serious complications.
- Causes: The causes of APS are not clearly understood.
- Risk factors: other autoimmune diseases, pregnancy, smoking, infections, estrogen-containing drugs, obesity, genetic predisposition
- Symptoms: vascular occlusions (thromboses), miscarriages
- Diagnostics: proven thrombosis or miscarriage (s), blood test (detection of antiphospholipid antibodies)
- Treatment: Blood thinning medication
- Prevention: No causal prevention possible
What is APS (Antiphospholipid Syndrome)?
Antiphospholipid syndrome (APS) is a disease in which blood clotting is impaired: the blood of those affected clots faster than usual. Blood clots form, which can lead to heart attacks, strokes or miscarriages. Doctors also speak of lupus anticoagulant syndrome or antiphospholipid antibody syndrome.
Frequency of APS
Doctors assume that around 0.5 percent of the general population develop antiphospholipid syndrome. APS can occur at any age, but usually begins in young to mid-adulthood: 85 percent of patients are between 15 and 50 years old. Women are generally more affected than men.
Forms of the GSP
APS is not a congenital disease, it develops over the course of life. Doctors distinguish between two forms of antiphospholipid syndrome, depending on whether it occurs as an independent disease or together with another underlying disease:
Primary APS
APS occurs as an independent disease in 50 percent of all those affected.
Secondary APS
In 50 percent of those affected, APS develops as a result of another disease.
The secondary antiphospholipid syndrome usually occurs together with other autoimmune diseases. These include:
- Lupus erythematosus
- Chronic polyarthritis
- Scleroderma
- psoriasis
- Behçet syndrome
- Polymyalgia rheumatica
- Autoimmune thrombocytopenia
APS is also seen in certain infectious diseases. These include, for example, hepatitis C, HIV, syphilis and mumps as well as infections with the Epstein-Barr virus (EBV). EBV infections lead, for example, to Pfeiffer's glandular fever.
Drugs rarely trigger the formation of antibodies against the body's own phospholipid-protein complexes. The most common drugs here are anti-epileptic drugs, quinine and interferon.
In a few cases, APS occurs together with a tumor such as multiple myeloma (plasmacytoma).
Causes and Risk Factors
causes
The causes of the antiphospholipid syndrome are still not fully understood. What is certain, however, is that it is an autoimmune disease.
In the case of an autoimmune disease, the immune system falsely forms defense substances (antibodies) against the body's own cells or cell components and damages them. Depending on which tissue is attacked, different autoimmune diseases such as lupus erythematosus, rheumatism or multiple sclerosis occur.
In APS, the antibodies are directed against certain endogenous phospholipid-protein complexes. They can be found, for example, on the surface of body cells.
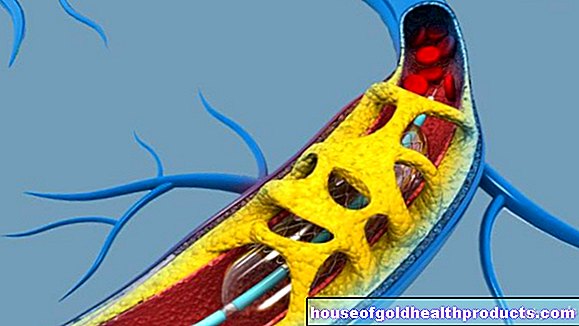
In healthy people, blood coagulation starts as soon as a blood vessel is injured. Certain blood cells (called platelets) form a plug that closes the wound again and stops the bleeding.
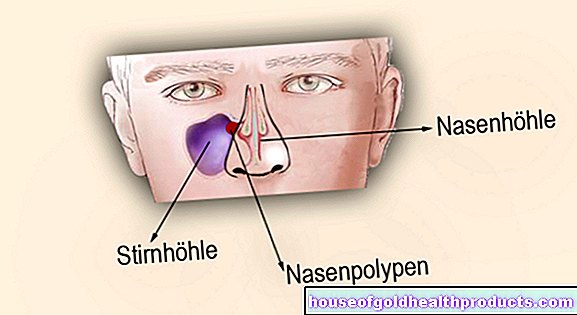
With APS, normal blood clotting is disturbed: the blood clumps faster, even without previous injury. A blood clot forms. If this reaches a certain size, it leads to vascular occlusion (thrombosis).
