disc prolapse
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
A herniated disc (disc prolapse, disc prolapse) occurs most often in people between the ages of 30 and 50. Often it does not cause any discomfort. But it can also cause severe back pain, sensory disturbances and even paralysis - then acting quickly is important. Read everything about symptoms, examinations and therapy of a herniated disc here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. G55M50M51
Herniated Disc: Brief Overview
- Possible symptoms: depending on the height and extent of the incident, e.g. back pain that can radiate into a leg or arm, sensory disturbances (pins and needles, tingling, numbness) or paralysis in the leg or arm in question, bladder and bowel emptying disorders
- Causes: mostly age-related and stress-related wear and tear, as well as lack of exercise and obesity; less often injuries, congenital misalignments of the spine or congenital weakness of the connective tissue
- Examinations: Physical and neurological examination, computed tomography (CT), magnetic resonance imaging (MRT), electromyography (EMG), electroneurography (ENG), laboratory tests
- Treatment: Conservative measures (such as light to moderate exercise, sport, relaxation exercises, heat application, medication), surgery
- Prognosis: Symptoms usually go away on their own or with the help of conservative therapy; Surgery is not always successful, complications and relapses are also possible
Herniated Disc: Symptoms
In some patients, a herniated disc triggers symptoms such as pain, tingling or pins and needles in the arms or legs, numbness, or even paralysis in the extremities. The reason for the complaints is that the inner core of the intervertebral disc protrudes and presses on nerves in the spinal canal.
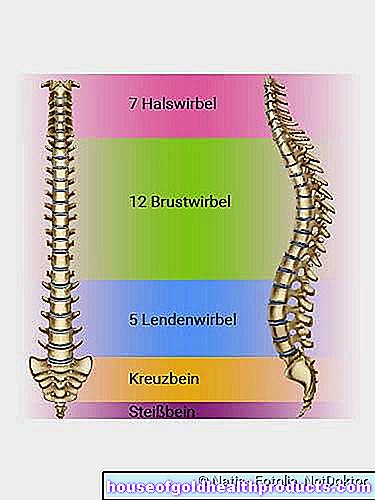
Spinal segments
Symptoms don't always appear
Not every herniated disc triggers symptoms such as pain or paralysis. It is then often only discovered by chance during an investigation.
If a herniated disc causes symptoms, this indicates that the slipped disc is pressing against individual nerve roots, the spinal cord or the nerve fiber bundle in the lumbar spine (cauda equina = horse's tail).
Disc herniation anatomy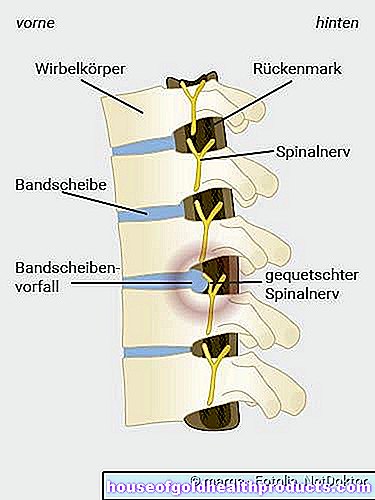
Herniated disc symptoms when pressure is applied to nerve roots
The herniated disc symptoms when pressure is applied to a nerve root depends on the height at which the affected nerve root is located - in the lumbar, thoracic or cervical spine.
Herniated Disc - Lumbar Spine:
Symptoms of a herniated disc almost always originate in the lumbar spine, because the body weight here exerts particularly strong pressure on the vertebrae and intervertebral discs. Doctors speak of a lumbar disc herniation or "lumbar disc herniation". Symptoms usually arise from herniated discs between the 4th and 5th lumbar vertebrae (L4 / L5) or between the 5th lumbar vertebra and the 1st coccyx vertebra (L5 / S1).
The pressure on nerve roots in the lumbar spine sometimes causes severe pain in the lower back, which can radiate into the leg (along the supply area of the nerve root concerned). Neurological deficits such as sensory disturbances (such as pins and needles, numbness) and paralysis in this area are possible.
It is particularly uncomfortable when the sciatic nerve is affected by the lumbar disc herniation. It's the thickest nerve in the body.It is composed of the fourth and fifth nerve roots of the lumbar spine and the first two nerve roots of the sacrum. The pain of being pinched is often described by patients as shooting or electrifying. They run from the buttocks over the back of the thigh down to the foot. The symptoms are often aggravated by coughing, sneezing or moving. Doctors refer to this symptom as sciatica.
Herniated disc - cervical spine:
Occasionally, a herniated disc occurs in the cervical area (cervical disc herniation or herniated disc in the cervical spine). It preferably affects the intervertebral disc between the 5th and 6th or the 6th and 7th cervical vertebrae. Doctors use the abbreviations HWK 5/6 or HWK 6/7 for this.
