Back pain
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Back pain is a common ailment of modern civilization: Almost everyone suffers from lower back pain etc. at least once in their life. Fortunately, in about 90 percent of cases the causes are not threatening. Therefore, those affected can do a lot against back pain themselves - from heat packs to exercises against back pain. Read more about the causes and treatment of back pain here.

Brief overview
- Back pain: are among the most common types of pain and mainly affect women. Most often, the pain is in the lower back and is non-specific (no cause can be determined).
- Classification: according to the duration (acute, subacute and chronic back pain), according to the location (upper, middle or lower back) and according to the cause (specific and non-specific back pain).
- Causes: In the case of non-specific back pain, no cause can be determined. On the other hand, specific back pain has a demonstrable trigger (muscle tension, vertebral blockage, ISG syndrome, herniated disc, osteoporosis, pelvic inflammation, myocardial infarction, prostate inflammation, lung tumor, etc.).
- Examinations: depending on the patient, physical examination, blood and urine tests, neurological examination, gynecological examination, electroneurography, electromyography, x-ray, gastroscopy, computed tomography, magnetic resonance tomography (MRT), scintigraphy, cardiac catheter examination, etc.
- Treatment: For specific back pain, treat the cause. For non-specific back pain, heat treatment, medicinal plants, correct bending and lifting, exercise and back-friendly sport, back school, back-friendly workplace, relaxation techniques, acupuncture, possibly medication
Back pain: description & classification
Low back pain, lumbago, stiff back or simply “having it in your back”: back pain is a multifaceted ailment. Sometimes it squeezes in the back, sometimes it pulls in the neck. Sometimes the back pain continues in the flanks, arms, or legs. The symptoms can be persistent or only occur intermittently. Sometimes they are so strong that those affected can barely move.
Those affected are as varied as the type and extent of the complaints: Back pain can plague people of almost any age. They are among the most common pain problems. Women in all age groups report back pain more often than men - a phenomenon that is also evident in other types of pain.
Doctors classify back pain according to various criteria:
Back pain: classification according to location
- Back pain - upper back: Pain that occurred at the top of the spine (neck region) can be acute to chronic. They often radiate in the shoulders, arms and / or the back of the head. Triggers for neck pain are, for example, incorrect posture at work, a slipped disc or psychological influences.
- Back pain - middle back: Back pain in the thoracic spine area is rarely caused by injuries. They are more often triggered by irritation of large muscle groups in this area or by functional disorders of the rib and vertebral joints.
- Back Pain - Lower Back: Back pain is most commonly found in the lower back. Because the lumbar spine (lumbar spine) is more susceptible to injuries and damage than the cervical and especially thoracic spine. Back pain in the lower back is called "lower-back-pain" in English. Possible causes are, for example, slipped discs or overexertion of the muscles.
Back pain: classification according to duration
Depending on the duration of the complaints, doctors differentiate between acute, subacute and chronic back pain:
- Acute back pain: Acute back pain is back pain that occurs for the first time or after at least six pain-free months and lasts for a maximum of six weeks. The prognosis is generally good: Acute back pain improves within a few weeks in the majority of those affected.
- Subacute back pain: If the back pain lasts longer than six weeks up to a maximum of three months, it is considered subacute.
- Chronic back pain: Chronic back pain or chronically recurring (recurrent) back pain last longer than three months. The severity of the pain can vary during this time - sometimes the back pain is weaker, sometimes stronger. Chronic back pain is more common with age.
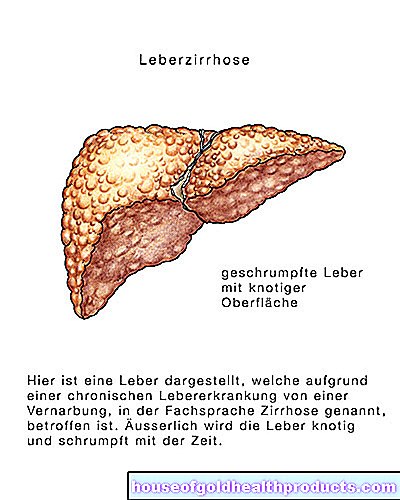
Chronic back pain is usually more than just back pain. Additional illnesses (comorbidities) often occur. These include, for example, wear-related (degenerative) and inflammatory joint diseases, osteoporosis, stroke, cardiac insufficiency, depression, pain medication abuse, severe overweight (obesity) and chronic bronchitis. When a patient with back pain comes to the doctor, the doctor will take such comorbidities into account when assessing and treating the symptoms.
