Scarlet fever
and Martina Feichter, medical editor and biologistRicarda Schwarz studied medicine in Würzburg, where she also completed her doctorate. After a wide range of tasks in practical medical training (PJ) in Flensburg, Hamburg and New Zealand, she is now working in neuroradiology and radiology at the Tübingen University Hospital.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Scarlet fever (Scarlatina) is a very contagious infectious disease. The triggering bacteria are transmitted via tiny droplets of saliva and can cause sore throats, rashes and fever. Here you can read more about the topic: What exactly is scarlet fever? How does the infection take place? How long is the scarlet fever incubation period? What are the symptoms? How is scarlet fever treated?
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. A38
Brief overview
- Important symptoms: sore throat, tonsillitis with reddening, swelling, pain; Pallor around the mouth (perioral) and "raspberry tongue" (bright red tongue), characteristic rash (small speckled papules, starting on the upper body, then all over the body except the palms and soles of the feet)
- Contagion: mostly via droplet infection (via sneezing, coughing, speaking) or smear infection (using / touching contaminated objects and surfaces)
- Investigations: throat examination, rapid scarlet fever test, blood tests for bacteria and antibodies
- Treatment: bed rest, gargling, pain relievers and fever killers (paracetamol, ibuprofen), antibiotics
- Complications and long-term effects: abscess of the tonsils, pneumonia, otitis media, sinusitis, acute kidney inflammation, rheumatic fever, inflammation of the inner lining of the heart (endocarditis) and myocarditis
Scarlet fever: symptoms
Scarlet fever symptoms appear for the first time around one to three days after infection with the triggering bacteria (scarlet fever incubation period). The disease almost always starts suddenly out of the blue. Common symptoms of scarlet fever are:
- Sore throat
- difficulties swallowing
- often high fever
- chills
- flushed cheeks
- Exhaustion
- Vomit
- Abdominal pain (especially in younger children)
- Headache and pain in the limbs
Signs like these, however, are not clear and can also occur with many other diseases. Only typical scarlet fever symptoms bring certainty: In addition to raspberry tongue and a characteristic rash, this includes scarlet fever angina, an inflammation of the tonsils.
There are also people who experience scarlet fever without a fever or rash. Older patients in particular often do not show all of the typical scarlet fever symptoms. In general, the disease is easily overlooked in adults.
Three characteristic symptoms of scarlet fever
Scarlet fever angina
Almost everyone with scarlet fever will develop tonsillitis (tonsillar angina). None of the other symptoms of scarlet fever occur as regularly as this one. The reason for this is that the scarlet fever pathogens colonize the lining of the throat. This can inflame the tonsils - and also the entire throat. These areas are then reddened, the palatine tonsils are usually clearly swollen and sometimes also covered with a white layer.
Other symptoms of scarlet fever in the mouth are small, whitish deposits on the inside of the cheeks. Often the neck lymph nodes are also swollen. These scarlet fever symptoms are similar to the signs of common tonsillitis.
Raspberry tongue
The raspberry tongue is one of the specific symptoms of scarlet fever. First of all, the tongue is covered with a white layer. This layer disappears after about four days and a raspberry-red tongue appears.
Scarlet fever rash
Scarlet fever rash develops on the first or second day of the disease: Pinhead-sized, bright red and slightly raised spots (papules) form that are rough to the touch but not itchy. The first thing the scarlet fever rash is often about is the groin area and the inner thighs. As a result, it then spreads over the whole body. Only a small triangle between the mouth and chin and the soles of the feet and palms are left out.
The rash will slowly go away after six to nine days. As a result, the skin often begins to flake - including on the soles of the feet and palms.
Skin rash in scarlet fever
Scarlet fever: complications and long-term effects
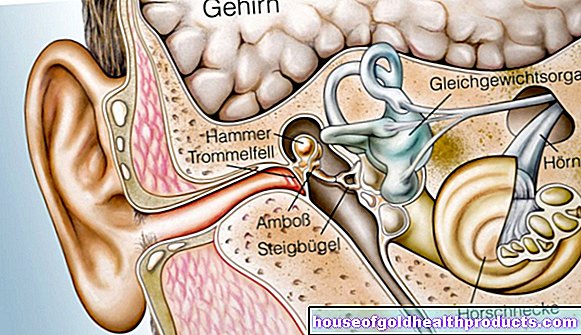
Scarlet fever symptoms usually improve very quickly with antibiotic therapy. Without treatment, however, the scarlet fever symptoms can last longer and under certain circumstances become more severe: some patients develop a highly purulent tonsillitis. Encapsulation of the pus creates an abscess. Sometimes a purulent otitis media accompanies it. A possible consequence of missing treatment is hearing loss.