Symptoms of a herniated disc in the cervical area may include pain radiating into the arm. Paresthesia (paresthesia) and deficiency symptoms (muscle paralysis) in the area where the affected nerve root spreads are also possible symptoms.
Herniated disc - thoracic spine:
A herniated disc is extremely rare in the thoracic spine. The diagnosis here is "thoracic disc herniation" (or in short: "herniated disc thoracic spine"). Symptoms can be back pain, which is mostly limited to the affected part of the spine. The pain rarely radiates into the supply area of the compressed nerve.
Slipped disc symptoms when pressure is applied to the spinal cord
The spinal cord extends from the brain stem to the first or second lumbar vertebra. If a herniated disc presses on the spinal cord, intense pain in a leg or arm as well as sensory disturbances (pins and needles, numbness) can occur. Increasing weakness in both arms and / or legs are also possible consequences of a herniated disc. Signs that the herniated disc is pressing on the spinal cord can also be dysfunction of the sphincter muscles of the bladder and bowel. They are accompanied by numbness in the anal and genital areas and are considered an emergency - the patient must be hospitalized immediately!
Slipped disc symptoms when pressure is applied to the horse's tail
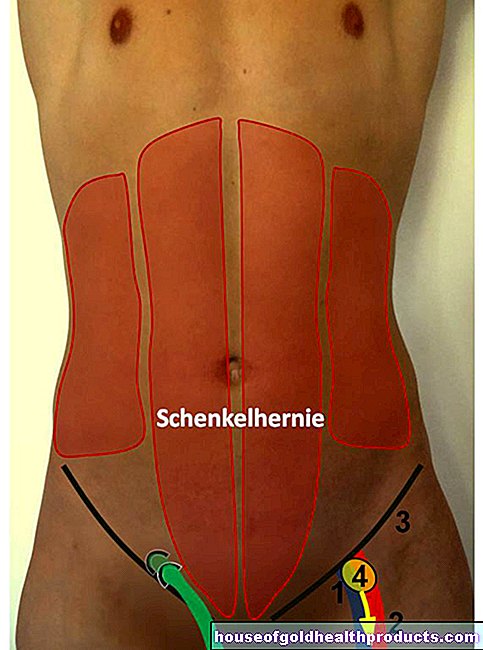
The spinal cord continues at the lower end in a bundle of nerve fibers, the horse's tail (cauda equina). It extends to the sacrum, an extension of the spine.
Pressure against the horse's tail (cauda equina syndrome) can cause problems with urination and bowel movements. In addition, those affected no longer have any sensation in the area of the anus and genitals or on the inside of the thighs. Sometimes even the legs are paralyzed. If you have such symptoms, you must go to the hospital immediately!
Suspected herniated disc symptoms
A herniated disc does not always trigger symptoms such as back pain - even if the X-ray shows an incident. Sometimes tension, spinal changes (e.g. due to wear and tear, inflammation) or neurological diseases are the cause of alleged herniated disc symptoms. Pain in the leg is also not a clear sign - a slipped disc with pressure on a nerve root is just one of several possible explanations. Sometimes there is a blockage of the joint between the sacrum and the pelvis (sacroiliac joint blockade). In most cases, leg pain in back pain cannot be assigned to a nerve root.
-
Herniated disc - targeted movement can prevent it
Three questions for
Dr. med. Samer Ismail,
Specialist in neurosurgery -
1
Back pain is not necessarily a sign of disc problems. What are the symptoms of a herniated disc?
Dr. med. Samer Ismail
In fact, around 60 percent of the population suffer from back pain without a herniated disc. However, if the pain radiates into the leg, those affected should see a doctor. Sensory disturbances such as pins and needles, tingling or numbness are often typical of a herniated disc.
-
2
What helps with a herniated disc?
Dr. med. Samer Ismail
Of course, that depends on how severe the damage is and whether the herniated disc is acute. In the long term, targeted movement is particularly important: stretching and stretching exercises, isometric training with building up the deep muscles, stabilizing exercises and then building muscles on the device. An operation only makes sense if there are signs of paralysis and / or severe pain that persists for more than six months.
-
3
How can I prevent a herniated disc?
Dr. med. Samer Ismail
It is important to take action before symptoms appear. It is helpful to strengthen the back extensors. They form the deepest of the three back muscle layers and stabilize the spine. Instead of using heavy weights, it is better to use cable pulls, a Theraband or your own weight to build up muscles. And do without sports with monotonous movement sequences such as golf or weightlifting.
-
Dr. med. Samer Ismail,
Neurosurgery specialistHead of the Munich East Spine Center and chief physician of the Neurosurgery Center there, specializing in minimally invasive surgical techniques on the spine, intervertebral disc prosthetics and stabilization and correction of the spine
Herniated disc: examinations and diagnosis
If you have unclear back pain, the first thing you should see is your family doctor. If you suspect a herniated disc, he can refer you to a specialist. This can be a neurologist, neurosurgeon, or orthopedist.