Back pain: classification according to the cause
Depending on whether a clear cause for the symptoms can be proven or not, doctors differentiate between specific and non-specific back pain. Read more about this in the next section.
Back pain: causes
Back pain can be roughly divided into two groups according to its cause: non-specific and specific back pain.
Non-specific back pain
In the case of non-specific back pain, the doctor cannot find a clear cause of the symptoms. The vast majority of all back pain cases fall into this category.
Specific back pain
Specific back pain has a clearly identifiable cause. However, this does not necessarily have to be in the area of the spine (as is the case with a herniated disc). Instead, a wide variety of diseases in other organs are often the reason for the complaints in the back: The spectrum ranges from shingles and pneumonia to kidney stones and heart attacks. Below is an overview of important causes of specific back pain:
- Muscle tension: very often, muscle tension is the cause of back pain. In the case of bad posture, one-sided loads and a lack of movement, the muscles are loaded unevenly - some muscles are overwhelmed, others under-challenged. As a result, muscles shorten or harden, which can lead to tension and pain. A pinched nerve can also result from muscle tension and cause back pain.
- Blockage (vertebral blockage, vertebral misalignment): A tense muscle can pull a vertebra out of its normal position over time. Such a vertebral misalignment or blockage can also occur if one suddenly does something that the body is not used to (such as jerky movements during sport). Vertebral blockages can cause pain in the muscles, the vertebral joints, or the exit canals of the nerves from the spinal cord. Sometimes the pain radiates to the arms or legs.
- Sacroiliac Joint Syndrome (ISG syndrome): ISG syndrome is an example of the vertebral block described above and is quite common. The blockage affects the joint between the sacrum and the pelvic bone, the so-called sacroiliac joint (SIJ) or sacrum-iliac joint. In contrast to other joints in the body, it can only move to a limited extent because it is held tightly together by strong ligaments. In an ISG syndrome, the joint surfaces of the sacroiliac joint shift against each other and block due to increased muscle tension. This can cause back pain.
- Herniated disc: The intervertebral discs lie as cushion-shaped shock absorbers between the individual vertebral bodies. They consist of a soft gelatinous core surrounded by a ring of fiber cartilage. If the gelatinous core slips and the fiber covering breaks through, there is a herniated disc. It causes severe back pain when the gelatinous mass emerging from the slipped intervertebral disc presses on the neighboring nerves.
Most often the sciatic nerve is pinched, more precisely: one of the nerve roots that emerge from the spinal cord in the lumbar vertebrae and sacrum and merge below the pelvis to form the sciatic nerve. This thickest and longest nerve in the body runs on the back of the thigh after multiple branches down to the foot. A pinched sciatic nerve can therefore cause pain that radiates from the buttocks to the back of the leg and into the foot. Such sciatica can have other causes besides a herniated disc. - Wear of the spine (osteoarthritis of the spinal joints, facet syndrome): With increasing age, the spinal joints in the body wear out. If this age-related joint wear goes beyond the normal level, doctors speak of osteoarthritis. Such osteoarthritis of the spinal joints can cause back pain. The symptoms occur especially at the beginning of a movement (for example when getting up in the morning). They slowly subside as you move.
- Spinal canal narrowing (spinal canal stenosis): The spinal canal with the spinal cord within it runs in the spine. This routes nerve signals from the brain to the body and back. In spinal stenosis, the spinal canal is narrowed in places and presses on the spinal cord or the emerging nerve roots. The result is back pain, for example in the area of the sacrum (lower back pain).
- Spine curvature: In what is known as scoliosis, the spine is curved to the side. This leads to premature wear and tear, which can trigger muscle tension and back pain, among other things. In the so-called Scheuermann's disease, too, the spine curves in a characteristic way. The consequences are a hunchback (hunched back), back pain and restricted mobility.
- Spinal inflammation (Bechterew's disease): This is a chronic rheumatic inflammation of the spine and the joint that connects the spine with the iliac bone (sacroiliac joint). The progressive disease triggers deep-seated back pain and can make the joints more and more rigid over time. This is why Bechterew's disease is also called ankylosing spondylitis, which translates as "stiffening vertebral inflammation".
