Seizure
and Carola Felchner, science journalistMarian Grosser studied human medicine in Munich. In addition, the doctor, who was interested in many things, dared to make some exciting detours: studying philosophy and art history, working on the radio and, finally, also for a Netdoctor.
More about the expertsCarola Felchner is a freelance writer in the medical department and a certified training and nutrition advisor. She worked for various specialist magazines and online portals before becoming a freelance journalist in 2015. Before starting her internship, she studied translation and interpreting in Kempten and Munich.
More about the experts All content is checked by medical journalists.In the event of a seizure, those affected lose all control of their body for a short time, suddenly sink to the ground, twitch and convulsively. While demonic forces were suspected in the Middle Ages, we now know that a seizure is the result of a disorder in the brain. Read about what can trigger a seizure, how you should react to it, and how dangerous a seizure is.

Brief overview
- What is a seizure? An involuntary event with spasmodic or twitching movements, possibly with loss of consciousness.
- Causes: Mostly epilepsy, although the trigger of the seizures is sometimes known (e.g. increased intracranial pressure, hypoglycaemia, encephalitis) and sometimes not. Non-epileptic seizures are less common, e.g. a febrile seizure in children (febrile convulsions) or seizures as a result of a stroke.
- First aid in the event of a seizure: remove dangerous objects from the vicinity of the person affected, protect his head, if necessary bring the person into a stable position on their side and call the emergency doctor.
- How dangerous is a seizure? Seizures often go away on their own. It becomes dangerous if the seizure occurs during a dangerous activity (e.g. driving a car, working with a chainsaw) or expresses itself as "status epilepticus" (a persistent epileptic seizure).
Seizure: causes and possible diseases
A seizure is usually a sudden, involuntary event with convulsive or twitching movements. The affected person can also lose consciousness. Sometimes a seizure shows all of these three characteristics, and sometimes it doesn't.
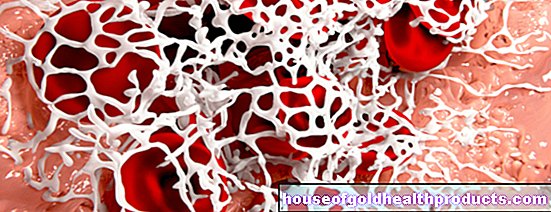
Typically, a seizure is caused by a malfunction of nerve cells (neurons) in the cerebral cortex. The normal task of a nerve cell is to generate or receive and transmit electrical signals. This happens millions of times in the brain every second, but in an orderly manner.
In the case of a cerebral seizure (= seizure emanating from the brain), however, all order is lost, so that suddenly certain groups of nerve cells discharge at the same time and transmit their uncoordinated signals synchronously. They infect downstream nerve cells with it, so to speak. Figuratively speaking, a seizure could also be described as a “thunderstorm in the brain”.
Seizures usually occur as part of epilepsy. Non-epileptic seizures are less common.
There are also seizures that are not based on a neurological disorder in the brain, but have psychological reasons (e.g. an extreme stressful situation). This is then a psychogenic seizure.
Epileptic seizures
In those affected, the nerve cells (neurons) in the brain are more susceptible to spontaneous and uncoordinated discharges. Such discharges - and with them epileptic seizures - can occur for no apparent reason. Then one speaks of idiopathic epilepsy. A distinction must be made between symptomatic epilepsy, in which the epileptic seizures have known triggers. These include:
- Brain injuries: As a result of such injuries, scar tissue can form in the brain, which in turn can lead to a seizure.
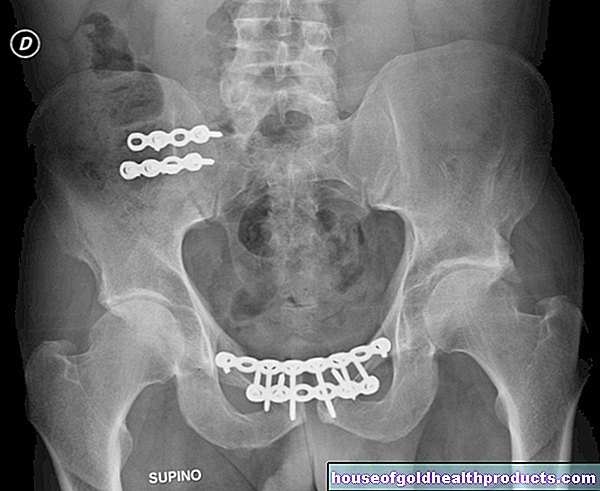
- Circulatory disorders: impaired cerebral blood flow (such as a stroke) occasionally leads to epileptic seizures.