In order to determine a herniated disc, it is usually sufficient to question the patient (anamnesis) as well as a thorough physical and neurological examination. Imaging procedures (such as MRI) are only necessary in certain cases.
Doctor-patient conversation
In order to clarify the suspicion of a herniated disc, the doctor will first collect the patient's medical history (anamnesis). For example, he asks:
- What complaints do you have? Where exactly do they occur?
- How long have the symptoms existed and what triggered them?
- Does the pain worsen if, for example, you cough, sneeze, or move?
- Are you having problems urinating or defecating?
The information helps the doctor to narrow down the cause of the symptoms and to estimate from which point on the spine they may originate.
Physical and neurological examination
The next step is physical and neurological examinations. The doctor carries out tactile, tapping and pressure examinations in the area of the spine and back muscles in order to discover abnormalities or pain points. It also tests the range of motion of the spine. Muscle strength, the feeling in the affected arms or legs and the reflexes are also tested. The type and location of the symptoms often give the doctor an indication of the height of the spine at which a herniated disc is present.
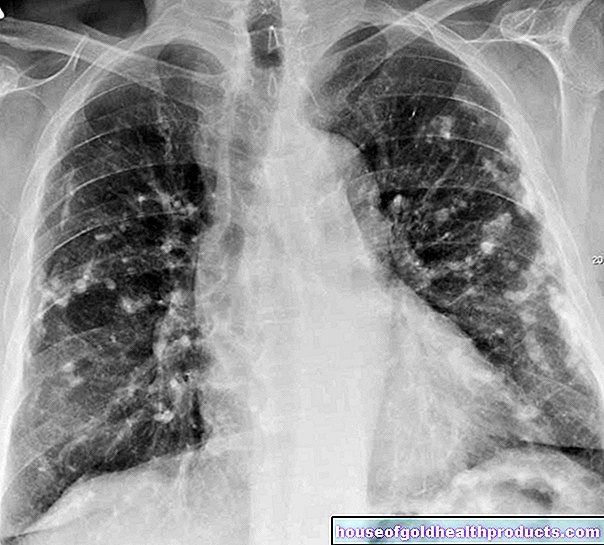
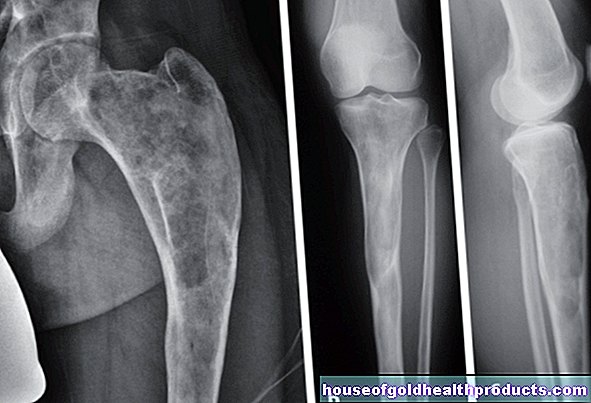
Imaging procedures
Computed tomography (CT) and magnetic resonance imaging (MRI) can make a herniated disc visible. The doctor then recognizes, for example, the extent of the incident and in which direction it occurred: In most cases, there is a mediolateral disc herniation. In the process, the jelly-like nucleus that has emerged has slipped between the intervertebral holes and the spinal canal.
A lateral herniated disc can be recognized by the fact that the gelatinous nucleus has slipped sideways and emerges into the intervertebral orifices. If he presses on the nerve root of the affected side, one-sided complaints result.
A medial disc herniation is less common: the gelatinous mass of the disc nucleus emerges in the center backwards in the direction of the spinal canal (spinal canal) and can press directly on the spinal cord.
When are imaging tests necessary for a herniated disc?
A CT or MRI is only necessary if a consultation with a doctor or physical examination has revealed evidence of a clinically significant herniated disc. This is the case, for example, if paralysis occurs in one or both legs, bladder or bowel function is disturbed, or severe symptoms persist for weeks despite treatment. MRI is usually the first choice.
Imaging is also needed if back pain has symptoms that suggest a possible tumor (fever, night sweats, or weight loss). In these rare cases, it is necessary to visualize the space between the spinal cord and the spinal cord sac (dural space) with an X-ray contrast medium (myelography or myelo-CT).
A normal X-ray examination is usually not useful if a herniated disc is suspected, as it can only show bones, but not soft tissue structures such as intervertebral discs and nerve tissue.
Imaging methods are not always helpful
Even if a herniated disc is discovered in the MRI or CT scan, it does not have to be the cause of the symptoms that prompted the patient to see a doctor. In many cases, a herniated disc runs without symptoms (asymptomatic).
In addition, imaging tests can help make the patient's pain chronic. Because looking at a picture of your own backbone can obviously have a negative psychological effect, as studies show. Especially with diffuse back pain without neurological symptoms (such as sensory disturbances or paralysis) one should therefore first wait. An imaging examination is only indicated if the symptoms do not improve after six to eight weeks.