- Slipping of the vertebrae (spondylisthesis): In this disease, the vertebrae are unstable so that they can shift easily. This mainly happens in the lumbar region. Many of those affected have little or no complaints. But back pain can also occur, for example during exercise and certain movements. If a displaced vertebra presses on a nerve root, neurological deficits such as sensory disturbances or paralysis are also possible.
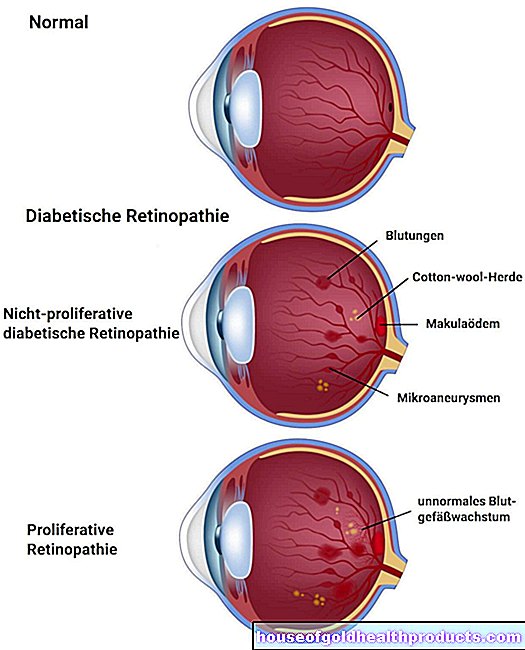
- Osteoporosis (bone loss): With osteoporosis, the bones become increasingly fragile. You can then break even with the slightest stress (such as falling, bumping into). This often leads to vertebral body collapse, which is accompanied by back pain. The preliminary stage of osteoporosis - osteopenia - can also be accompanied by back pain.
- Pregnancy: Many pregnant women have back pain. There are mutliple reasons for this. For example, the hormonal change in pregnant women causes tendons and ligaments in the pelvic floor area to loosen. As a result, you lose stability, which can cause pain in the pelvis and lower back. In addition, the woman's body center of gravity shifts due to the growing unborn child. To compensate, many pregnant women fall into the hollow back. This can also result in back pain. In addition, pre-labor and early labor can also be associated with back pain.
- Shingles: This painful rash is caused by the same virus as chickenpox (variella zoster virus). It usually forms on one side of the trunk, along the spinal cord nerves (for example, where the trouser belt sits). Severe back pain can occur in connection with shingles.
- Acute prostate inflammation (prostatitis): An acute inflammation of the prostate gland (prostate) can cause men not only pain and burning sensation when urinating, but also back pain, among other things.
- Kidney inflammation: Kidney inflammation is usually triggered by bacteria and occurs mainly in women. Especially if it is chronic, it can cause protracted back pain.
- Kidney stones: In contrast to inflammation of the renal pelvis, kidney stones tend to occur in men. Sometimes they are so small (kidney gravel) that they are simply excreted in the urine through the ureter. Larger kidney stones, on the other hand, can get stuck in the ureter. The result is renal colic, which, depending on the location of the kidney stone, can trigger, among other things, stabbing, cramp-like and wavy back pain.
- Chest tightness (angina pectoris): If the heart muscle temporarily receives too little oxygen, this triggers an angina pectoris attack. Frequent signs are pain and tightness in the chest, feelings of oppression, sudden shortness of breath, nausea, vomiting - and back pain.
- Heart attack (myocardial infarction): The pain in the heart area that occurs during a heart attack often radiates to other parts of the body, for example between the shoulder blades in the back.
- Inflammation of the heart muscle (myocarditis): Sometimes an inflammation of the heart muscle is hidden behind back pain. Such myocarditis is usually caused by viruses or bacteria.
- Inflammation of the pericardium (pericarditis): Acute pericardial inflammation can be triggered by pathogens (such as viruses or bacteria), other diseases or heart operations. It causes sharp pain behind the breastbone or in the left rib cage. Sometimes the pain radiates to the shoulder blade region - the patient complains of back pain.