The germs from the pharynx can not only get into the middle ear, but also into the paranasal sinuses or lungs. Then a sinus infection (sinusitis) or pneumonia (pneumonia) can develop - in addition to the symptoms of scarlet fever mentioned above.
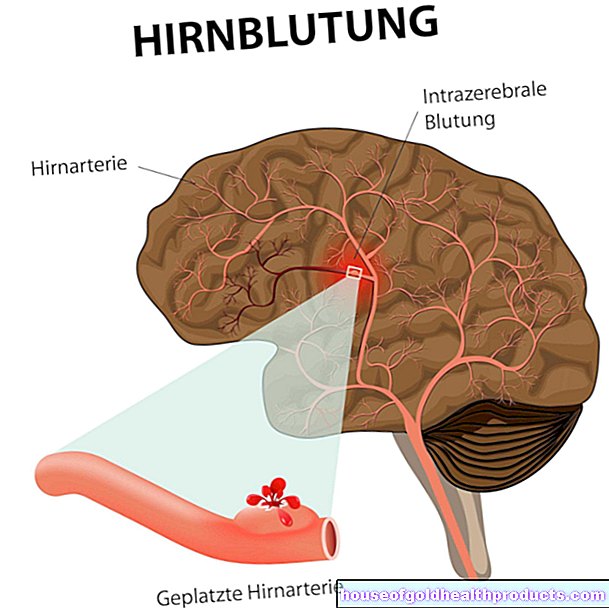
The septic course of scarlet fever is very rare, but potentially life-threatening: The scarlet fever bacteria penetrate the bloodstream and are distributed throughout the body. "Blood poisoning" (sepsis) develops with a sudden high fever, vomiting, diarrhea, bleeding from the skin and mucous membranes, clouding of consciousness, severe heart damage and shock.
A possible late complication of scarlet fever is an acute rheumatic fever. It occurs primarily in patients between the ages of three and fifteen years, usually after a symptom-free period of 19 days. Various joints or organs (such as the heart) become inflamed in those affected. Acute inflammation of the kidneys (glomerulonephritis) can also develop as a long-term consequence of scarlet fever (after one to five weeks for throat infections, after three weeks for skin infections).
-
Scarlet fever - "Not a harmless childhood disease!"
Three questions for
Prof. Dr. Jörg Schelling,
Specialist in General Medicine -
1
Isn't scarlet fever a harmless childhood disease?
Prof. Dr. Jörg Schelling
No - there are no harmless teething problems. "Teething troubles" are often more severe in adults! You don't need to panic with scarlet fever either, but you should contact your family doctor. As a rule, scarlet fever is easily recognizable, treatable and heals without consequences.
-
2
Why are scarlet fever diseases coming back more often?
Prof. Dr. Jörg Schelling
With increasing globalization and the disappearance of borders, the number of scarlet fever diseases is also increasing again in Germany. Unfortunately, there is no vaccination yet. Also, even if you've already had the disease, you won't become immune to scarlet fever.
-
3
How can I prevent scarlet fever disease?
Prof. Dr. Jörg Schelling
Avoid direct contact with sick people during the contagious first three days. In general, good hygiene, i.e. correct hand washing with soap, is important when protecting against scarlet fever. Hand disinfectants are also useful to further minimize the risk of infection. Preventive treatment of contact persons with antibiotics is only carried out in rare individual cases.
-
Prof. Dr. Jörg Schelling,
Specialist in General MedicineFounding director at the Institute for General Medicine at LMU Munich and member of the Bavarian state working group on vaccinations. As a vaccination expert, he trains general practitioners in vaccinating.
Scarlet fever: contagion
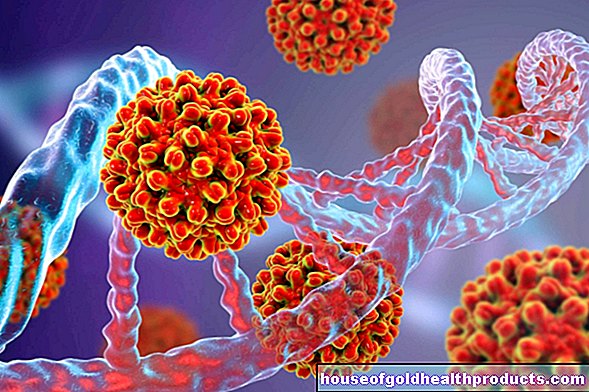
Scarlet fever is caused by infection with certain streptococcal bacteria. These are "Streptococcus pyogenes", also called A streptococci. The germs attach themselves mainly to the mucous membrane in the mouth and throat and can cause inflammation here. In addition, they produce toxic metabolic products (toxins), which cause the typical skin changes.