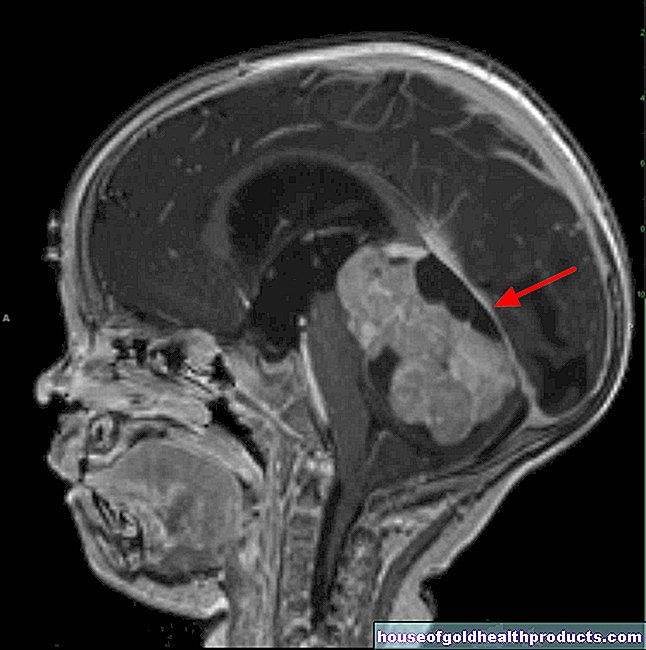
Since phospholipid-protein complexes occur in all body cells, blood clots and thromboses can occur anywhere in the body. If the blood vessel is blocked, the tissue is no longer (sufficiently) supplied with blood (ischemia). Most common with APS there is vascular occlusion in the brain, in the heart and in pregnant women in the placenta area.
Risk factors
Not all people who have antiphospholipid antibodies will develop blood clots. The risk is around 50 percent. Why some people get GSP and others don't is not clear.
Doctors assume that genetic predisposition plays a role: The literature describes that other family members are often affected in APS patients. Around a third of the blood relatives of an APS patient also have elevated levels of the corresponding autoantibodies. However, the assessment has not yet been clearly proven.
In addition, most people with APS who develop thrombosis have other risk factors. These include:
- pregnancy
- smoking
- Taking oral contraceptives (pill)
- Obesity
- Infectious diseases such as hepatitis C.
- Damage to the inner wall of the blood vessels
Symptoms
Patients who have antiphospholipid antibodies in their blood but have not yet had a thrombosis or pregnancy complications usually do not notice anything. The following signs point to APS - but also to many other diseases:
- headache
- dizziness
- Memory problems
- Bluish discoloration under the skin, often tree-like branches (Livedo racemosa)
The antiphospholipid syndrome is usually only noticeable when thrombosis occurs. This is the case in about half of all people with antiphospholipid antibodies. The symptoms depend on which vessel is blocked. The most common are:
- Swelling of the leg with drawing pain (deep leg thrombosis)
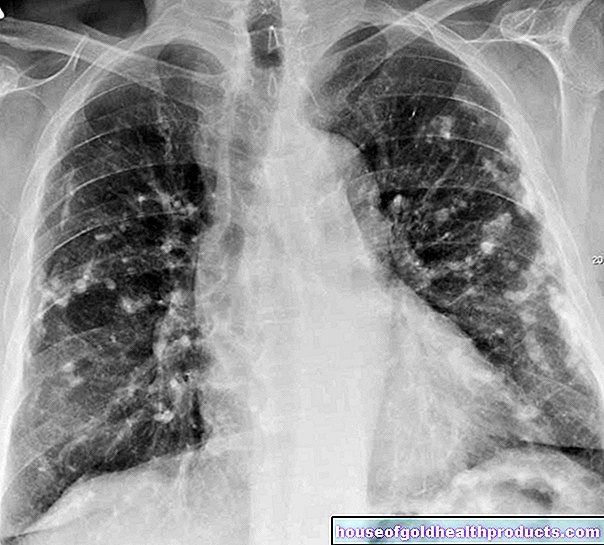
- Sudden shortness of breath with sharp pain in the chest (pulmonary embolism)
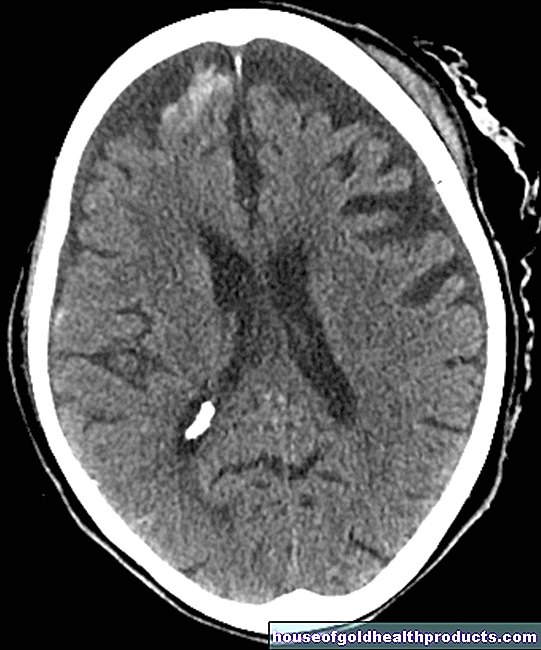
- Sudden paralysis on one side of the body or difficulty speaking (stroke)
- Seizure
- migraine
- Bleeding under the fingernails or toenails
- Pregnancy complications
Vascular occlusion in the arteries (arterial thrombosis)
With the exception of the pulmonary artery, arteries carry nutrient- and oxygen-rich blood to the organs. If an artery is blocked, the tissue behind it is no longer adequately supplied with blood. For example, an arterial thrombosis in the brain causes a stroke, and in the heart a heart attack.
Vascular occlusion in the veins (venous thrombosis)
Veins carry oxygen-poor blood back to the heart (the pulmonary vein, which pumps oxygen-rich blood to the heart, is an exception here). Vascular occlusions in the veins mostly occur in the deep veins of the leg (deep vein thrombosis), less often in the arms (arm vein thrombosis). When parts of the thrombus loosen and are flushed with the bloodstream into a vessel in the lungs, they clog it. The lungs or parts of them are no longer adequately supplied with blood. A pulmonary embolism occurs, in the worst case a pulmonary infarction.
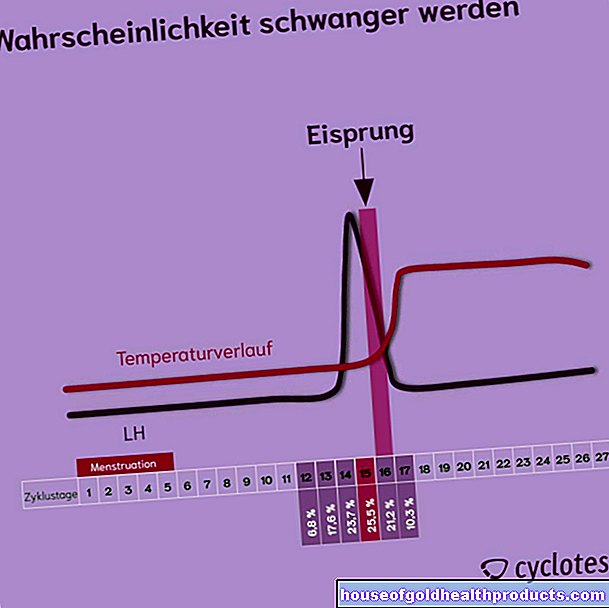
Blood clotting disorder in pregnancy
Many women with antiphospholipid syndrome carry out their pregnancy without complications and give birth to a healthy child. In some cases, however, blood clots cause problems during pregnancy.