- Expansion of the main artery (aortic aneurysm): The sac- or spindle-shaped expansion of the aorta occurs most frequently in the abdominal area. Such an abdominal aortic aneurysm can lead to back pain, among other things.
- Inflammation of the lungs (pneumonia): In addition to a cough and fever, back pain can sometimes also be attributed to pneumonia. The cause of the inflammation is usually bacteria.
- Lung collapse (pneumothorax): In a pneumothorax, air collects in the narrow space between the lungs and the chest wall (pleural space or pleural space). This can happen spontaneously with no apparent cause, or it can be the result of a disease or injury to the lungs. The lung in question collapses. This can be recognized, among other things, by the sudden onset of pain in the chest area, which can radiate into the back.
- Pulmonary infarction (pulmonary embolism): A pulmonary embolism occurs when a blood clot that has washed up blocks the flow of blood in a pulmonary artery. The result is chest pain, which, as with pneumothorax, continues backwards and can trigger back pain in the chest area (thorax).
- Inflammation of the pleura (pleurisy): pleurisy often occurs as a result of a lung disease such as pneumonia. The dry form of the disease (little fluid in the pleural space = space between the pleura and pleura) is noticeable through severe, stabbing chest pain or back pain.
- Inflammation of the esophagus (esophagitis, reflux disease): Inflammation of the lining of the esophagus mainly causes burning pain behind the breastbone (heartburn). These can radiate into the back.
- Esophageal spasm (esophageal spasm): This leads to spasmodic contractions of the esophageal muscles - spontaneously or triggered by swallowing.The pulp can then no longer be transported towards the stomach. It builds up, causing severe pain behind the breastbone. Even pain in neighboring areas of the body - such as back pain - can be traced back to esophageal spasms.
- Esophageal injuries: If you swallow a foreign body, tears can occur in the esophageal wall in rare cases. Large cracks, caused by violent vomiting as in bulimia, are even rarer. You can express yourself with a sudden, violent pain (annihilation pain) behind the breastbone, which can radiate into the back.
- Inflammation of the pancreas (pancreatitis): Both acute and chronic inflammation of the pancreas cause pain in the upper abdomen. These often radiate backwards in a belt shape and are then perceived as back pain.
- Pancoast tumor: Pancoast tumor is a rare malignant growth on the apex of the lung. Among other things, it can cause back pain, more precisely: discomfort in the cervical spine.
- Spine tumor and rib tumor: Back pain can also be caused by a spine tumor or rib tumor. Sometimes such tumors are benign, sometimes malignant. In the second case, it is almost always daughter tumors of cancerous tumors in other parts of the body, such as breast or lung cancer.
Risk factors for back pain
There are several factors that increase your risk of back pain. Above all, this includes:
- Work-related factors: Carrying and lifting heavy loads, vibrations (as when working with a jackhammer) and working in unfavorable postures put stress on the spine, joints and muscles. In the long run, this can lead to back pain. Therefore, some back diseases are recognized as occupational diseases.
- Work-related psychosocial conditions: Anyone who is dissatisfied with their job or who has to do monotonous work from morning to evening (for example on the assembly line) is more prone to back pain. Social conflicts in the workplace and a high level of work effort without adequate rewards (in the form of money, recognition, opportunities for advancement, etc.) can also lead to back pain.
- Social status: Back pain is more common in people with a low social status in terms of schooling, occupation and income than in people with a high social status.
The course of existing back pain can also be influenced by unfavorable conditions, such as psychological factors. This includes, for example, unrealistic fears about back pain, depression and passive or overactive behaviors - i.e. pronounced relieving posture or too much activity.
Back pain: therapy
In the case of specific back pain, the doctor will treat the cause of the discomfort if possible. For example, in the case of a herniated disc, conservative (non-surgical) therapy is usually sufficient, for example with heat applications, physiotherapy, relaxation techniques and pain relieving or muscle relaxing medication. Surgery is rarely necessary. If the back pain is caused by an inflammation of the kidney pelvis, the doctor will usually prescribe antibiotics. In most cases, bacteria are the cause of the inflammation.
The much more common non-specific back pain is mainly about alleviating the symptoms (symptom treatment). First and foremost, you as a patient are asked: You can do a lot yourself against your back pain (back-friendly behavior, correct movement, warmth, etc.). You may also be able to try alternative healing methods. But be careful with the many guides that are mainly circulating on the Internet. It is best to always discuss a method with a doctor before trying it.