Insightful pictures of the spine
Measurement of muscle and nerve activity
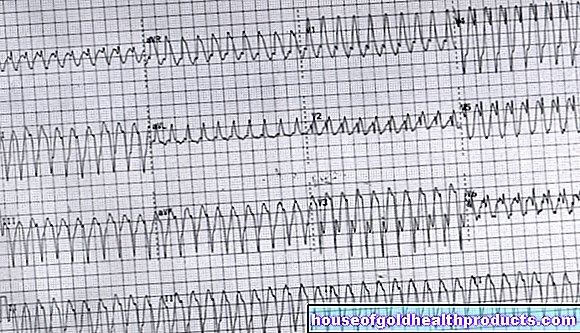
If paralysis or sensory disorder occurs in the arms or legs and it is unclear whether this is the direct result of a herniated disc, electromyography (EMG) or electroneurography (ENG) can provide certainty. With the EMG, the attending physician uses a needle to measure the electrical activity of individual muscles. In cases of doubt, the ENG can reveal which nerve roots are being squeezed by the herniated disc or whether there is another nerve disease, for example a polyneuropathy.
Laboratory tests
In rare cases, certain infectious diseases such as Lyme disease or herpes zoster (shingles) can cause symptoms similar to a herniated disc. If the imaging shows no results, the doctor can therefore take a blood sample and possibly also a sample of the cerebrospinal fluid (cerebrospinal fluid) from the patient. These samples are examined in the laboratory for infectious agents such as Borrelia or herpes zoster viruses.
The doctor can also arrange for general parameters in the blood to be determined. These include inflammation values such as the number of leukocytes and C-reactive protein (CRP). These are important, for example, if the symptoms could also result from an inflammation of the intervertebral disc and adjacent vertebral bodies (spondylodiscitis).
Herniated disc: treatment
Most patients are primarily interested in: "What to do if there is a herniated disc?". The answer to this depends mainly on the symptoms. For more than 90 percent of patients, conservative disc herniation treatment, i.e. therapy without surgery, is sufficient. This is especially true if the herniated disc causes pain or slight muscle weakness, but no other / more serious symptoms.
These include paralysis and disorders of the bladder or rectum function. In such cases, surgery is usually carried out. Surgical intervention can also be considered if the symptoms persist despite conservative treatment for at least three months.
Herniated disc: treatment without surgery
As part of conservative disc herniation treatment, the doctor now rarely recommends immobilization or bed rest. However, in the case of a herniated cervical disc, for example, it may be necessary to immobilize the cervical spine using a cervical collar. In the case of severe pain due to a herniated disc in the lumbar spine, a step bed position can be helpful for a short time.
In most cases, conservative disc herniation therapy involves light to moderate exercise. Normal everyday activities are - as far as the pain allows - advisable. Many patients also receive physiotherapy as part of outpatient or inpatient rehabilitation. For example, the therapist practices painless movement patterns with the patient and gives tips for everyday activities.
In the long term, too, regular exercise is very important in the case of a herniated disc: On the one hand, switching between loading and unloading the intervertebral discs promotes their nutrition. On the other hand, physical activity strengthens the core muscles, which relieves the intervertebral discs. Therefore, exercises to strengthen the back and abdominal muscles are highly recommended in the case of a slipped disc. Physiotherapists can show patients these exercises as part of a back school. Afterwards, the patients should exercise regularly themselves.
In addition, if you have a herniated disc, you can and should do sports, provided it is disc-friendly. This applies, for example, to aerobics, running, backstroke swimming, cross-country skiing and dancing. Tennis, downhill skiing, soccer, handball and volleyball, golf, ice hockey, judo, karate, gymnastics, canoeing, bowling, wrestling, rowing and squash are less good for the intervertebral discs.
Anyone who does not want to do without such a sport, which is damaging to the intervertebral discs, should do exercise and strength training to compensate, for example running, cycling or swimming regularly. In the event of uncertainty, patients should discuss the nature and extent of sporting activities with their doctor or physiotherapist.
Many people with back pain from a herniated disc (or any other reason) also benefit from relaxation exercises. These can help, for example, to relieve pain-related muscle tension.
Heat applications have the same effect. That is why they are also often part of conservative treatment for herniated discs.
If necessary, drugs are used for herniated discs. These include primarily pain relievers such as non-steroidal anti-inflammatory drugs (ibuprofen, diclofenac, etc.). In addition to a pain-relieving effect, they also have an anti-inflammatory and decongestant effect. Other active ingredients may also be used, such as COX-2 inhibitors and cortisone. They also have anti-inflammatory and analgesic effects. If the pain is very severe, the doctor can prescribe short-term opiates.
Pain therapy for herniated discs should be closely monitored by the doctor to avoid serious side effects. Patients should strictly follow the doctor's instructions when using pain relievers.