How does the scarlet fever infection take place?
The scarlet fever bacteria are found in the saliva of patients. They are transmitted from person to person through direct or indirect contact, more rarely when coughing, sneezing or speaking, packaged in tiny liquid droplets. Other people nearby can inhale these droplets and become infected with scarlet fever (droplet infection). People who are in close contact with scarlet fever patients are particularly at risk. The infectious disease therefore often spreads in community facilities such as kindergartens or schools.
When patients hold their hands over their mouths when coughing or sneezing, the bacteria-containing droplets get onto the palms of their hands. From there they can be transferred to objects such as cutlery or doorknobs. If a healthy person uses the same cutlery or touches the contaminated objects and then grabs his mouth or nose with his hand, he can also become infected with scarlet fever (smear infection).
Scarlet fever is only rarely infected through contaminated food or water (food infection).
Occasionally, the scarlet fever pathogens enter the body through skin wounds (wound scarlet fever).
Cough secretion as a source of infection
How long is scarlet fever contagious?
With an acute strep infection, such as scarlet fever, that is not specifically treated, patients can be contagious for up to three weeks. In the case of purulent excretions, the risk of infection can persist even longer without treatment.
However, once effective antibiotic treatment has been initiated, patients are no longer contagious after 24 hours.
Can you get scarlet fever more than once?
Regardless of whether a scarlet fever disease is being treated or not - once you have overcome the disease, you are not immune to re-infection! In the course of an infection, the body forms a certain protection against certain bacterial toxins. But there are different strains of scarlet fever, so that a person affected can be infected several times. If, on the other hand, a person is attacked a second time by the same strain of pathogen after a previous scarlet fever infection, they will most likely not get sick with scarlet fever, but at most with tonsillitis (angina tonsillaris).
By the way: not everyone who carries the scarlet fever pathogen also gets sick. The throat is colonized with the bacteria in up to 20 percent of the population, but there are no symptoms.
Scarlet fever in children and adults
As a childhood disease, scarlet fever is more common in children than adults. Usually children between the ages of six and twelve get it. In principle, however, scarlet fever can occur at any age. Only infants are relatively safe from infection because they have the appropriate antibodies from their mother ("nest protection").
Scarlet fever in adults is often not recognized or recognized only late: In the case of a sudden fever, sore throat and difficulty swallowing, many do not think of the possibility of being infected with the pathogen of the "childhood disease" and do not go to the doctor at all or only too late. This can have serious consequences under certain circumstances: Scarlet fever in adults, as in children, can cause complications and long-term effects such as rheumatic fever as well as heart and kidney infections.
Scarlet fever: pregnancy
When a pregnant woman develops scarlet fever, there is nothing particularly to worry about at first. The disease has no direct impact on the unborn child. In contrast to other childhood diseases such as rubella, mumps or measles, there is no specific risk of child malformations, miscarriages or stillbirths.
However, indirectly, scarlet fever can have a negative impact on the child during pregnancy: if the expectant mother develops complications such as inflammation of the heart muscle, this can impair the supply of oxygen and nutrients to the unborn child and thus impair the child's development.
Scarlet fever during pregnancy should therefore be treated with antibiotics at an early stage. In addition, the pregnant woman and her unborn child are medically monitored - as with all infectious diseases during pregnancy.
You can read more about this in the article Scarlet Fever and Pregnancy.
Scarlet fever: examinations and diagnosis
The typical symptoms of the disease usually quickly lead the doctor to suspect scarlet fever. To be on the safe side, he first takes the medical history (anamnesis). He asks the patient (in the case of children: the parents), for example, when the fever started and whether people in the area are currently sick with scarlet fever.
This is followed by the physical examination: the doctor checks whether the throat and tonsils are red, swollen or white. He also feels the lymph nodes on the neck. They can swell with scarlet fever. The doctor also looks at the skin all over the body. If there is a rash, he asks where it started and whether it is itchy. A scarlet fever rash temporarily fades under the pressure of a wooden spatula. Sometimes a rash forms on the lining of the mouth in patients.