- Attitude: Your mental attitude has a great influence on your health. Your attitude towards back pain greatly influences its course and treatment. Anyone who is convinced that they have to come to terms with the pain, or who thinks of a tumor every time they experience pain, will find it difficult to get rid of the back pain. Therefore, avoid both hopelessness and catastrophe thinking about your back pain.
- Properly bend over, lift and carry: How do you lift a water tank? By bending down with your knees straight and jerking the box up? Not a good idea, because the intervertebral discs are squeezed together in a wedge shape. This one-sided stress causes the intervertebral discs to age faster and become porous in the long run. As a result, the gelatinous core of the intervertebral discs can shift and painfully press on nerve fibers. You can avoid this by always kneeling and keeping your back straight when lifting and setting down loads. When carrying around, you should always keep loads close to your body.
- Back-friendly workplace: If you spend a lot of time at your desk and computer, you should make sure that your workplace is ergonomically designed - so that the work does not cause you health problems over time, e.g. painful tension in the neck and shoulder area, pain in the lumbar spine, arms and joints or tendinitis.
- No excessive rest and bed rest! With acute, non-specific back pain, many patients try to move as little as possible. Some even go to bed. Experts advise against both! Anyone who avoids movements or keeps bed rest for fear of the pain favors the symptoms becoming chronic (chronification). Instead, if you have acute non-specific back pain, you should continue your normal everyday activities. A walk can also be good. The back muscles are loosened and the vertebral joints are gently moved.
- Exercise and sport: Exercise therapy and back-friendly sport are particularly recommended for subacute and chronic non-specific back pain, but not for acute back pain. The term "back-friendly sport" means less specific types of sport. Rather, it depends on the right training dose, a targeted training structure and good technique - then a wide variety of sports can have positive effects on back pain. Targeted strength training is particularly effective for strengthening the core muscles: the stronger the back and abdominal muscles are, the more they help the spine with its support function. Such a strong muscle corset can even prevent back pain. It is best to seek advice from a sports doctor or sports trainer who has experience with back pain patients!
- Special exercises against back pain / back training: Different versions of the squat, arm lifts, mini-crunches and more - exercises like this particularly train flexibility, balance, strength and performance of the back. Following guidance from an experienced trainer (for example in a back school), you should perform the exercises regularly at home. This not only helps against existing back pain. Exercises like the ones mentioned above are generally suitable for strengthening the back and can therefore also prevent back problems. For non-specific back pain, experts consider a back school to be useful if the symptoms persist for more than six weeks or keep recurring. A back school with a biopsychosocial approach should be chosen: Here the body is not viewed as a purely mechanical construct. Instead, one takes into account that health (or back pain) is also influenced by psychological, emotional and social factors.
- Relaxation procedures: Progressive muscle relaxation (PMR) is recommended by experts for acute and subacute non-specific back pain when there is a high risk that the symptoms will become chronic. The targeted relaxation helps against stress and tension (both play an important role in back pain). If the pain is already chronic, PMR can also be useful. There are also other relaxation methods such as autogenic training and meditation. Many back patients have also had positive experiences with it.
- Holistic exercise methods: Yoga, Qi Gong and Tai Ji Quan also have a relaxing effect. These holistic exercise methods are also suitable for preventing lumbago and herniated discs. In the case of painful muscle tension due to incorrect movement patterns, you can try the Alexander Technique or the Feldenkrais Method: Both methods will help you get used to unhealthy movement patterns again.
- Heat treatment: Heat applications (e.g. in the form of hot water bottles, heat packs, mud baths, fango packs) relax the muscles and can provide relief for non-specific back pain. This also applies to acute complaints. Experts recommend combining heat treatment with activation (i.e. movement). This can significantly improve the pain.
- Medicinal plants: Combination preparations made from ash and quivering aspen can relieve back pain. In the case of painful muscle tension, a cream or plaster with capsaicin helps: The hot substance from different types of peppers has a local effect on blood circulation (and thus warming). In combination with activating measures (movement), this can alleviate non-specific back pain. If stress-related, nervous tension is (partly) responsible for the back pain, you should drink valerian tea. It relaxes both the mind and the muscles.