In some cases, the doctor will also prescribe muscle relaxing medication (muscle relaxants) because the muscles can become tense and hardened due to pain and a possible relieving posture. Sometimes antidepressants are also useful, for example for severe or chronic pain.
Physiotherapy for a herniated disc
Herniated disc: when do you have to operate?
The doctor and patient decide together whether a herniated disc operation should be performed. The criteria for a disc surgery are:
- Symptoms that indicate pressure on the spinal cord (surgery soon or immediately)
- severe paralysis or worsening paralysis (immediate surgery)
- Symptoms of pressure on the cauda equina (immediate surgery)
- decreasing pain and increasing paralysis (rapid operation because there is a risk that the nerve roots will already die)
There are various surgical techniques for treating a herniated disc. Microsurgical procedures are standard today. They reduce the risk of scarring. Alternatively, in certain cases, minimally invasive procedures for a herniated disc operation are possible.
Herniated Disc Surgery: Microsurgical Discectomy
The most widely used technique in the surgical treatment of a herniated disc is microsurgical discectomy (disc = disc, ectomy = removal). The affected intervertebral disc is removed with the help of a surgical microscope and the smallest of special instruments. This is supposed to relieve the spinal nerves that are constricted by the herniated disc and cause discomfort.
Only small incisions are required to insert the surgical instruments. This is why microsurgical operation technology is one of the minimally invasive procedures.
Microsurgical discectomy can remove all herniated discs - regardless of the direction in which the part of the disc slipped. In addition, the surgeon can see directly whether the distressed spinal nerve has been relieved of any pressure.
Course of the operation
Microsurgical discectomy is performed under general anesthesia. The patient is in a kneeling position with the upper body at a higher level on the operating table.This increases the distance between the vertebral arches and makes it easier to open the vertebral canal.
At the beginning, the surgeon makes a small skin incision over the diseased disc area. Then he carefully pushes the back muscles to the side and partially (as little as necessary) cuts into the yellowish ligament (ligamentum flavum) that connects the vertebral bodies. This allows the surgeon to look directly into the spinal canal with the microscope. Sometimes he also needs to remove a small piece of bone from the vertebral arch to improve vision.
With special instruments he now loosens the herniated disc tissue under visual inspection of the spinal nerve and removes it with grasping forceps. Larger defects in the fiber ring of the intervertebral disc can be sutured microsurgically. Disc parts (sequesters) that have slipped into the spinal canal can also be removed. In the last step of the intervertebral disc operation, the surgeon closes the skin with a few sutures.
Possible complications
Microsurgical disc surgery can injure the nerve that is to be relieved. Possible consequences are sensory and movement disorders of the legs, functional disorders of the bladder and intestines, and sexual disorders. Such complications are rare.
As with any operation, there is also a certain risk of anesthesia with this intervertebral disc operation, as well as the risk of infections, wound healing disorders and secondary bleeding.
Some of the patients experience pulling leg pain or a tingling sensation after weeks or months, even with optimal intervertebral disc surgery and removal of the incision. This late consequence is called "Failed back surgery syndrome".
After the operation
As with any operation under anesthesia, sometimes the bladder has to be emptied with a catheter on the first day after the operation. After a very short time, however, the bladder and bowel functions normalize. Usually the patient can get up on the evening of the day of the operation.
On the first day after the operation, physiotherapy exercises are started in the patient with a herniated disc. This should strengthen his muscles and ligaments again. Psychologists, nutritionists and occupational therapists also work as specialists in rehabilitation after a herniated disc operation.
The hospital stay usually only lasts a few days. The long-term success of the intervertebral disc operation is checked six or twelve months after the microsurgical discectomy. Imaging procedures help here.
Herniated Disc Surgery: Open Discectomy
Before the introduction of the surgical microscope, herniated discs were often operated on using the conventional open technique under a larger access (larger incisions). Today, open discectomy is rarely performed, for example in the case of malformations of the spine. Its results are comparable to those of microsurgical discectomy. However, serious complications are more common.
Course of the operation
The open discectomy is essentially the same as the microsurgical herniated disc operation, but larger incisions are made and the surgical area is not assessed with a micro-optic, but from the outside.
Possible complications
The possible complications of open discectomy are comparable to those of microsurgical discectomy, but occur more frequently.
After the operation
Sometimes the bladder has to be emptied with a catheter on the first day after the open disc surgery. The bladder and bowel functions return to normal within a very short time.
The patient is usually allowed to get up again on the evening of the day of the operation. Physiotherapy exercises are usually started the next day in order to strengthen the muscles and ligaments of the back again. The patient usually only has to stay in the hospital for a few days.