Palpation of the lymph nodes
For a rapid scarlet fever test, the doctor takes a swab from the lining of the throat to examine it for streptococci. The result is clear after just a few minutes. However, it is not entirely reliable: If the result is positive, there is very likely an infection with group A streptococci. However, a negative test result does not reliably rule out such an infection. Then you can send the throat swab to the laboratory in order to cultivate any pathogens it may contain (bacterial culture) and then determine it.
The blood values can also indicate a scarlet fever infection. In general, with inflammation, the white blood cells (leukocytes) and the rate of sedimentation are often increased.
There is also the option of testing the patient's blood for antibodies against the scarlet fever pathogen. However, this only makes sense if a streptococcal secondary disease such as rheumatic fever is suspected.
Scarlet fever: treatment
Scarlet fever therapy usually consists of giving an antibiotic. It allows the symptoms to subside a little faster and prevents complications. In addition, patients are no longer contagious to other people just 24 hours after starting antibiotic therapy.
Generally, scarlet fever is treated with penicillin. The antibiotic is given orally (as a tablet) or parenterally (as a syringe). It must be used for ten days. If the antibiotic is stopped earlier, the risk of relapse increases.
If someone is allergic to penicillin, scarlet fever therapy is done with a different antibiotic. For example, cephalosporins and erythromycin are suitable.
In the case of severe disease such as sepsis (blood poisoning), the antibiotic clindamycin should be administered in addition to penicillin injections.
In some patients, scarlet fever leads to a rheumatic fever as a long-term consequence. Those affected are at increased risk of getting strep A again. Such relapses can be much more severe and exacerbate existing heart damage. Therefore, in the case of rheumatic fever, prolonged treatment with penicillin is recommended to prevent relapses. This recurrence prophylaxis should be carried out for at least five years.
Scarlet Fever Therapy: More Tips
- Patients should keep bed rest, especially if they have a fever.
- In the first two days of antibiotic therapy, the sick should also avoid contact with other people. This will reduce the risk of infecting others with scarlet fever. For the same reason, patients should always cough or sneeze into a tissue or the crook of their elbows, and then wash their hands thoroughly with soap and water.
- Gargle solutions with medicinal plants such as sage or marshmallow as well as warm throat compresses help against the unpleasant sore throat caused by scarlet fever (read more about the effects and use of compresses here).
- Because of the pain when swallowing, soft or liquid food is recommended. The diet should be low in salt and protein.
- If patients have a fever, they should drink plenty of fluids. For example, lime blossom tea sweetened with honey is recommended. Water or diluted juices are also suitable.
- If necessary, ibuprofen or paracetamol can also be taken against the pain and fever. Both active ingredients relieve pain and lower fever.
- Antibiotic therapy can unbalance the intestinal flora. To avoid this, yoghurt should be eaten regularly - but at a later time than the antibiotic administration.
Sometimes homeopathy and other alternative healing methods are recommended to support the conventional medical treatment of scarlet fever. Anyone interested in this should seek advice from an experienced doctor or therapist.
Children and adolescents who are proven or suspected of having scarlet fever are temporarily not allowed to visit community facilities (such as kindergartens, schools). Sick employees of such a facility are only allowed to go back to work when they are no longer contagious. The attending doctor or the health department will decide on this.
Scarlet fever: disease course and prognosis
With early antibiotic therapy, the scarlet fever symptoms usually subside after a few days. In most cases, once the antibiotic treatment is over, people will be completely healthy again.
Complications and long-term consequences
In rarer cases, the childhood disease scarlet fever takes a severe course or has long-term consequences.These include acute kidney inflammation (acute glomerulonephritis) and acute rheumatic fever. The latter can be accompanied by joint pain and inflammation of the inner lining of the heart (endocarditis), the heart muscle (myocarditis) or the pericardium (pericarditis). In addition, rheumatic fever can affect the brain and cause a form of movement disorder (chorea minor, syn. Sydenham).
The risk of complications and long-term effects of Schlarl fever disease can be reduced by early treatment with antibiotics.
Scarlet fever: prevention
There is no vaccination against scarlet fever. But there are other ways you can reduce the risk of the disease: Avoid close contact with sick people and wash your hands regularly with soap. For people with serious underlying diseases or a weakened immune system, the doctor may be able to prescribe an antibiotic as a preventive measure to protect them from contracting scarlet fever.
Additional information
Guideline:
- S2k guideline "Therapy of inflammatory diseases of the palatine tonsils - tonsillitis" (as of 2015)