- Aromatherapy: For lumbago (lower back pain), you can rub the affected area with pine, sandalwood or ginger oil. This can help alleviate the discomfort.
- Homeopathy: For acute back pain, homeopaths recommend, for example, Aconitum C30 (acute lumbago after exposure to the cold), Arnica D12 (back pain after overexertion or lifting) or Nux vomica C30 (nervous tension and tension). The homeopath will advise you on the selection and dosage of the preparations.
- Schüssler salts: Ferrum phosphoricum D6 is said to relieve acute back pain. To do this, the tablets are dissolved in hot water, which is then drunk in sips. If you suffer from lumbago more often, you can try Calcium floratum 6X (take for several weeks). It is best to ask a naturopath or doctor with experience in the field of Schüssler salts about the selection and dosage of the remedies.
- Bach flower therapy: If there is psychological tension behind the back pain, taking Bach flowers can help: So, for example Rock water Recommended if there is a lack of flexibility and rigid adherence to principles. Oak is used on the other hand when someone demands a lot of himself and is never satisfied with himself. Advice from a Bach flower expert will help you choose the right remedy.
- Traditional Chinese Medicine: TCM experts see lumbago and herniated discs as a weakness of kidney qi or kidney yang. With acupuncture and herbal treatments, the patient's kidneys are strengthened. Acupuncture and moxibustion of the bladder meridian can also be helpful. According to conventional medicine, acupuncture can be tried for chronic non-specific back pain and in certain cases of acute non-specific complaints (e.g. if conventional medical treatments do not help).
- Ayurveda: Low back pain (lumbago, lumbago) should be seen as an excess of Vata from the point of view of an Ayurveda expert. Vata-reducing oil massages and herbal oil enemas should quickly remedy this.
- Back-friendly nutrition: bones, joints, muscles and intervertebral discs need a lot of nutrients in order to be able to perform their tasks. You should therefore ensure that you have a sufficient supply of essential fatty acids, calcium, fluoride, vitamins C, D and E as well as B vitamins, magnesium, boron, selenium and zinc. This is not only good for your back, it also promotes general health.
- Drink a lot: The nutrient supply of the intervertebral discs only works with plenty of fluids. This is the only way to keep the small shock absorbers between the vertebral bodies healthy and elastic. In addition, studies show how important sufficient fluid intake is for back pain: If you drink about two liters of water a day, you can often relieve your pain with it.
Experts advise against this
There are also methods that, in the opinion of experts, are not suitable for treating certain back pain. For example, cold treatment, magnetic field therapy and kinesio taping are not recommended for non-specific back problems. In the case of acute non-specific back pain, patients should refrain from both massage and occupational therapy.
Back pain medication
Any physical activity can be painful for non-specific back pain. In the case of acute complaints, many patients therefore want to move as little as possible. In the case of subacute and chronic non-specific back pain, some sufferers refuse exercise and sports therapy recommended by their doctor due to pain.
In such cases, medication can be useful: They alleviate the back pain to such an extent that physical activity is possible again. Over time, the dose of medication should and can be reduced: As the level of training increases, patients usually need less medication in order to move (almost) painlessly. The doctor will give each patient precise instructions on when a drug can be used, in what dosage and for how long. Patients should follow these instructions to avoid side effects or habituation effects.
Pain therapy can also be useful and necessary for specific back pain. Usually it is only carried out for a short time.
In principle, different groups of active substances are available for the treatment of back pain. It depends on the type and severity of the complaints which preparation is best suited in each individual case:
- conventional pain relievers (analgesics) such as ibuprofen or diclofenac
- very strong painkillers from the group of opiates, also called opioids (opioid analgesics). In the case of severe back pain, for example after a herniated disc, they are often the first aid to enable the patient to move again.
- Muscle relaxants (muscle relaxants): not recommended for non-specific back pain
- certain antidepressants, e.g. for chronic non-specific back pain, if the patient is simultaneously suffering from depression or a sleep disorder
Some of these drugs require a prescription, so they have to be prescribed by a doctor. Painkillers also include preparations that are available without a prescription (e.g. with pain relievers such as ibuprofen or acetylsalicylic acid). Nevertheless, you should discuss their use and possible side effects with your doctor in advance.
Herbal supplements are also offered to relieve back pain. For example, with chronic non-specific back pain, taking willow bark extracts (capsules, tablets, etc.) can help - in combination with activating measures (such as exercise therapy).
