Tracheotomy
All content is checked by medical journalists.An incision in the windpipe, also known as a tracheotomy, is a surgically created access to the windpipe. It is carried out to secure the airways in special situations, especially in patients who have to be ventilated for a long time. Read all about the tracheal incision, when to use it and the risks it entails.

What is a tracheotomy?
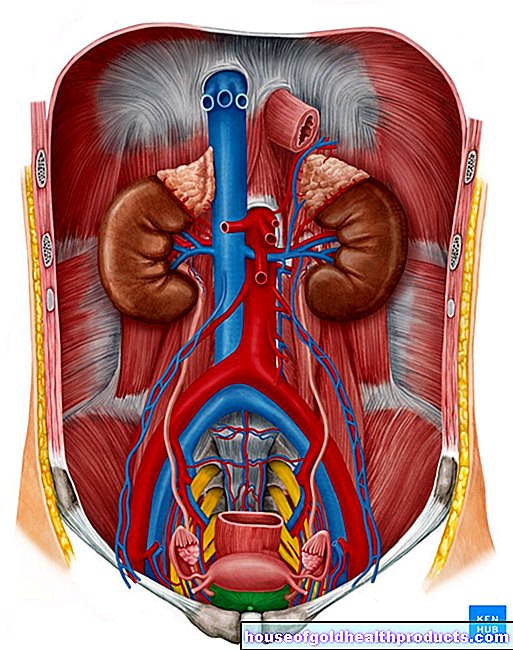
The surgical opening of the windpipe (trachea) is called a trachea incision. The doctor secures this access with a metal or plastic cannula. The opening of the windpipe created in this way is called a tracheostoma.
Various procedures are available for access to the trachea: A distinction is made between the standard tracheotomy and the dilated tracheal incision.
After a tracheal incision, the patient can only speak if a special speaking cannula has been inserted. These are windowed on the back wall so that the air flows into the upper larynx when you exhale. This enables the patient to speak.
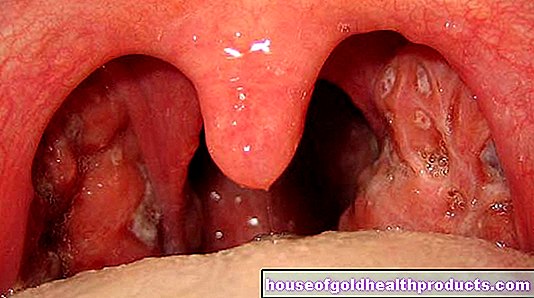
The tracheal incision is often confused with the cricothyrotomy, in which the connecting tissue between the cricoid and thyroid cartilage of the larynx is pierced. In contrast to the "real" trachea incision, the cricothyrotomy is only performed in emergency situations with an acute risk of suffocation, when other ventilation methods are no longer possible - for example if the throat is swelling due to an allergic reaction or something has been inhaled into the trachea.
When do you perform a tracheal incision?
Often, patients who are likely to have to be artificially ventilated over a longer period of time receive an incision in the trachea (coma, chronic weakness of breath and others). Other situations where a tracheotomy is necessary include:
- Narrowing canker sores in the nose and throat
- Midface injuries
- Skull base fracture
- Malformations and injuries to the nasal passages, larynx and throat where tube ventilation is not possible
- Nerve injuries associated with swallowing disorder
The advantage of a tracheal incision compared to ventilation via intubation is that the risk of injuring the vocal cords, the nose or the larynx is significantly lower during the procedure. In addition, the patient does not have as strong a foreign body sensation as with the tube that is placed over the nose or mouth. Eating is also easier for such patients. One disadvantage, however, is that it is an operation that is not carried out in the hospital room, but under sterile conditions.
What do you do with a tracheotomy?
Before the trachea incision is made, the patient is given general anesthesia by the anesthetist so that they can survive the procedure asleep and without pain. In some cases, local anesthesia is sufficient. Then the surgeon disinfects the skin of the neck and covers the patient with sterile cloths, leaving out the neck region.
Standard tracheotomy
The doctor opens the trachea with a cross section in the upper third. To do this, he also removes a small piece of the cartilage. He introduces a metal or plastic cannula into the opening created in this way, which keeps the access created open. To prevent it from slipping, the doctor then fixes the cannula in place with sutures or a collar.
Dilated tracheotomy
With a dilated trachea incision, the doctor punctures the skin and then pushes this puncture site apart with scissors until it hits the trachea. He punctures this with a needle and inserts a wire into the windpipe. He pushes a so-called dilator over this wire, with which the opening is expanded. Now he introduces the cannula.
What are the risks of a tracheotomy?
Ventilation through an incision in the trachea carries the following risks:
- Cardiac arrest
- The cannula is blocked or slipped
- Cannula misplacement
- Bleeding
- Air accumulation in the pleural space, possibly with compression of the lungs
- Air accumulation in the middle layer of the thoracic cavity
- Wound infection
- Connection between the esophagus and windpipe (tracheoesophageal fistula)
- Closure of the trachea
- Narrowing of the windpipe (tracheal stenosis)
The longer a patient needs the tracheostomy, the greater the likelihood that these problems will occur.
What do I have to consider after a tracheotomy?
After an incision in the windpipe, the air no longer flows through your mouth and nose into your lungs, but directly into the windpipe via the cannula. This significantly limits your sense of smell and taste. The cannula also makes swallowing difficult because it weighs down the larynx. This can cause saliva to build up and block the cannula. Therefore, the saliva has to be sucked out regularly.
As soon as you no longer need to be ventilated through the tracheostoma, the doctor can remove the cannula. This usually happens when you breathe out; anesthesia is usually not necessary.
After a standard tracheotomy, the wound can either be surgically closed with sutures or it will heal on its own after a while. The dilated tracheotomy does not require a suture; the wound usually heals faster than a standard tracheotomy. A permanently visible scar in the neck region remains after a tracheal incision.
Tags: digital health alcohol alternative medicine