Blood clotting disorders in the uterine lining may prevent the embryo from implanting in the uterus. If this is the case, a miscarriage occurs.
If a blood clot develops in the placenta or in the umbilical cord, the child is no longer adequately supplied with blood. The undersupply leads to the fact that the unborn child lags behind in its growth or is even rejected. Pregnancy diseases such as eclampsia and preeclampsia (high blood pressure with protein excretion in the urine) also indicate APS.
Women who have had repeated miscarriages are recommended to be tested for antiphospholipid antibodies. If the pregnant woman is treated accordingly, the probability of giving birth to a healthy child is around 90 percent despite APS.
diagnosis
The first point of contact if the antiphospholipid syndrome is suspected is the internist or rheumatologist.
Physical examination
The doctor first asks about the medical history (anamnesis) and conducts a physical examination. If thromboses or miscarriages have already occurred in the past, the suspicion of APS is reinforced.
Blood test for antibodies
This is followed by a blood test. The doctor examines the blood for antibodies that speak for APS:
- Antibodies against proteins of coagulation factors: lupus anticoagulant (LA)
- Antibodies against cardiolipin: anti-cardiolipin antibodies (aCL)
- Antibodies against beta2-glycoprotein 1: anti-beta-2-glycoprotein I antibody (ab2gp1)
APS antibodies are found in one to five percent of the population, for example in connection with bacterial or viral infections or cancer.
Sidney criteria
The doctor diagnoses the antiphospholipid syndrome based on the so-called "Sidney criteria": APS is established when the doctor detects at least one physical condition and at least one type of APS antibody.
Physical signs for APS:
- Secure thrombosis in the area of the larger or smaller veins / arteries
- Three (or more) miscarriages before the tenth week of pregnancy or one (or more) miscarriages after the tenth week of pregnancy that cannot be explained by other causes.
Detection of APS antibodies:
- The diagnosis is confirmed when the elevated antiphospholipid antibodies can be detected twice at an interval of at least twelve weeks.
treatment
Since there are no drugs that inhibit the formation of antiphospholipid antibodies or block their effect, a cure is not possible. However, the risk of (further) blood clots is significantly reduced with anticoagulant medication.
Which therapy is used for an antiphospholipid syndrome depends on the type of thrombosis (arterial, venous or during pregnancy) and the risk of the individual patient.
Treatment depending on the personal risk of thrombosis
The risk of thrombosis in APS is different for each patient. There is a high risk if lupus anticoagulants are found in the blood. Patients in whom all three antibodies can be detected (triple-positive) have the highest risk of thrombosis.
According to one study, 37.1 percent of these patients will develop one or more additional thromboses within ten years. If only the antibody against beta2-glycoprotein 1 is increased, the risk is lower.
The risk of thrombosis also increases if patients have high cholesterol, high blood pressure, or smoke. The same applies to women who take estrogen-containing medication such as the pill or preparations for menopausal symptoms.
Medication
The doctor treats the antiphospholipid syndrome with anticoagulant drugs. They cause clotting to start later and more slowly than usual, thereby preventing blood clots from forming. If there is an injury, however, it takes longer for the wound to close and the bleeding to stop. So people who take anticoagulant drugs have a potentially increased risk of bleeding.
There are different anticoagulants available for the treatment of APS:
Vitamin K antagonists
In order to be able to clot, the blood needs vitamin K. Vitamin K antagonists are antagonists of vitamin K and inhibit blood clotting. They are taken as tablets or capsules and usually work with a delay of two to four days. During the treatment, the doctor regularly checks the INR value: This shows how quickly the blood coagulates.