Back pain: when do you need to see a doctor?
Back pain is not always a sign of a more or less severe illness that requires a doctor's visit. Often there are relatively harmless causes behind it, for example muscle tension due to lack of exercise or incorrect posture. To be on the safe side, you should see a doctor in the following cases:
- untypical back pain
- persistent back pain
- increasing back pain
Back pain: examinations
To clarify back pain, the doctor will first talk to you in detail to collect your medical history (anamnesis). Possible questions are:
- Where does the back pain occur?
- Does the back pain radiate to other parts of the body (for example to the flanks or into a leg)?
- How long has the current pain episode been going on?
- Have there been previous episodes of back pain? How was the pain?
- Are there factors that trigger, aggravate or alleviate back pain (such as warmth, cold, movement, etc.)?
- How has the back pain been treated so far (medication, massages, etc.)? Were the measures successful? Did you experience any side effects?
- What does the (diurnal) time course of the back pain look like?
- How bad is your back pain? Do they interfere with everyday activities?
- Do you have accompanying complaints or illnesses of a mental or physical nature?
The doctor will also ask what you think about your pain (for example, a pessimistic attitude). Your pain behavior is also important, i.e. whether you move as little as possible for fear of the symptoms. In addition, the doctor asks about possible psychosocial risk factors such as stress, conflicts at work or a tendency to depression.All this information can be used to estimate, among other things, how great the risk is that your back pain will become chronic.
Medical examinations
After the anamnesis discussion, the doctor can carry out various tests to get to the bottom of the causes of the back pain.
- Physical examination: The doctor pays attention to incorrect or relieved postures, for example. These often give an important indication of the cause of the complaints. If shingles (herpes zoster) is the trigger for the back pain, the doctor will recognize this from the typical skin rash.
- Orthopedic examination: It is especially indicated for the more detailed clarification of lower back pain (lumbago, lumbago).
- Blood test: The measurement of various blood values can, for example, indicate spinal column wear, inflammation (such as pleurisy, prostate inflammation, kidney inflammation) or heart attack as a trigger of back pain.
- Urine examination: The analysis of a urine sample can remove or substantiate the suspicion of a kidney disease or an acute inflammation of the prostate.
- Gynecological exam: This is due for pregnant women who have back pain that may be signs of labor.
- Neurological examination: The functional and conduction state of nerve tracts is examined if the cause of the back pain could be a narrowing of the spinal cord or nerve roots (e.g. in the case of a herniated disc).
- Electronurography (ENG): Examining the nerve conduction in the arms and / or legs can provide evidence of a herniated disc.
- Electromyography (EMG): The measurement of the electrical activity of a muscle is also used to clarify a herniated disc as a possible cause of back pain.
- Ultrasound examination: If the back pain is caused by an inflammation of the kidney pelvis or by kidney stones, an ultrasound (sonography) can provide certainty.
- Excretory urography: With an X-ray examination of the lower urinary tract with the help of a contrast medium, kidney stones can be proven as the cause of back pain.
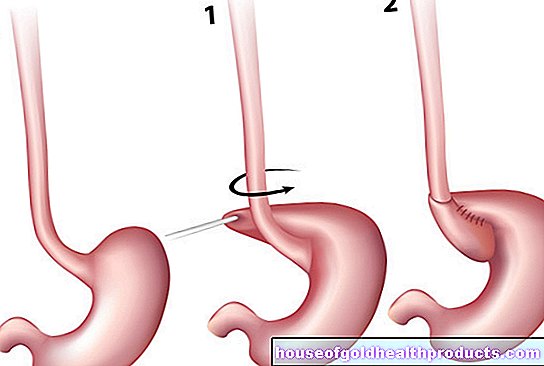
- Gastroscopy: A gastroscopy is done when the cause of back pain may be in the esophagus (esophagitis, esophageal spasm, tear in the esophagus).
- X-ray: A simple X-ray examination can provide information about various possible causes of back pain such as pneumonia, pneumothorax, spinal column wear, spinal inflammation (ankylosing spondylitis) or osteoporosis.