Herniated Disc Surgery: Endoscopic Discectomy
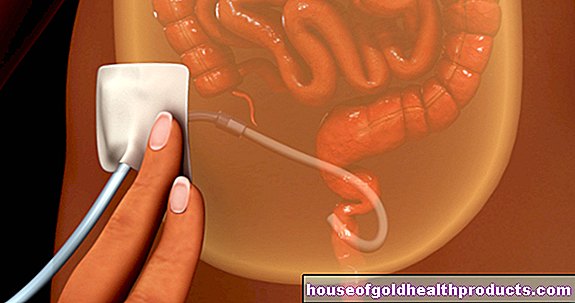
In addition to the microsurgical method, the minimally invasive techniques of disc surgery also include so-called percutaneous endoscopic methods. The intervertebral disc is removed here with the help of endoscopes, video systems and micro-instruments (some of which are motor-driven), which are inserted through small incisions in the skin. The patient is usually in a semi-awake state and under local anesthesia. This enables him to communicate with the surgeon.
Endoscopic herniated disc surgery cannot be performed on every patient. It is unsuitable, for example, if parts of the intervertebral disc have become detached (sequestered disc herniation) and have slipped up or down in the spinal canal. Endoscopic discectomy cannot always be used for herniated discs in the transition area between the lumbar spine and sacrum. Because here the iliac crest blocks the path of the instruments.
By the way: With endoscopic methods, not only can the entire intervertebral disc be removed (discectomy), but also only parts of the nucleus if necessary. Then one speaks of percutaneous endoscopic nucleotomy.
Course of the operation
The patient lies on his stomach during the endoscopic disc operation. The skin over the affected section of the spine is disinfected and locally anesthetized. One or two small metal tubes are pushed into the disc space through one or two small incisions under X-ray control. These are working sleeves with a diameter of three to eight millimeters. They allow instruments such as small grasping forceps and an endoscope to be inserted into the intervertebral disc space. The latter has special lighting and optics. The images from the operating area inside the body are projected onto a video monitor where the surgeon can see them.
The surgeon can now selectively remove intervertebral disc tissue that is pressing on a nerve. After the endoscopic disc operation, he sutures the incisions with one or two stitches or provides them with special plasters.
Possible complications
The complication rate in endoscopic disc surgery is relatively low. Even so, there is a certain risk of damaging nerves. Possible consequences are sensory and movement disorders in the legs as well as functional disorders of the bladder and intestines.
As with any operation, there is also the risk of infections, wound healing disorders and secondary bleeding.
Compared to microsurgical discectomy, the relapse rate (recurrence rate) is higher in endoscopic disc surgery.
After the operation
If the endoscopic disc operation went smoothly, the patient can get up again within three hours and leave the hospital on the same day or the next morning. Physiotherapy exercises should be started the day after the operation.
Intervertebral disc surgery with an intact fibrous ring
If someone only has a slight herniated disc in which the fibrous ring is still intact, the affected intervertebral disc in the area of the gelatinous nucleus can sometimes be reduced in size or shrunk by means of a minimally invasive procedure. This relieves the pressure on nerve roots or the spinal cord. This technique can also be used for protruding intervertebral discs (the fibrous ring is always intact here).
The advantage of minimally invasive interventions is that they only require small skin incisions, are less risky than open surgery and can usually be performed on an outpatient basis. However, they are only suitable for a small number of patients.
Course of the operation
In this minimally invasive disc operation, the skin over the affected spinal column is first disinfected and locally anesthetized. Sometimes the patient is also put into a twilight sleep. Now the doctor carefully pricks a hollow needle (cannula) into the center of the affected intervertebral disc under image control. He can insert working instruments through the hollow canal in order to reduce or shrink the tissue of the gelatinous nucleus:
This can be a laser, for example, which causes the gelatinous nucleus inside the intervertebral disc to vaporize with individual flashes of light (laser disc decompression). The gelatinous core consists of over 90 percent water. The evaporation of tissue reduces the volume of the core. In addition, the heat destroys "pain receptors" (nociceptors).
In the case of thermal lesions, the surgeon pushes a thermocatheter into the interior of the intervertebral disc under X-ray control. The catheter is heated up to 90 degrees Celsius, so that part of the intervertebral disc tissue boils off. At the same time, the heat should solidify the outer fiber ring. Part of the pain-conducting nerves is also destroyed.
In what is known as nucleoplasty, the doctor uses radio frequencies to generate heat and vaporize the tissue.
The doctor can also insert a decompressor through the cannula into the interior of the intervertebral disc. At its tip there is a rapidly rotating spiral thread. It cuts into the tissue and at the same time can suck out up to one gram of the gelatinous mass.
In chemonucleolysis, the enzyme chymopapain is injected, which chemically liquefies the gelatinous nucleus inside the intervertebral disc. After a certain waiting time, the liquefied core mass is sucked off through the cannula. It is very important here that the fibrous ring of the intervertebral disc in question is completely intact. Otherwise, the aggressive enzyme can escape and cause severe damage to surrounding tissue (such as nerve tissue).
Possible complications
One of the possible complications in minimally invasive disc operations is bacterial disc inflammation (spondylodiscitis). It can spread to the entire vertebral body. That is why the patient is usually given an antibiotic as a preventive measure.