Vitamin K antagonists used to treat APS are:
- Phenprocoumon
- Warfarin
Vitamin K antagonists should not be taken by pregnant women as this could damage the unborn child.
Antiplatelet agents
Platelet inhibitors prevent the blood platelets from attaching to blood vessel walls and forming a blood clot as easily. They are also taken as tablets or capsules. The best-known example of a platelet inhibitor is acetylsalicylic acid (ASA).
Direct / new oral anticoagulants (DOAK, NOAK)
DOAC / NOAC work similarly to platelet inhibitors, but more powerful and their effect is quicker. The DOAC / NOAC include the active ingredients apixaban, dabigatran, edoxaban and rivaroxaban.
Heparin
Heparin is an anticoagulant that is injected under the skin or into a vein. Since the effect occurs very quickly, heparin is used for the acute treatment of thrombosis.
Fondaparinux
Fondaparinux is an anticoagulant that is injected under the skin like heparin. It is suitable for acute treatment and for the prevention of thrombosis.
Treatment of existing thrombosis
If a thrombosis occurs as a result of the antiphospholipid syndrome, acute therapy is usually given with heparin. It causes the thrombus to dissolve. The patient then receives the active ingredient phenprocoumon. It prevents more blood clots from forming.
Treatment if antibodies are detected without a previous thrombosis
People without symptoms, but who have antiphospholipid antibodies, have an increased risk of thrombosis. In some cases, preventive treatment with blood-thinning medication (acetylsalicylic acid) is appropriate. Here, the doctor decides on a case-by-case basis whether preventive therapy makes sense.
Treatment during pregnancy
For women diagnosed with antiphospholipid syndrome, it is advisable to consult with their doctor before a planned pregnancy. Oral anticoagulants such as phenprocoumon can harm the unborn child. Therefore, the doctor will adjust APS therapy that was started before pregnancy accordingly.
APS patients who want to have children and those who are diagnosed with pregnancy will then receive (low molecular weight) heparin once a day. Heparin does not reach the child via the placenta and is therefore harmless to mother and child. Pregnant women often receive a low dose of acetylsalicylic acid up to the 36th week of pregnancy.
Latest studies
The latest studies on antiphospholipid syndrome show that direct oral anticoagulants (DOAC / NOAC) should not be used in high-risk groups.
In September 2018, the results of the TRAPS study (Trial on Rivaroxaban in Anti-Phospholipid Syndrome) were published: The researchers compared the two active ingredients rivaroxaban and warfarin in high-risk patients with APS. Since patients treated with the direct oral anticoagulant (DOAC) rivaroxaban had significantly more complications (predominantly arterial thrombosis), the study was terminated prematurely.
A meta-analysis (summary of several studies) also showed a higher risk for DOAC compared to vitamin K antagonists (e.g. warfarin).
According to the current recommendations of the European Rheumatism League from 2019, rivaroxaban should therefore not be used in triple-positive APS patients, but should be replaced by vitamin K antagonists.
Prevent
Since the trigger for antiphospholipid syndrome is unknown, there are no specific preventive measures. People who have already suffered a thrombosis should have regular check-ups with their doctor and take any prescribed medication carefully.
Women with APS are advised to avoid medication containing estrogen, such as those used for contraception or the treatment of menopausal symptoms. Because estrogen can significantly increase the risk of thrombosis.
In addition, it is advisable to pay attention to a balanced lifestyle. This includes abstaining from nicotine, sufficient fluids, a healthy diet, plenty of regular exercise and enough relaxation and recovery phases.
forecast
There is no cure for APS. However, with individually tailored treatment and regular check-ups with a doctor, the risk of thrombosis can be significantly reduced.
Tags: parasites travel medicine sex partnership








-nachrichten-aus-der-rhre.jpg)






.jpg)