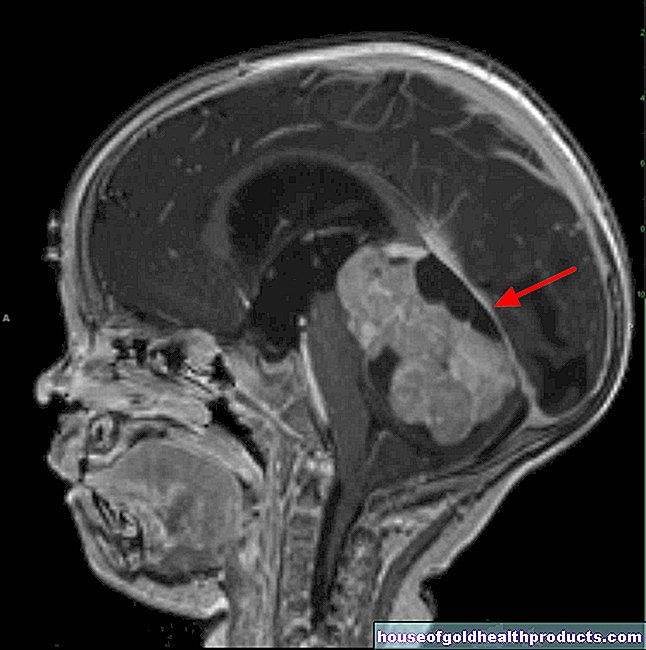
- Computed tomography (CT) scan: This is done when there is suspicion that the back pain is being caused by a herniated disc, spinal wear, an aortic aneurysm, inflammation of the pancreas, or a lung tumor.
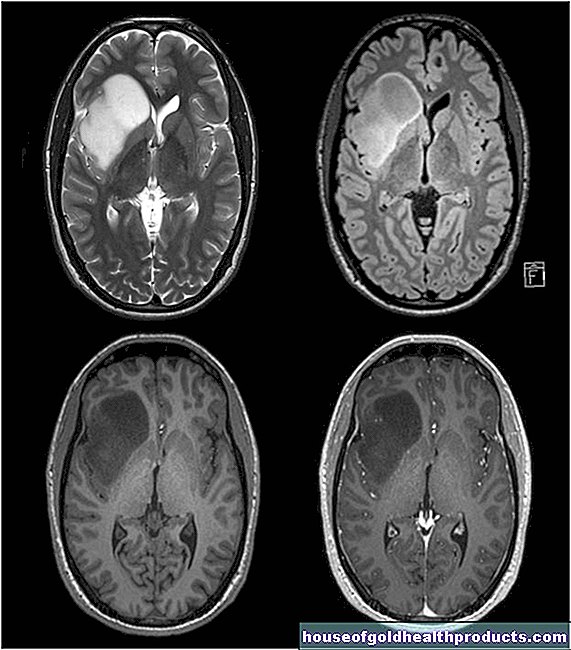
- Magnetic resonance imaging (MRT): This examination, also known as magnetic resonance imaging, can be used to investigate suspected herniated discs or spinal infections (ankylosing spondylitis).
- Scintigraphy: In this nuclear medicine examination, the activity status of various tissues is determined, for example bone tissue (bone scintigraphy: if ankylosing spondylitis is suspected) or lung tissue (lung scintigraphy: if pulmonary embolism is suspected).
- Electrocardiography (EKG): The electrical activity of the heart muscle is examined if a heart disease (angina pectoris, heart attack, myocarditis, pericarditis) is suspected to be the cause of back pain.
- Cardiac ultrasound: an echocardiography is indicated if an inflammation of the heart muscle or pericardium could be responsible for the back pain.
- Cardiac catheter examination: A cardiac catheter is placed if angina pectoris is suspected.
When and which examinations are necessary
The physical examination and laboratory tests (blood, urine) are part of the routine program when diagnosing back pain. In contrast, radiological examinations - i.e. x-rays, computed tomography (CT) and magnetic resonance imaging (MRI) - are only recommended if specific back pain is suspected. In the initial diagnosis of acute and uniformly chronic back pain, this is deliberately avoided: Too many examinations can stir up fear in the patient that there may be a serious cause behind the back pain that has just not yet been found. This can contribute to acute back pain becoming chronic (chronification).
The other very special examinations such as cardiac catheters or scintigraphy are also only carried out in certain suspected cases of patients with back pain.
Tags: prevention teeth Diseases