- Tumors or inflammation: Sometimes epileptic seizures are the symptom of a brain tumor or an inflammation of the meninges or meninges (encephalitis, meningitis).
- Increased intracranial pressure: Increased pressure in the brain (e.g. as a result of an injury) can also promote seizures.
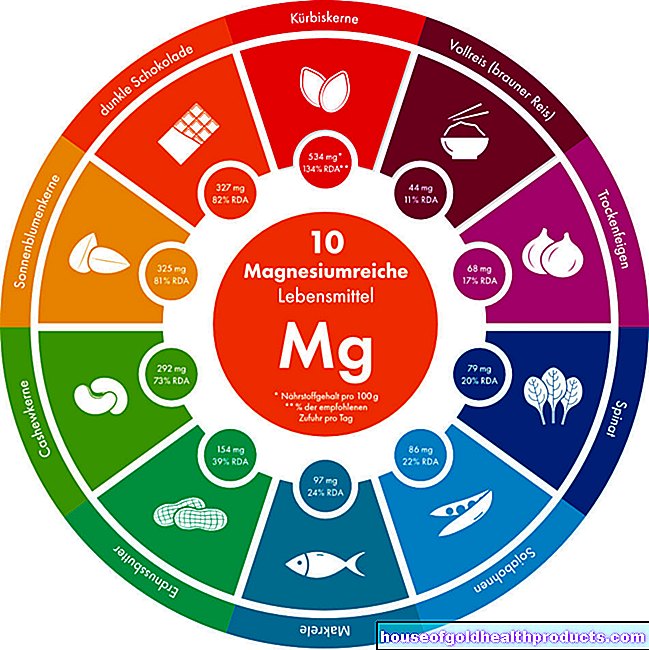
- Metabolic disorders: Sometimes low blood sugar (hypoglycaemia) can be identified as a cause of convulsions.
- Oxygen deficiency: If hypoxia lasts for a long time, the body will eventually be undersupplied. In the brain, the lack of oxygen can trigger seizures, among other things.
- Optical stimuli: For some people, for example, strobe light in the disco triggers a seizure.
- Poisoning: For example, drugs such as tricyclic antidepressants can provoke seizures.
- Drugs like alcohol: For example, if an alcoholic goes through withdrawal, seizures can occur.
A single seizure is not (yet) called epileptic.
Non-epileptic seizures
Some people have seizures, but they do not have epilepsy. Such non-epileptic seizures are not based on an increased susceptibility of the neurons to seizures - rather they are caused by a reversible disorder in the brain or another condition that irritates the brain, such as:
- Head injury
- stroke
- infection
- Medication
- Drugs
- in children: fever (febrile convulsions)
A distinction must be made between seizures and other diseases and disorders that can lead to cramping of the muscles. For example, a tetanus infection (tetanus) leads to muscle cramps all over the body.
First aid for a seizure
Whenever you see someone having a seizure, it is best to keep calm - even if such a full body cramp is often a frightening sight. The attack usually stops on its own after a few minutes. Otherwise, the following recommendations apply:
- remove dangerous objects that are close to the convulsant so that he does not injure himself.
- protect the head (e.g. with a pillow)
- do not hold the victim
- Do not put any objects in the mouth as a bite wedge (e.g. spoons) - there is a risk of injury and the risk that the patient will inhale or swallow the object.
- Secure the airways by turning the patient into a prone or stable lateral position.
- Call an ambulance if the seizure lasts more than five minutes.
If it is known that the patient is already being treated for seizures, you do not need to consult a doctor if the seizure is minor. In the event of a first attack, however, it is always advisable to alert a doctor.
How dangerous is a seizure?
Single seizures are usually not dangerous and go away on their own. However, an epileptic seizure that lasts longer than five minutes (status epilepticus) is life-threatening. Therefore, in such cases, the emergency doctor must be alerted immediately!