After the operation
In the first few weeks after a minimally invasive disc operation, the patient should take some physical care. Sometimes the patient is prescribed a corset (elastic bodice) for relief during this period.
Herniated Disc Surgery: Implants
As part of the surgical disc herniation treatment, the worn disc is sometimes replaced with a prosthesis in order to preserve the mobility of the spine. The intervertebral disc implant is designed to maintain the distance between the vertebrae and their normal mobility, and to relieve pain.
So far it is unclear which patients will benefit from an intervertebral disc implant and what the long-term success will look like. Ongoing studies have so far produced positive results. However, there are still no real long-term results, especially since most patients are middle-aged at the time of the intervertebral disc operation, so they probably still have a long time to go.
Nucleus pulposus replacement
In the early stage of intervertebral disc wear (intervertebral disc degeneration), it is possible to replace or support the gelatinous core of the intervertebral disc (nucleus pulposus). Doctors usually use hydrogel pillows as a kind of artificial gelatinous core. This gel comes very close to the biochemical and mechanical properties of the natural gelatinous core because it can absorb liquid. Like the intervertebral disc, it absorbs water when it is relieved and releases it again when it is exerted.
Depending on the extent of the findings and depending on the procedure, a local or short anesthetic is often sufficient for this intervertebral disc operation. The hydrogel is usually introduced using a hollow needle (under X-ray view). Affected people can often get up on the same day and move freely the next day. The process is being further developed and monitored in clinical studies around the world. Little is known about long-term results.
Total replacement of the intervertebral disc
With total disc replacement, the intervertebral disc and parts of the base and cover plates of the adjacent vertebrae are removed. In most models, the intervertebral disc replacement consists of titanium-coated base and cover plates and a polyethylene inlay (very similar to the well-known hip prostheses).
The procedure for the intervertebral disc operation: The old intervertebral disc is removed; In addition, part of the cartilage on the base and cover plates of the adjacent vertebrae is rasped away. With the help of fluoroscopy, the size of the intervertebral disc is determined and a suitable implant is selected. Depending on the model, the surgeon now chisels a small, vertical slot in the base and cover plates of the adjacent vertebrae. It serves to anchor the prosthesis. Then the surgeon installs the disc replacement. The pressure of the spine stabilizes the implant. Within three to six months, bone material grows into the specially coated base and cover plates of the full disc prosthesis.
The patient can get up on the first day after the operation. In the first few weeks he is not allowed to lift heavy loads and must avoid extreme movements. An elastic bodice that the patient can put on himself is used for stabilization.
Patients who suffer from osteoporosis (bone loss) or who have unstable movements in the vertebrae to be treated must not receive a total disc replacement.
Herniated Disc: Causes and Risk Factors
If an intervertebral disc - the shock absorber between two vertebrae - slips, the inner gelatinous core of the intervertebral disc slips. The tough, fibrous covering (annulus fibrosus) of the intervertebral disc tears and the nucleus jelly emerges. It can press on the nerves (spinal nerves) originating in the spinal cord and cause discomfort. Sometimes detached parts of the gelatinous nucleus slide into the spinal canal. Then the diagnosis is “sequestered disc herniation”.
Herniated disc - the different forms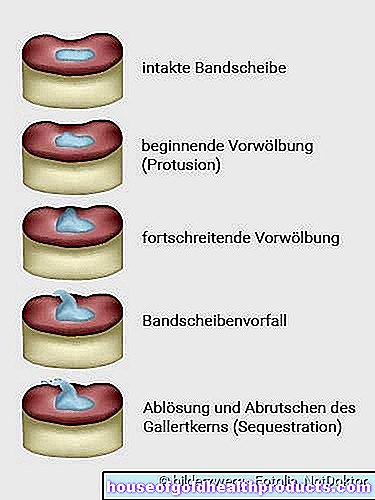
The cause of a herniated disc is usually an age-related and stress-related degeneration of the connective tissue ring of the intervertebral disc: It loses its stabilizing function and tears under great stress. Some of the gelatinous nucleus can leak out and press on a nerve root or the spinal cord. The frequency of herniated discs decreases again from the age of 50, because the nucleus then loses more and more fluid and therefore leaks less often.
In addition, sedentary lifestyle and obesity are important risk factors for herniated discs. Typically, the abdominal and back muscles are then also weak. Such instability of the body promotes incorrect loading of the intervertebral discs, since only strong trunk muscles relieve the spine.
Possible triggers of a herniated disc are posture errors, jerky movements and sports in which the spine is shaken (riding, mountain biking) or twisted (tennis, squash). The same goes for heavy physical labor such as lifting heavy loads. However, this alone cannot cause a herniated disc. This can only happen if a disc is already showing signs of wear and tear.
Injuries (e.g. from falling stairs or traffic accidents) and congenital misalignments of the spine are less common causes of a herniated disc.
In some people, a congenital weakness of the connective tissue contributes to the development of a herniated disc.
