ICSI: Intracytoplasmic Sperm Injection
Nicole Wendler holds a PhD in biology in the field of oncology and immunology. As a medical editor, author and proofreader, she works for various publishers, for whom she presents complex and extensive medical issues in a simple, concise and logical manner.
More about the experts All content is checked by medical journalists.ICSI (intracytoplasmic sperm injection) is the most commonly used method of artificial insemination. In principle, a single fertilizable sperm and egg cell is sufficient for this. Here you can find out more about the ICSI process and why fertilization succeeds in most cases, but the chances of a successful pregnancy are still significantly lower.

What is the ICSI?
The abbreviation ICSI stands for "intracytoplasmic sperm injection". This means that a single sperm is injected directly into the interior of the cell (cytoplasm) of the previously removed egg cell with the help of a fine pipette. The procedure mimics the natural penetration of the sperm into the egg. However, the entire process takes place outside the body (extracorporeal) and is checked under the microscope.
How does the ICSI work?
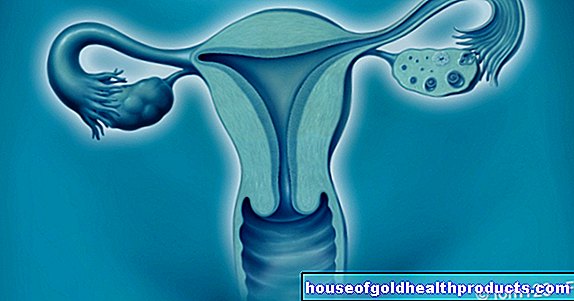
Before ICSI, hormonal stimulation of the ovaries (ovarian stimulation) is necessary in order to stimulate the maturation of several follicles. There are various methods for this with different hormone preparations.
Ovulation and egg retrieval
If there are enough follicles after ovarian stimulation, ovulation is triggered hormonally - the woman is injected with human chorionic gonadotropin (hCG), whereupon the mature follicles each release a fertilizable egg. The ovaries are punctured about two days later. Under ultrasound control, the doctor removes the egg cells from the ovary using a thin needle through the vagina. The woman receives a light anesthetic for this.
Semen sample
On the day of egg retrieval, fresh or processed, frozen sperm must be available - for example from a sperm donation. The reproductive medicine specialist selects a suitable sperm cell for ICSI based on appearance, shape and mobility.
Variant PICSI
A relatively new variant for the selection of suitable sperm cells is based on the ability of the sperm to bind to the enzyme hyaluronidase. During reproduction, it ensures that the egg shell dissolves when the sperm heads come into contact with the egg cell. This physiological variant of ICSI, or PICSI for short, is intended to identify mature and genetically perfect sperm cells. Only in the second step are the morphological criteria taken into account when making the decision. This selection method is intended to further improve the ISCI success rate.
Sperm Injection and Transfer
In the laboratory, the sperm cell is injected directly into the egg cell's cytoplasm using a pipette. After this microinjection, the fertilized egg ends up in the incubator for two to four days. This shows whether the ICSI was successful: If the cell continues to develop through cell division, nothing stands in the way of the ISCI transfer of the embryo into the uterus.If several egg cells have been fertilized in this way, only two embryos should be transferred through the vagina into the uterus in order to avoid multiple pregnancies as far as possible. The remaining egg cells can be stored thanks to cryopreservation - for a possible further attempt (if the first fails) or a second pregnancy.
ICSI: duration
The entire procedure takes a maximum of 20 days. For a first pregnancy test according to ICSI you have to wait about five weeks. If the ICSI was successful, you can use special pregnancy calculators to determine the due date. Whether ICSI or IVF: The basis for calculation is the date of egg retrieval or the day on which a cryopreserved sample was thawed.
Who is ICSI suitable for?
The ICSI treatment is particularly suitable for couples in whom the man's limited fertility has hitherto prevented the desire for children because the sperm contains no or only very few fertilizable sperm.
Reasons for this can be antibodies against sperm, missing sperm ducts, blocked sperm passages or impaired sperm cell production in the testes. If there are no sperm cells in the ejaculate at all (azoospermia), these can possibly be obtained from the testicles or epididymis (TESE or MESA) through an operation. Even after cancer therapy, if only frozen (cryopreserved) sperm cells are available, the ICSI promises success.
The ICSI can also help if the cause of the unfulfilled desire to have children cannot be clarified (idiopathic sterility) or if both partners have a fertility disorder. Sometimes ICSI is also a good method of artificial insemination for older couples.
ICSI chances of success
In principle, one egg and one sperm cell are sufficient for an ICSI. Therefore, for example, the ICSI success rate is also good for men with few sperm in the ejaculate or poor sperm quality. Fertilization occurs in over 70 percent of the egg cells.
The further course after the ICSI - i.e. the chances of a successful pregnancy - cannot be predicted with certainty in individual cases. Individual factors such as fertility and the age of the woman influence the ICSI success rate. After transfer to the uterus, about 15 to 20 percent of women become pregnant.
To do this, many steps have to work together smoothly. However, ovarian stimulation does not always work, a fertilized egg cell does not always develop further, and the egg cell does not always lodge in the uterus (uterus). However, once the fertilized egg has found its place in the uterus, the chances of a normal pregnancy, as with any other pregnancy, are quite good. The slightly increased miscarriage rates are mostly attributed to the advanced age of the expectant mothers.
Assisted hatching
A new method to improve the chances of success of an ICSI (or also In-Vitro-Fertilization, IVF) is the "Assisted Hatching". After the egg cell has been artificially fertilized and the embryo has been created through cell division, it has to implant itself in the uterine lining on about the fifth day. However, this can only succeed if the shell that surrounds the embryo (the so-called zona pellucida) is thin enough that the embryo can slip out of it.
This "hatching" can be difficult in some cases, for example if the shell is too thick or too hard. Under certain circumstances, "assisted hatching" is used here: the zona pellucida of the egg cell is thinned a little at one point with a special laser. This allows the embryo to penetrate the layer and implant itself in the uterus.
In some studies, "assisted hatching" increased the pregnancy rate. But there are also studies in which no such benefit of the laser treatment could be proven.
Advantages and disadvantages of ICSI
The advantage of ICSI is the low need for raw material. The ICSI is a sensible method, especially for men with a poor sperm analysis, because in the best case one single potent sperm cell is sufficient for a successful artificial insemination. If a surgical procedure (TESE / MESA) is necessary for the collection of semen, it should be remembered that there are certain complication risks associated with it (see here).
For women, ICSI treatment begins with hormonal stimulation of the ovaries. This can be very physically demanding. In the worst case, an overstimulation syndrome develops, which can be life-threatening. There is also a low risk of infection or injury after the ovaries have been punctured - i.e. the egg cells have been removed for ICSI.
Tags: Menstruation book tip nourishment




-infektion.jpg)