In principle, it can also be dangerous if someone has a seizure in a dangerous situation - for example at the wheel of a car or when working on the roof or with a chainsaw. Epileptics should take this to heart, even if the last seizure was a long time ago.
Normally, if an epileptic has not had a seizure for at least a year, he is allowed to drive a car privately again. There are exceptions to this, for example in treatment-resistant epilepsy.
Seizure: What Does the Doctor Do?
First, the doctor clarifies whether you actually had a seizure. To do this, he must rule out other causes that can produce similar symptoms. If the patient actually has a seizure, it is important to clarify the cause and, if necessary, initiate treatment.
Diagnosing a seizure
The exact description of the symptoms - either by the patient himself or by relatives - can already be very helpful. In addition, the doctor asks, among other things:
- How long did the seizure last?
- What preceded the attack? (Sometimes unusual sensations such as tingling in the stomach or an unusual smell occur shortly beforehand, or the patient has a premonition that a seizure is about to follow)
- How quickly did you / did the patient recover after the attack?
- Are there any factors that could trigger the seizure (sounds, flashing lights, etc.)?
- If there is a pre-existing or underlying disease (e.g.Brain infection) or a recent head injury?
- Do you / does the patient consume dorgen such as alcohol? Is withdrawal currently taking place?
The patient's brain waves are then measured and recorded using electroencephalography (EEG) in order to detect any abnormalities. The doctor can also try to provoke a seizure during the measurement - for example by using certain light stimuli or by deliberately hyperventilating the patient.
An EEG can also be recorded over a longer period of time. There is also the option of filming the patient during this (video EEG monitoring) so that the doctor can see exactly what is happening during a (possible) further seizure.
To identify possible causes of seizures, the doctor can also use computed tomography (CT) or magnetic resonance imaging (MRI, magnetic resonance imaging) to create detailed cross-sectional images of the brain. It may reveal structural changes (such as a stroke) that could cause seizures.
Blood tests can, for example, provide clues about metabolic disorders that trigger seizures. Urine tests can also be helpful - for example, to detect drugs that the patient has not reported.
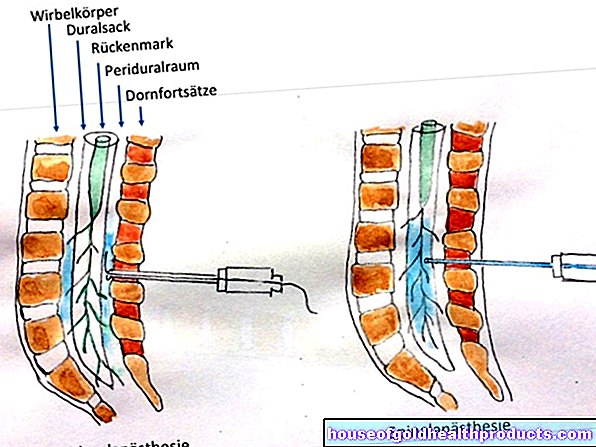
If necessary, further examinations are indicated. This includes, for example, taking and analyzing a sample of the cerebral spinal cord fluid (lumbar puncture) if a brain infection is suspected as the cause of seizures.
Treating a seizure
In the case of seizures, attempts are made to treat the cause. If, for example, hypoglycaemia has triggered the attack, the patient is given glucose (e.g. as an infusion). In addition, if possible, the doctor will treat the reason for the low sugar level (e.g. diabetes).
In most cases, seizures are caused by epilepsy. Long-term, individually tailored treatment may then be necessary to prevent further attacks. Such anti-epileptic therapy can include:
- anticonvulsants (called anticonvulsants or anti-epileptic drugs)
- Avoiding possible triggers (e.g. excessive alcohol consumption, lack of sleep)
- possibly surgical intervention on the brain
Seizure: When should you see a doctor?
Anyone who has ever had a seizure should always consult a doctor - regardless of how severe the attack was. It is important to have the cause clarified. The specialist in charge of seizures is a neurologist.
Sometimes those affected do not even notice that they are having or have just had a seizure (for example in the case of absenteeism). Outsiders who notice should then tell the person concerned.
Tags: menshealth first aid prevention