The disc protrusion (disc protrusion) must be distinguished from the herniated disc (disc prolapse). Here the inner intervertebral disc tissue shifts outward without the annulus of the intervertebral disc tearing. Nevertheless, complaints such as pain and sensory disturbances can occur. A well-known example is lumbago (lumbago): This refers to acute shooting, severe pain in the lumbar vertebrae.
Herniated disc: cervical spine
Age-related wear and tear on vertebral joints and intervertebral discs is the main reason why the cervical spine can have a herniated disc, especially in older people: the vertebral joints loosen and change over the years, and the intervertebral discs wear down increasingly.
The effects of a herniated disc in the cervical spine mostly affect the shoulders, arms and the chest area because the nerves supplying it leave the spinal cord at this height.
When younger people have a herniated cervical disc, the cause is often an injury or an accident. For example, turning the head abruptly can cause a disc to herniate between the cervical vertebrae.
Read more about the causes, symptoms and treatment of a cervical disc prolapse in the article Slipped disc cervical spine.
Herniated disc: disease course and prognosis
In around 90 out of 100 patients, the pain and restricted mobility that an acute herniated disc causes subside within six weeks. Presumably, the displaced or exuded intervertebral disc tissue is removed from the body or shifts, so that the pressure on the nerves or spinal cord decreases.
If treatment is necessary, conservative measures are usually sufficient. They are therefore often the therapy of choice for a herniated disc. The duration of regeneration and the chances of recovery depend on the severity of the herniated disc.
Even after successful treatment, a new incident can occur on the same disc or between other vertebral bodies.Therefore, anyone who has survived a herniated disc should train their core muscles regularly and take further advice to heart to prevent a herniated disc (see below).
After an operation
An operation for a herniated disc should be carefully considered. Often it is successful, but there are always patients for whom the procedure does not bring the desired freedom from pain in the long term. Doctors speak of failed-back surgery syndrome or post-discectomy syndrome. It arises from the fact that the procedure has not eliminated the actual cause of the pain or has created new causes of the pain. This can be, for example, inflammation and scarring in the surgical area.
As a further complication of an intervertebral disc operation, nerves and vessels can be damaged during intervention.
For various reasons, a patient may feel worse after a disc surgery than before. Follow-up operations may also be necessary. This can also be the case if later herniated discs occur again in the operated patient.
A herniated disc should therefore only be operated on if it is urgently necessary, for example because it causes paralysis. In addition, the expected benefit should be significantly greater than the risks. In order to improve the results, many patients stay in rehab clinics after the operation.
So far there is no way to find out in advance which patients with a herniated disc will benefit most from an intervertebral disc operation.
Herniated Disc: Prevention
Healthy, strong core muscles are the prerequisite for the body to be able to cope with everyday challenges. If you follow a few rules, you can do something about a herniated disc. Preventive measures include:
- Pay attention to your body weight: being overweight puts a strain on the back and promotes a herniated disc.
- Exercise regularly: Hiking, jogging, cross-country skiing, crawling and backstroke swimming, dancing, water aerobics and other types of gymnastics that strengthen the back muscles are particularly beneficial for your back.
- Certain relaxation techniques such as yoga, tai chi, and pilates also promote good posture and help strengthen your core and back. This is the best relief for the spine and intervertebral discs.
- If possible, sit upright in a normal high chair. Change your sitting position often. Accompanying strength training stabilizes the core muscles.
- Position objects that you use often at an easily accessible height: the eyes and arms are relieved and you prevent overloading the cervical spine. This is also important in a back-friendly workplace.
- Avoid deep and soft seating; A wedge-shaped seat cushion is recommended.
- Working while standing: The workplace must be high enough that you can (permanently) stand upright.
- Never lift very heavy objects with your legs straight and your spine bent: bend your knees, keep your spine straight and lift the load "out of your legs".
- Distribute the load in both hands so that the spine is evenly stressed.
- Do not bend your spine towards the opposite side when carrying loads.
- When carrying loads, keep your arms close to your body: do not shift your weight backwards and avoid a hollow back.
- Make sure that the spine cannot kink while sleeping. It makes sense to have a good mattress (the hardness should correspond to the body weight) plus a slatted frame and possibly a small pillow to support the natural shape of the spine.
People who have already had a herniated disc should also adhere to this advice.
Additional information
Books
- Intervertebral disc disease - What to do ?: With the best exercises for everyday life (Paul Th. Oldenkott et al., 2013, Goldmann Verlag)
Guidelines
- S2k guideline "Conservative and rehabilitative care for herniated discs with radicular symptoms" of the German Society for Orthopedics and Orthopedic Surgery (DGOOC) (status: 2014)
- S2k guideline "Lumbar radiculopathy" of the German Society for Neurology (as of 2012)
- S1 guideline "Cervical Radiculopathy" of the German Society for Neurology (as of 2012)


.jpg)


.jpg)